- What are the Factors Driving the Growth of the Healthcare API Market?
- Regulatory Push for Interoperability
- Rise of Consumer-Centric Care
- Growth of Value-Based and Remote Care Models
- Cloud Transformation and Agile Infrastructure
- Demand for Automation and Workflow Optimization
- Ecosystem Collaboration and Platformization
- How APIs are Improving Efficiency in Healthcare?
- Service-Level Impact of Healthcare APIs
- Application-Level Efficiency Gains Across Stakeholders
- How are Technological Advancements Boosting Healthcare API Adoption?
- 1. FHIR Maturity and Standardization
- 2. Cloud-Native Infrastructure
- 3. AI and Data Layer Integration
- 4. Interoperability and API Marketplaces
- 5. Focus on Cybersecurity and Compliance
- Key Considerations When Designing an API-First Strategy in Healthcare
- 1. Compliance with Regulatory Frameworks
- 2. Role-Based Access and Consent Management
- 3. Data Normalization and Clinical Standardization
- 4. Auditability and Data Lineage
- 5. Scalability and Resilience by Design
- 6. Developer Experience and Ecosystem Readiness
- 7. Security as a Foundation, Not an Afterthought
- API Monetization in Healthcare - From Cost Center to Revenue Driver
- 1. API-as-a-Product Strategy in Healthcare
- 2. Joining API Marketplaces and Developer Hubs
- 3. White-Labeled Integration Services for Vendors
- 4. Enabling Value-Based Partnerships
- 5. Accelerating Time-to-Value for HealthTech Startups
- Why Appinventiv is the Right Healthcare API Development Partner?
- FAQs
Key takeaways:
- Strategic Asset: Healthcare APIs drive data exchange, care coordination, and digital transformation.
- Regulatory Push: Mandates like the 21st Century Cures Act and HL7 FHIR enforce API adoption.
- Patient-Centric: APIs enable apps to integrate appointments, test results, and wearable data.
- Cloud Integration: APIs connect scalable cloud systems for telehealth and AI diagnostics.
- Automation: APIs streamline claims and prior authorizations, reducing costs.
- EHR Access: APIs expedite diagnostics with instant access to health records.
- Remote Monitoring: APIs integrate wearable data for proactive care.
- Monetization: APIs generate revenue via marketplaces and white-labeled services.
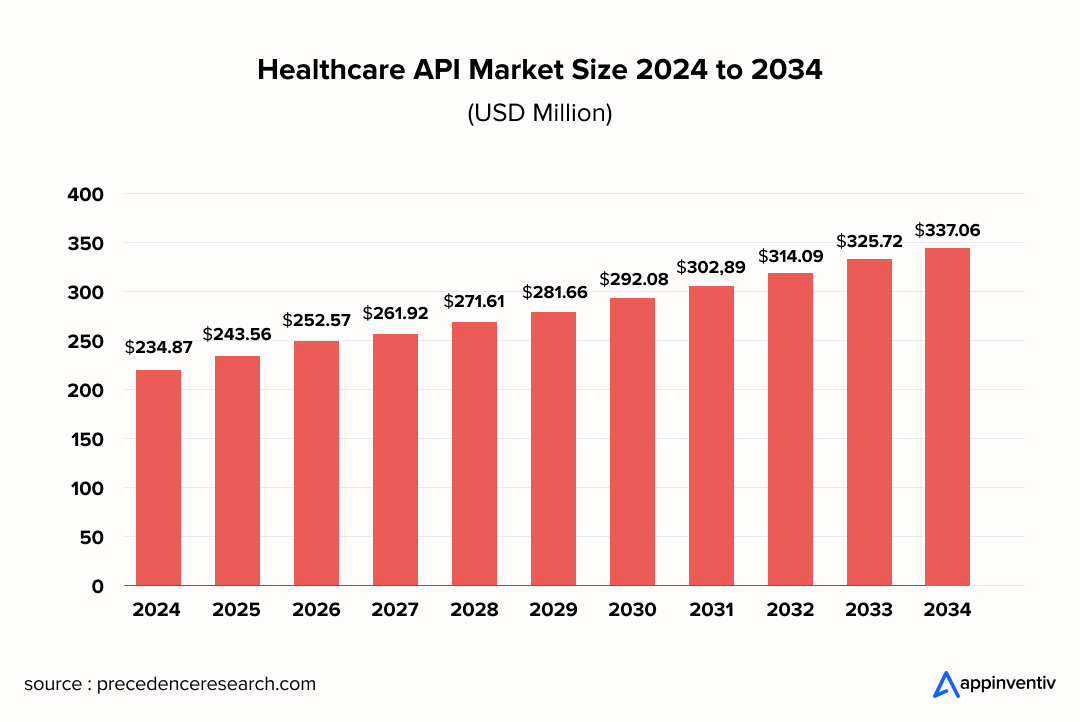
In an industry where data fragmentation, regulatory compliance, and care coordination are daily challenges, Healthcare APIs (Application Programming Interfaces) are no longer just a technical enabler; they’re a strategic imperative. From enabling real-time data exchange between Electronic Health Records (EHRs) and diagnostic platforms to powering patient-facing mobile applications, APIs in healthcare have redefined how organizations interact with their internal systems, external partners, and patients.
Driven by federal mandates, such as the 21st Century Cures Act, and interoperability standards like HL7 FHIR (Fast Healthcare Interoperability Resources), the role of Application Programming Interfaces (APIs) in healthcare has evolved beyond simple integration. Today, they function as foundational assets that drive innovation, operational agility, and digital transformation.
Health systems, payers, digital health startups, and even medical technology companies are increasingly leveraging APIs to accelerate the time-to-market for new offerings, personalize care experiences, and unlock new revenue streams.
This article explores how healthcare APIs, when aligned with core business strategy, can move the needle from regulatory compliance to a competitive advantage. From API-first architectures to monetization models, the sections ahead outline the emerging trends, use cases, and considerations for making healthcare APIs for business growth a cornerstone of digital health leadership.
For many enterprises, the next step is understanding how these API strategies support real generative AI in healthcare applications, from automated documentation to virtual assistants
Partner with a team that understands healthcare inside out.
What are the Factors Driving the Growth of the Healthcare API Market?
The growth of the APIs integration in healthcare is being shaped by a confluence of clinical, regulatory, and technological shifts, each demanding faster, more secure, and patient-centric data exchange. These drivers are not only fueling innovation across care delivery models but also influencing the strategic roadmap of providers, payers, and digital health vendors alike.
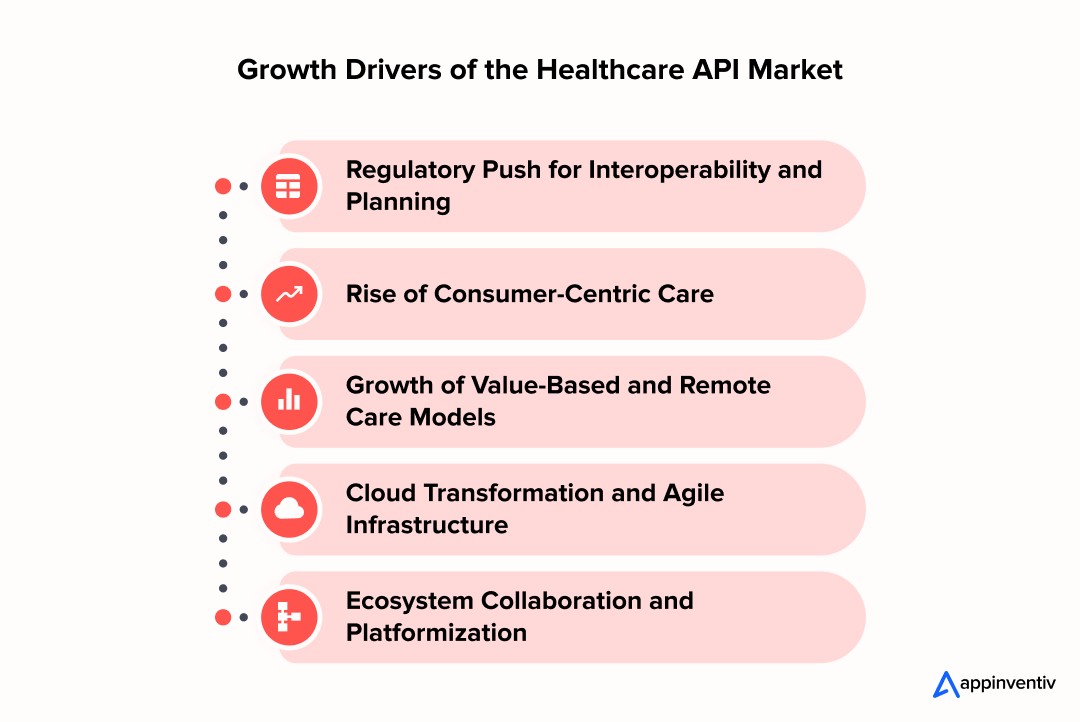
Regulatory Push for Interoperability
Landmark regulations, such as the 21st Century Cures Act and CMS’s Interoperability and Patient Access Rule, have compelled the healthcare ecosystem to reconsider siloed architectures. APIs – particularly those built on HL7 integration, FHIR standards – are at the core of these mandates, enabling EHR access services that allow patients, providers, and third-party developers to retrieve and securely share health data in real-time.
Rise of Consumer-Centric Care
Patients are increasingly behaving like digital consumers, expecting personalized, seamless, and mobile-first experiences. APIs healthcare implementation strategy is critical to delivering such experiences, whether it’s booking appointments, accessing test results, or integrating wearable healthcare device data into patient portals. This shift is accelerating the demand for patient-facing, API-driven innovation in healthcare, applicable to both provider and payer environments.
Growth of Value-Based and Remote Care Models
Healthcare’s transition from volume to value requires access to longitudinal data, care coordination across teams, and real-time monitoring, especially for chronic care and post-acute management. The benefits of APIs integration in healthcare lie in the fact that it supports remote patient monitoring services by enabling continuous data flow from wearables and IoT medical devices into provider workflows, helping close care gaps and reduce readmissions.
Cloud Transformation and Agile Infrastructure
As healthcare organizations shift from legacy on-premise systems to more scalable and agile cloud-based deployments, APIs are serving as the glue that connects modular systems. They enable organizations to innovate incrementally by integrating telehealth platforms, AI-based diagnostics, or third-party billing services without disrupting existing infrastructure.
Bonus Read: How Is Google Cloud Health Api Powering Healthcare?
Demand for Automation and Workflow Optimization
Administrative overhead, from prior authorizations to payment processing, remains a massive pain point. The role of APIs in healthcare lies in enabling automation across revenue cycle operations, including payment services and the integration of claims data. For payers and vendors, secure healthcare APIs architectures support scalable, reusable microservices that streamline backend operations and reduce time-to-market for new solutions.
Ecosystem Collaboration and Platformization
The line between traditional healthcare entities and tech players is blurring. API-driven healthcare solutions allow vendors, med-tech OEMs, and digital health startups to build platform ecosystems where services, from scheduling to clinical decision support, can be consumed via plug-and-play interfaces. This is fostering a new wave of vendor and B2B end-use cases, where APIs are not just enablers but products in their own right.
Bonus Read: API Development Guide: Build, Test, Deploy like a Pro
How APIs are Improving Efficiency in Healthcare?
Efficiency in healthcare isn’t just about speed; it’s about precision, accessibility, and coordination across an increasingly complex care ecosystem. Healthcare APIs are central to this transformation, enabling services and applications that automate workflows, improve data fluidity, and elevate the quality of care. Below, we explore how specific API-enabled services and their applications across key stakeholders are delivering measurable efficiency gains.
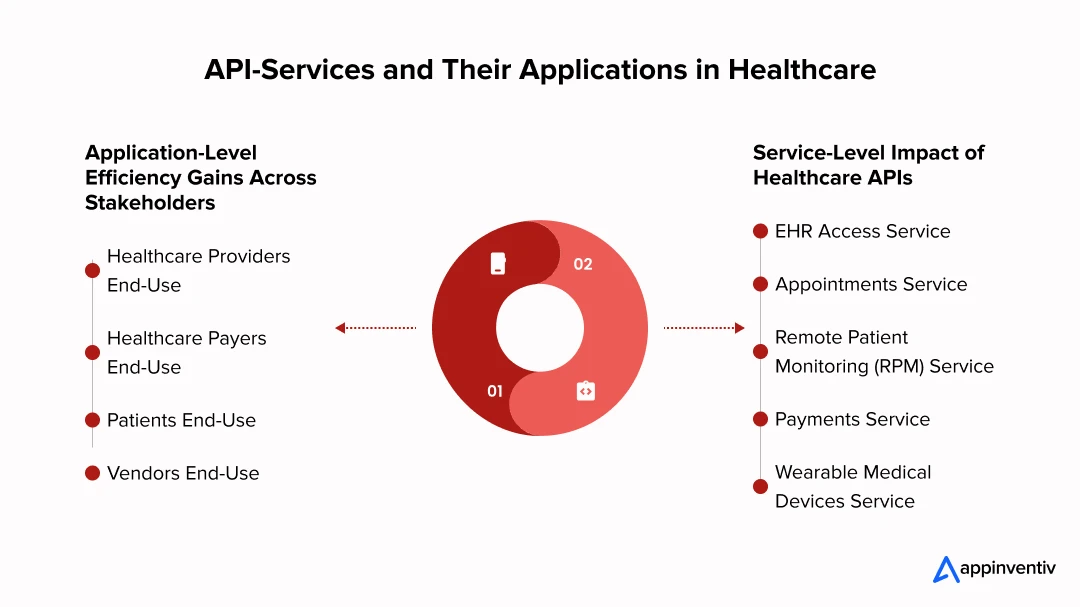
Service-Level Impact of Healthcare APIs
Application Programming Interfaces in healthcare are streamlining traditionally fragmented services – transforming everything from how data is accessed to how care is delivered, monitored, and reimbursed.
EHR Access Service
One of the benefits of APIs integration in healthcare can be seen in how it accesses clinical data from electronic health records, reducing the burden on providers and IT teams. Instead of toggling across multiple platforms or waiting for faxed records, clinicians can retrieve up-to-date patient histories instantly. This accelerates diagnostics, improves handoffs across specialties, and cuts down administrative lag.
These gains depend heavily on robust EHR interoperability that ensures consistent access across systems.
Appointments Service
APIs integrate scheduling systems with patient portals and third-party tools, reducing no-shows, overbooking, and manual coordination. Providers benefit from optimized resource allocation, while patients experience improved self-service and transparency.
Remote Patient Monitoring (RPM) Service
APIs connect wearables and home-based devices to provider systems, enabling passive, continuous health tracking. This allows clinicians to intervene early, particularly in the management of chronic diseases, while reducing hospital admissions and in-person follow-ups.
Payments Service
By integrating APIs into billing and revenue cycle systems, payers and providers can automate claims submission, eligibility checks, and remittance advice. This reduces billing errors, accelerates reimbursement, and improves patient financial transparency.
Wearable Medical Devices Service
APIs facilitate the flow of real-time biometric data from FDA-approved wearable devices into clinical decision-making systems. This not only empowers personalized care plans but also enriches datasets for population health analytics and precision medicine initiatives.
Application-Level Efficiency Gains Across Stakeholders
Across providers, payers, patients, and vendors, APIs are eliminating inefficiencies by enabling real-time data flow, seamless integrations, and more connected digital health experiences.
Healthcare Providers End-Use
Providers leverage APIs to reduce documentation time, support clinical decision-making, and ensure seamless data interoperability across departments and locations. The result is faster diagnosis, fewer errors, and more face time with patients.
Bonus Read: Guide For Clinical Mobility Solution
Healthcare Payers End-Use
Payers use APIs to streamline member onboarding, automate claims adjudication, and integrate with external health apps for better risk profiling. APIs also facilitate real-time data exchange with providers, enabling faster prior authorizations and more dynamic care coordination.
Patients End-Use
Patients benefit from API-enabled apps that provide one-stop access to their records, test results, prescriptions, and appointment scheduling, as well as quickly accessing billing information through AI in medical billing. This not only enhances engagement but also reduces the dependency on call centers and in-person visits for routine queries.
Vendors End-Use
Digital health vendors and solution providers utilize APIs to integrate their services into larger health systems without incurring costly custom integrations. Whether it’s integrating a decision support tool with an EHR or syncing wearable data with a payer dashboard, APIs reduce deployment timelines and simplify updates.
How are Technological Advancements Boosting Healthcare API Adoption?
As healthcare organizations embrace digital transformation, emerging technologies are not just integrating APIs into healthcare workflow; they’re accelerating their adoption and redefining what APIs can achieve. The convergence of cloud, AI, FHIR, and cybersecurity innovations is enabling API ecosystems that are more scalable, secure, and clinically intelligent than ever before.
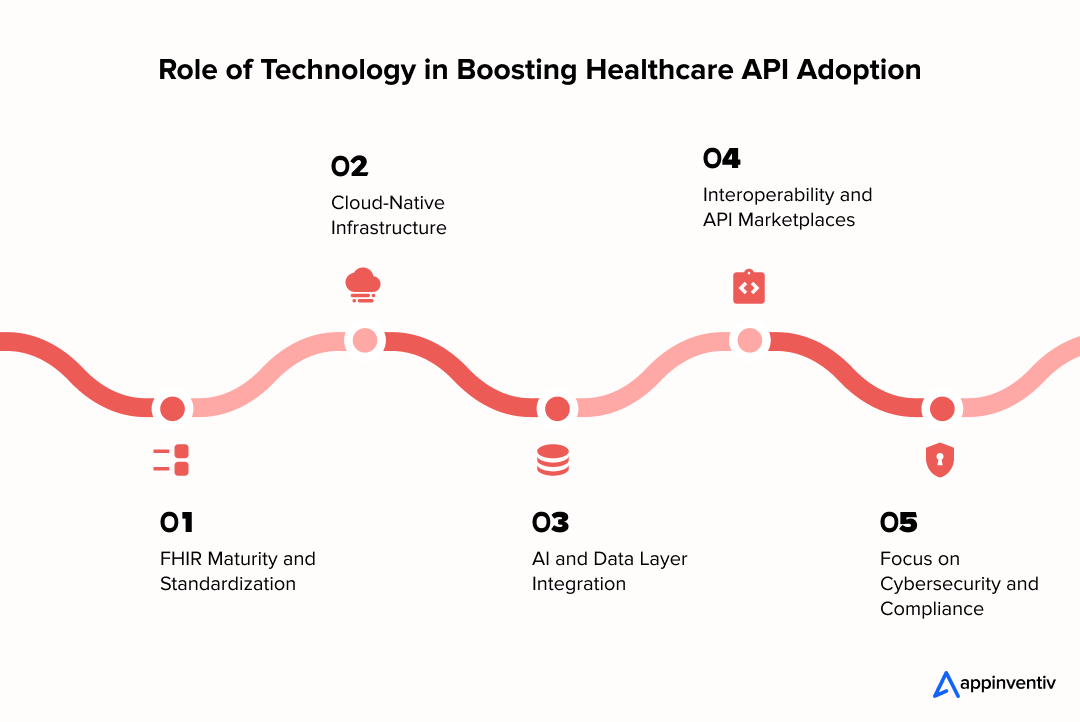
1. FHIR Maturity and Standardization
The evolution of HL7 FHIR from a compliance framework to a developer-friendly standard has significantly lowered the technical barrier to building APIs. Its resource-based architecture allows the role of APIs in healthcare to expand, enabling the modeling of clinical concepts, such as medications, encounters, or lab results, using a consistent, modular format. As a result, EHR access services are becoming more reliable, standardized, and future-proof.
2. Cloud-Native Infrastructure
Cloud-based deployments are dramatically reducing time-to-deployment and total cost of ownership for API-driven healthcare solutions. Providers and vendors are leveraging serverless architectures, containerization (e.g., Docker, Kubernetes), and managed API gateways to scale their services elastically and securely. This flexibility is especially critical for remote patient monitoring and real-time data-intensive use cases.
3. AI and Data Layer Integration
Advanced APIs are increasingly embedded with AI-powered services, such as natural language processing, image recognition, and predictive analytics. For example, APIs can extract structured data from unstructured clinical notes, flag abnormal trends in wearable data, or suggest billing codes using ML in healthcare. These “intelligent APIs” go beyond access—they drive action.
4. Interoperability and API Marketplaces
API marketplaces and interoperability platforms are transforming how healthcare entities discover, integrate, and monetize APIs. These hubs enable hospitals, payers, and health tech vendors to rapidly adopt third-party services, from appointment scheduling to prior authorization, without needing to build them from scratch. It’s accelerating innovation while maintaining governance.
5. Focus on Cybersecurity and Compliance
As API usage grows, so does the risk surface. Modern healthcare APIs now integrate OAuth2.0, OpenID Connect, and JWT-based tokenization to ensure secure access and granular control. Zero Trust frameworks, data encryption standards (e.g., TLS 1.3), and real-time threat monitoring are being baked directly into API management layers, helping meet HIPAA and HITRUST requirements.
Bonus Read: Advantages of Data Encryption Technology
Key Considerations When Designing an API-First Strategy in Healthcare
Adopting an API-first approach in healthcare isn’t simply about exposing endpoints; it’s about creating a secure, scalable, and governed ecosystem that respects the clinical, operational, and regulatory nuances of the industry.
Whether you’re a provider, modernizing a legacy system in healthcare, or a vendor launching an interoperability-driven product, these considerations are central to successful and secure healthcare APIs strategy execution.
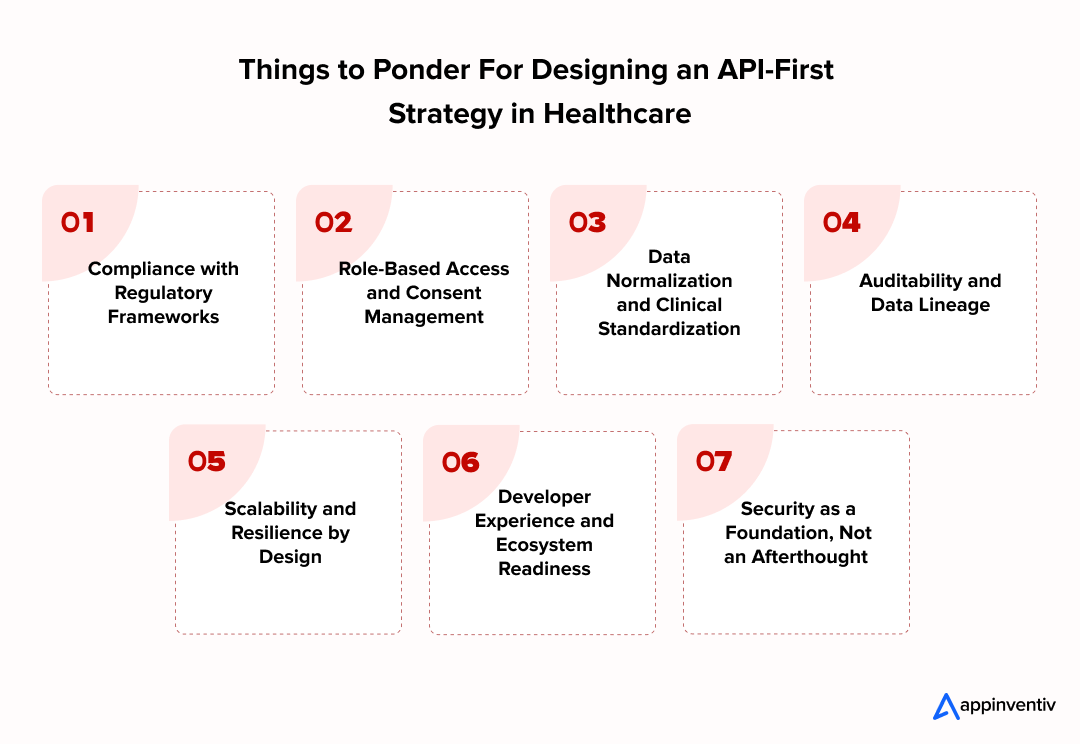
1. Compliance with Regulatory Frameworks
One of the sureshot factors driving the growth of the healthcare API market is that every healthcare or medical supply delivery must prioritize HIPAA, the 21st Century Cures Act, CMS’s interoperability mandates, and ONC’s API Certification Criteria. Beyond protecting PHI, compliance ensures eligibility for federal programs and smooth integration with a certified EHR system. This requires embedding compliance logic at the API level – encryption, audit trails, and token-based access, not just at the application layer.
Bonus Read: Guide to Build ERS System
2. Role-Based Access and Consent Management
Access control in healthcare is rarely a binary decision. APIs must enforce role-based access based on user identity (e.g., clinician, patient, insurer) and context (e.g., treatment, payment, operations). Furthermore, patient consent must be actively tracked and enforced across endpoints, whether it’s for data sharing with third-party apps or internal transitions of care.
3. Data Normalization and Clinical Standardization
Integrating data from multiple systems often means handling different formats, vocabularies, and timestamp logic. APIs built using HL7 FHIR and terminology standards, such as SNOMED CT, LOINC, and RxNorm, help normalize inputs and outputs, ensuring a clean and consistent data flow that EHRs, payer platforms, and analytics tools can consume without reconciliation bottlenecks.
4. Auditability and Data Lineage
In healthcare, every API call could have downstream clinical, legal, or billing implications. APIs must generate complete, immutable logs that capture the who, what, when, and why of each data interaction. This auditability is not only a HIPAA safeguard, it’s also essential for resolving clinical disputes, debugging integration errors, and enabling retrospective analytics.
5. Scalability and Resilience by Design
Peak surges, such as vaccine drives or flu season, test the limits of healthcare infrastructure. APIs healthcare implementation strategy must be built for elasticity, using scalable cloud services, auto-scaling rules, and asynchronous processing queues where appropriate. High availability, timeout management, and graceful degradation strategies must be defined early in the architecture.
6. Developer Experience and Ecosystem Readiness
The fastest way to slow down an API driven innovation in healthcare is by overlooking the developer experience. Clean documentation, SDKs, test sandboxes, example payloads, and CI/CD pipelines streamline development efficiency, making it easier for in-house teams or vendor partners to integrate rapidly. Both internal and external stakeholders should find your APIs discoverable, testable, and versioned with backward compatibility.
7. Security as a Foundation, Not an Afterthought
APIs integration in healthcare is a high-value target for attackers. TLS encryption, OAuth 2.0 flows, access tokens with short expiries, anomaly detection, rate limiting, input validation, and third-party risk management must all be embedded from the start. Frameworks like Zero Trust should guide how identity, context, and device posture influence access, especially for mobile and remote endpoints. AI TRiSM to manage and secure AI systems.
API Monetization in Healthcare – From Cost Center to Revenue Driver
As APIs mature from internal plumbing to strategic infrastructure, healthcare organizations are discovering new revenue opportunities by exposing their APIs as products. What began as a means to achieve interoperability is something that a healthcare software development company (and the industry) is now evolving into a platform strategy, where data access, services, and capabilities are offered to partners, developers, and even competitors via commercialized APIs.
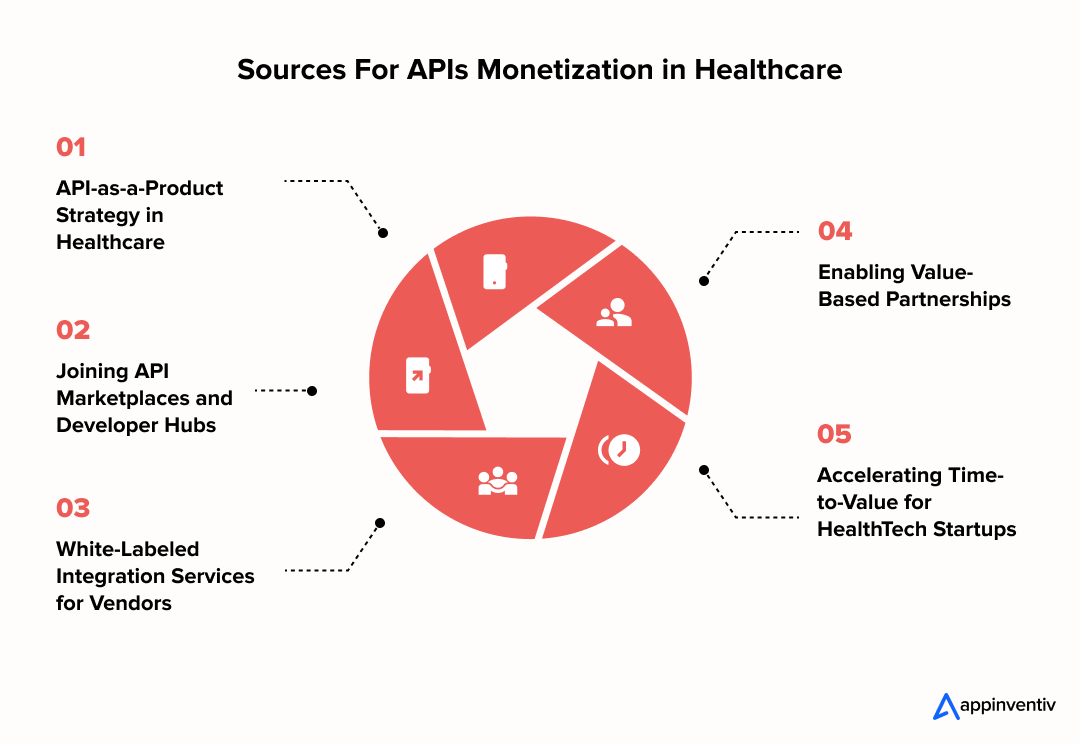
1. API-as-a-Product Strategy in Healthcare
Forward-thinking providers and payers are packaging APIs, such as eligibility checks, provider directories, claims status, or clinical data access, as standalone products. These are offered to digital health startups, research institutions, and employer health platforms under usage-based or subscription-based models, proving to be an excellent source of API monetization in healthcare.
2. Joining API Marketplaces and Developer Hubs
By listing APIs on healthcare-specific API marketplaces and interoperability hubs, organizations can generate revenue through increased visibility and reuse. For instance, an RPM service API or lab result-sharing API can be licensed to third-party virtual care platforms looking to accelerate go-to-market timelines.
3. White-Labeled Integration Services for Vendors
Some health systems are offering white-labeled API layers or integration middleware as a service to digital health vendors, positioning themselves as key providers of cost-reduction strategies utilizing healthcare APIs. This not only generates income but also strengthens control over data sharing and security across third-party applications.
4. Enabling Value-Based Partnerships
Exposed APIs can support value-based care models by integrating performance-based analytics, real-time quality metrics, and patient-reported outcomes into partner systems. Healthcare API business models become monetizable assets when tied to measurable improvements in care coordination, adherence, or reimbursement accuracy.
5. Accelerating Time-to-Value for HealthTech Startups
Health API providers are entering strategic partnerships with early-stage healthcare tech startups that need compliant, prebuilt services. In exchange, they negotiate revenue shares, data insights, or exclusive platform access, turning healthcare APIs for business growth into venture-aligned assets.
Bonus Read: 17 Innovative Healthcare Tech Startup Ideas
Why Appinventiv is the Right Healthcare API Development Partner?
Healthcare API development requires more than technical skill; it demands a deep understanding of clinical workflows, regulatory compliance, payer-provider dynamics, and patient privacy.
At Appinventiv, a bespoke healthcare app development company, we bring all of that together in your healthcare API business model. Our teams are well-versed in HIPAA, HL7 FHIR, the 21st Century Cures Act, and CMS interoperability mandates, ensuring your APIs are not only functional but fully compliant from day one.
We’ve worked with hospitals, payers, digital health startups, and medtech vendors to build scalable Application Programming Interfaces in healthcare ecosystems that integrate with major EHR systems like Epic, Cerner, Athenahealth, and others. Whether it’s EHR access, appointment scheduling, remote patient monitoring, or wearable device integration, our solutions are designed to meet the evolving needs of providers, payers, and patients alike.
Beyond app development, our healthcare software development company helps organizations shape their API strategy, covering consent management, data standardization, security infrastructure, and even monetization models. Our cloud-native architecture and DevSecOps approach ensure that your APIs are performant, scalable, and secure across environments.
When you partner with Appinventiv, you’re not just hiring a tech team; you’re gaining a healthcare innovation partner that understands how APIs can create real, measurable business value.
FAQs
Q. How do APIs work in healthcare?
A. APIs in healthcare act as secure intermediaries that allow different software systems like electronic health records (EHRs), lab systems, patient apps, and billing platforms – to communicate with each other in real time. Using industry standards such as HL7 FHIR, APIs allow for structured, permissioned data sharing. They ensure that data flows seamlessly between stakeholders while adhering to strict privacy and access controls.
Q. What are APIs used for in healthcare?
A. APIs are used across the healthcare ecosystem to enable core digital functions. These include accessing EHR data, booking appointments, exchanging lab results, processing claims, enabling remote patient monitoring, integrating wearable health data, and powering mobile health apps. They serve patients, providers, payers, and vendors alike – each relying on APIs to enable faster, more informed, and automated workflows.
Q. How are APIs improving efficiency in healthcare?
A. Integrating apis into healthcare workflow improves efficiency by automating manual tasks, reducing redundancies, and enabling real-time access to critical data. For example, appointment APIs eliminate scheduling bottlenecks, while EHR access APIs allow clinicians to retrieve patient history without delays. APIs also power backend operations like claims adjudication or inventory management, allowing care teams to focus on delivery instead of administration.
Q. What are some common healthcare API examples used in the industry?
A. Healthcare API examples include FHIR (Fast Healthcare Interoperability Resources) APIs for standardized data exchange, EHR (Electronic Health Record) APIs like those from Epic or Cerner for accessing patient records, and telehealth APIs like Doxy.me for virtual care integration. These APIs enable seamless data sharing and interoperability across healthcare systems.
Q. How do healthcare APIs improve patient experience?
A. By enabling services like digital appointment booking, on-demand access to medical records, personalized treatment updates, and remote monitoring, APIs in healthcare help patients stay engaged and informed. They reduce wait times, increase transparency, and give patients more control over their care journeys – ultimately improving satisfaction and health outcomes.
Q. How do healthcare APIs drive business innovation?
A. APIs unlock innovation by making healthcare systems more modular and flexible. Organizations can experiment with new features, integrate external platforms, and scale digital services quickly. Whether it’s launching a virtual care platform, connecting to a pharmacy network, or building predictive care models, APIs in healthcare shorten development cycles and reduce integration complexity, making it easier to innovate without overhauling core systems.
Q. Why are healthcare APIs considered the future of digital health businesses?
A. As the industry moves toward consumer-centric care, value-based models, and nationwide interoperability, APIs are becoming foundational to digital health strategy. They enable organizations to adapt faster, partner more broadly, and personalize care at scale. For digital health businesses, APIs are no longer just technical infrastructure – they are strategic levers for growth, compliance, and differentiation.
Q. How are technological advancements boosting healthcare API adoption?
A. Cloud computing, AI, IoT, and blockchain are enhancing what Application Programming Interfaces in healthcare does. Modern APIs can now process real-time data from wearables, support AI-driven diagnostics, enable blockchain-based audit trails, and scale instantly in cloud-native environments. These technologies are not just accelerating adoption, they’re expanding the possibilities of what APIs can achieve across care delivery, operations, and research.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

Change Management in Healthcare: Principles, Processes, and Models
Key Takeaways Change in healthcare fails quietly when ownership, workflow alignment, and follow-through are missing. Successful change management in healthcare focuses on adoption, not just system implementation. Clinical workflows and workforce capacity determine whether transformation sticks or stalls. Governance, clear accountability, and post-go-live support matter more than the model used. Sustainable healthcare transformation depends on…
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…