- Why Patient Management Software is a Strategic Investment: Market Insights
- Key Benefits of Patient Management Software
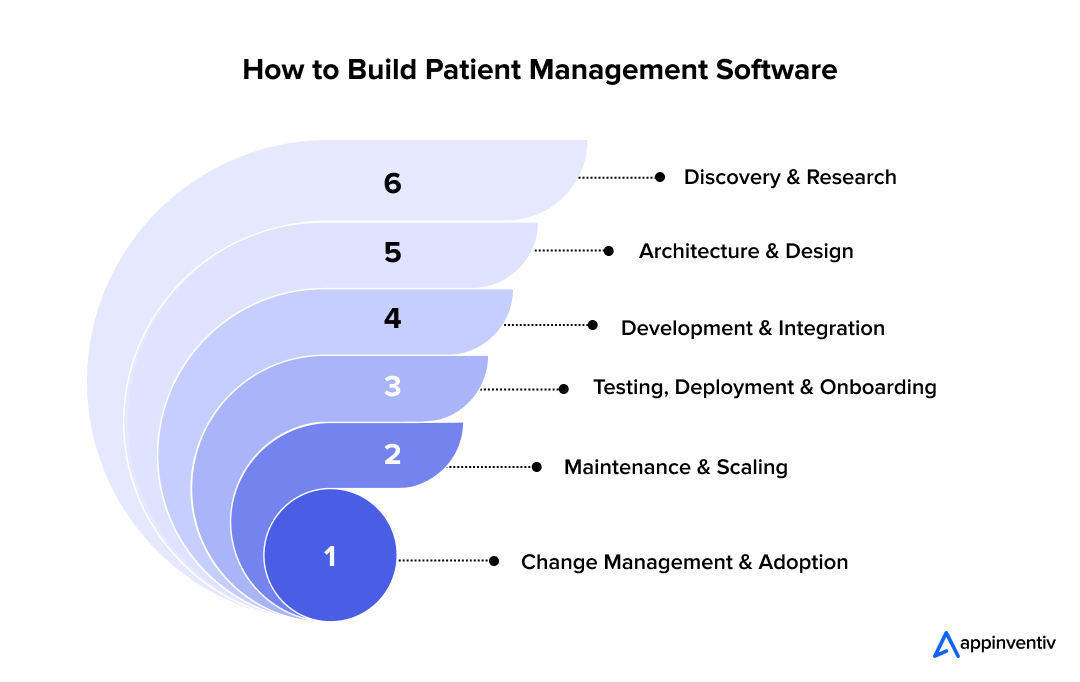
- How to Build Patient Management Software?
- 1. Discovery & Research
- 2. Architecture & Design
- 3. Development & Integration
- 4. Testing, Deployment & Onboarding
- 5. Maintenance & Scaling
- 6. Change Management & Adoption
- Technical & Architecture Considerations
- 1. Architecture Style
- 2. Data Modeling
- 3. API Strategy
- 4. Scalability & Performance
- 5. Security & Compliance
- 6. Interoperability
- Data Migration & Switching from Legacy Systems
- Start with a solid migration plan
- Handle downtime and data integrity carefully
- Train your people before flipping the switch
- Regulations, Compliance & Risk Management
- Understand Your Legal Requirements
- Make Systems Transparent and Traceable
- Design for Safety
- Get Certified
- Compliance Never Stops
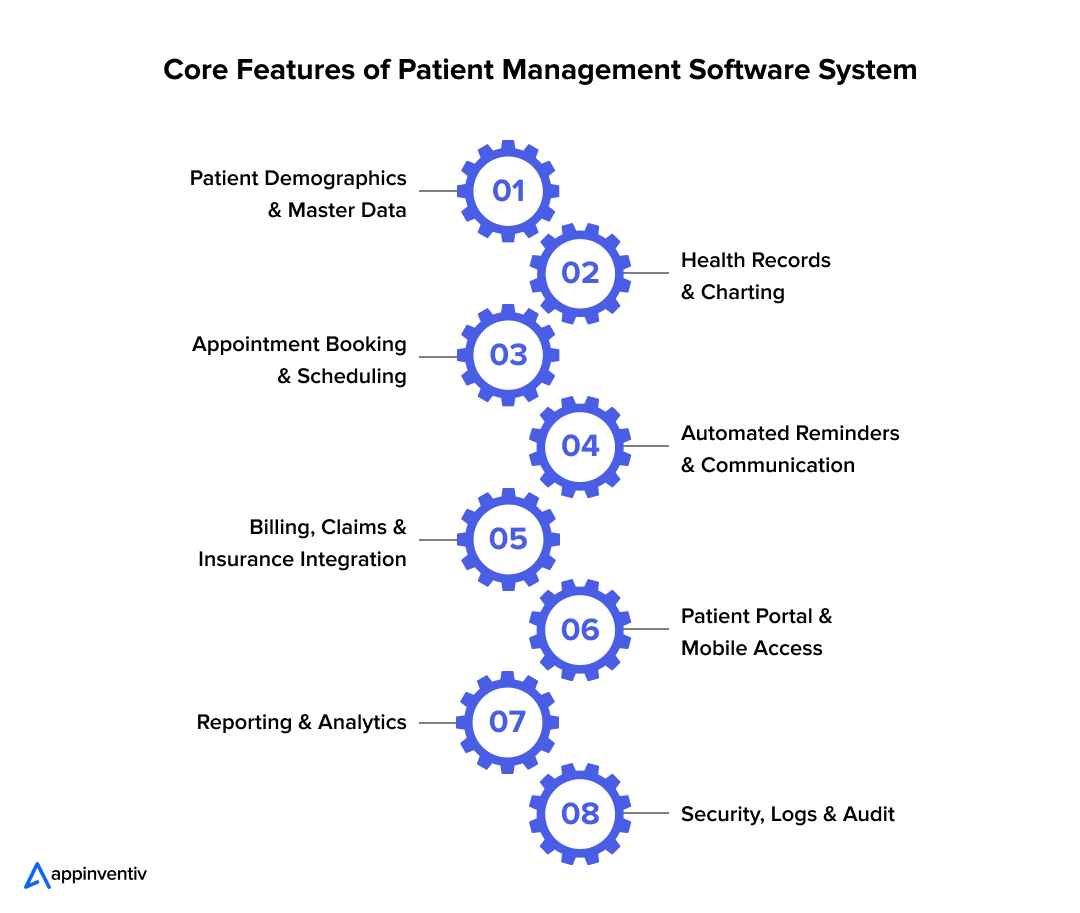
- Core Features of Patient Management Software System
- 1. Patient Demographics & Master Data
- 2. Health Records & Charting
- 3. Appointment Booking & Scheduling
- 4. Automated Reminders & Communication
- 5. Billing, Claims & Insurance Integration
- 6. Patient Portal & Mobile Access
- 7. Reporting & Analytics
- 8. Security, Logs & Audit
- Patient Management Software Development Cost Examined
- The Ongoing Investment
- Understanding ROI and Payback
- Challenges in Patient Management Software Development
- 1. Scope Creep and Feature Overload
- 2. Data Privacy and Evolving Regulations
- 3. Integration with Legacy Systems
- 4. User Adoption and Change Resistance
- 5. Technical Debt and Long-Term Maintenance
- 6. Security Risks and System Vulnerabilities
- 7. Migration Errors and Data Loss
- The Future of Patient Management Software
- 1. Smarter Care Through AI and Machine Learning
- 2. Real-Time Insights from Wearables and IoT Devices
- 3. Patient-Owned Data and Blockchain Security
- 4. Open Ecosystems and Plug-In Marketplaces
- How Appinventiv Can Help with Patient Management Software Development
- FAQs
Key takeaways:
- PMS is the Backbone of Healthcare: Patient Management Software (PMS) integrates critical functions like patient data, scheduling, billing, and communication into a unified system, streamlining hospital operations and improving patient care.
- Development Process: Building PMS involves discovery, design, development, and testing, with a focus on real healthcare workflows to ensure user adoption.
- Cost Efficiency: PMS development ranges from $40,000 to $400,000, with ROI typically realized within 12–18 months through improved efficiency and billing accuracy.
- Compliance and Security: PMS must comply with regulations like HIPAA and GDPR, with built-in security features to protect patient data.
- Scalability: Cloud-based, modular PMS allows for easy scalability and future integration of features like telehealth and AI tools.
Walk into almost any hospital today, and you’ll see the same chaos repeating itself- nurses juggling spreadsheets, front-desk staff buried under patient files, and doctors wasting precious minutes logging into three different systems just to find a single medical record. Behind that clutter lies a deeper problem: healthcare data is fragmented, slow, and costly to manage.
According to a report by The Business Research Company, the global healthcare software market is projected to reach $111.65 billion in 2029. Meanwhile, the American Hospital Association estimates that hospitals spend nearly $9.5 million annually on IT infrastructure alone. Despite these investments, inefficiency still drains time and resources- physicians spend about 36% of their work hours on administrative tasks, not patient care. For any healthcare enterprise, that’s a signal that digital transformation can no longer wait.
That’s where a Patient Management Software (PMS) comes in. And it’s not just about turning paper forms into PDFs. It’s about designing a connected software for patient management where every piece —records, scheduling, billing, and communication—works together instead of requiring three logins and five phone calls.
In this guide, we’ll walk through how to build patient management software that actually works in real healthcare settings: the stages you’ll move through, the patient management software development process, and what you should realistically expect to spend. No inflated estimates, no vague ranges. Just clear direction from field-tested experience.
Launch a patient management software system designed around your workflows.
Why Patient Management Software is a Strategic Investment: Market Insights
Healthcare is going through its biggest digital leap yet. The global medical software market is expected to grow from $58.9 billion in 2024 to $111.65 billion in 2029 at a compound annual growth rate (CAGR) of 13.4% (The Business Research Company), while the digital health sector could surpass $2.1 trillion by 2034 (Global Market Insights).
Even with all the technology available today, many hospitals aren’t getting the efficiency gains they expect. In the U.S., the average hospital spends around $9.5 million a year on IT (Definitive Healthcare), yet clinicians still spend about a third of their day buried in administrative tasks. A well-designed medical patient management software changes that- cutting repetition, reducing errors, and creating a connected system that truly supports both staff and patients.
Key Benefits of Patient Management Software
Patient Management Software (PMS) is essential for improving healthcare operations, enhancing staff productivity, and delivering better patient care. Here are its main benefits:
- Operational Efficiency: Reduces administrative workload, freeing up time for direct patient care and increasing overall productivity.
- Revenue Protection: Automates billing processes, ensuring accuracy and minimizing financial losses from errors.
- Enhanced Patient Experience: Simplifies appointment booking, sends automated reminders, and provides easy access to records, boosting patient satisfaction and reducing no-shows.
- Actionable Data: Consolidates data for real-time insights, helping identify and resolve operational bottlenecks quickly.
- Streamlined Compliance: Built-in access controls, audit logs, and encryption help meet compliance standards without manual effort, reducing risk.
- Scalability and Flexibility: Modular or cloud-based systems easily scale to accommodate growth and new features, like telehealth and AI integration.
How to Build Patient Management Software?
Creating software for patient management isn’t just about coding screens for your team; it’s about designing a workflow solution people will actually use. Here’s the proven, phase-by-phase approach to building the patient management software.
1. Discovery & Research
Begin by gaining a deep understanding of your hospital’s workflow to identify inefficiencies and ensure the software is aligned with real-world needs.
- Start by watching how your hospital really operates.
- Shadow nurses during their shifts. Sit with the front desk staff. You’ll quickly see the actual problems: staff entering the same patient data three times, test results taking two days to reach the right doctor, and appointments getting double-booked because two systems don’t sync.
- Map everything from patient check-in through discharge. Write down what slows people down.
- Benchmark existing patient management software examples in the market to see what works and what frustrates users.
- Figure out your compliance requirements now- HIPAA, GDPR, local regulations. Retrofitting compliance later costs about three times more.
What you need: A requirements document showing real problems, not theoretical ones.
2. Architecture & Design
This will decide if your system becomes a valuable asset or a costly burden.
- Pick your structure. Monolithic works if you’re small. Microservices make sense if you plan to grow or need flexibility.
- Design data flow carefully. Patient records, appointments, billing- everything needs clean connections and clear ownership.
- Choose a tech stack for patient management software early, focusing on frameworks, databases, and APIs that balance performance with compliance.
- Security goes in first, not last. Encryption, access controls, and audit logging. One breach destroys the trust you spent years building.
- Use FHIR and HL7 if you want your system to work with anyone else’s. These aren’t suggestions; they’re how healthcare IT actually connects.
3. Development & Integration
Focus on building the core functionalities and integrating the system incrementally to ensure the platform meets the real needs of healthcare staff.
- Build core functions first: patient records, scheduling, billing, and basic reporting.
- Work in short cycles. Test every two weeks, not every six months.
- Put actual nurses and doctors in front of the system while you’re building it. A billing manager will spot problems in five minutes that your developers would miss for months.
- Use APIs to link CRM for patient management so communication data feeds directly into care plans.
- Watch every click. Healthcare staff don’t have time for complicated interfaces.
4. Testing, Deployment & Onboarding
Ensure the system is secure, compliant, and user-friendly before launching it to guarantee a smooth transition and maximum adoption.
- In healthcare, testing means patient safety.
- Test how it works, how it performs under load, how it holds up when someone tries to break in. Check every compliance requirement.
- CI/CD pipelines allow safe updates and quick rollback when issues arise- critical for a cloud-based patient management system that runs 24/7.
- Deploy to one department first. Watch what happens. Fix problems. Then expand.
- Train people properly. Nobody uses software they don’t understand.
5. Maintenance & Scaling
Your PMS needs to grow as your organization does.
- Monitor everything: system performance, error rates, and user complaints.
- Update regularly. New features matter, but so does staying compliant as regulations change.
- Add capacity before you need it. Patient volumes don’t grow on convenient schedules.
- Refactor old code before it breaks. Technical debt compounds fast.
- When staff report the same issue repeatedly, that’s not a training problem; that’s a system problem. Fix it.
- Track ROI metrics to refine your patient management software revenue model by assessing how efficiency savings, licensing, or subscription pricing sustain growth.
6. Change Management & Adoption
Successful adoption depends on engaging staff early, addressing concerns, and demonstrating the value of the new system to ensure widespread use.
- Software works when people choose to use it.
- Start with one department. Get it right there. Then spread.
- Find staff members who like the new system and let them help their colleagues.
- Ask for feedback often, but keep it short. Fix small frustrations quickly.
- Show results: fewer hours on admin work, faster patient check-ins, better data accuracy.
- You know it’s working when staff start saying they prefer the new system. That’s success.
A successful AI-driven patient management system rollout doesn’t feel forced; it feels like the hospital just got easier to run.
Also Read: Hospital Management System Software Development
Technical & Architecture Considerations
The architecture behind your patient management system software determines how secure, fast, and scalable it will remain over the next five to seven years. Here’s what experienced teams focus on from day one.
1. Architecture Style
Choose your architecture style- Monolithic or Microservices:
- Monolithic: Works well for smaller operations needing quick deployment. Straightforward initially. As your system grows, updates become risky; changing one component can break others. Scaling means scaling everything, even parts that don’t need it.
- Microservices: Each module (billing, scheduling, records) runs independently. You can scale the appointment system without touching billing. Updates happen without downtime. The cost: more complexity upfront and higher operational overhead.
Most organizations we’ve worked with initially choose a modular monolith, built in separable components. You get speed to market now, with the option to split into microservices later when growth justifies the complexity.
2. Data Modeling
A well-structured data model is key to ensuring smooth operations, compliance, and data accuracy across your patient management system.
- Data structure affects everything: query performance, compliance audits, and system reliability.
- Core entities: Patients, Appointments, Encounters, Billing, Claims, Audit Logs.
- Normalize schemas for data integrity. Use JSON fields where data requirements evolve frequently.
- Soft deletes and versioning preserve historical records. Healthcare regulators expect complete data lineage.
- Audit trails track every modification. Not optional, medical liability and HIPAA require comprehensive change logs.
- Store all in a secure, patient management system environment for redundancy and disaster recovery.
3. API Strategy
APIs are the lifelines of a medical patient management software- connecting it to labs, pharmacies, EHRs, and payers.
- REST remains standard across healthcare IT. GraphQL works better when frontend teams need flexible data queries without backend changes for each requirement.
- Version your endpoints (/api/v1/). Breaking changes during updates disrupt partner integrations.
- Keep previous versions operational during migration periods. Forced upgrades damage partner relationships.
- Rate limiting prevents single users from overwhelming your infrastructure. Pagination keeps responses manageable.
Well-structured APIs also enable integration with a CRM for patient management, improving follow-ups, reminders, and retention analytics.
4. Scalability & Performance
Healthcare facilities operate continuously. Your infrastructure needs to match.
- Cache frequently accessed data (Redis, Memcached). Patient demographics and appointment schedules are read far more often than written.
- Index databases properly. Paginate results. Lazy load when appropriate. Poor query optimization kills performance with large patient datasets.
- Scale horizontally- add servers as load increases rather than perpetually upgrading single servers.
- Separate analytics workload through read replicas. Reporting queries won’t slow patient registration.
- Background queues handle heavy processes, report generation, and notification batches, without blocking user interactions.
- Planning for scale during initial development costs substantially less than emergency rebuilding when your system fails as it grows.
5. Security & Compliance
Ensuring the security and compliance of patient data is critical to maintaining trust and avoiding costly penalties.
- Healthcare data breaches make headlines and cost organizations millions in fines and lost patient trust.
- Encrypt data in transit (TLS) and at rest (AES-256).
- Role-based access control. Users see only the data their role requires.
- Multi-factor authentication for administrative access and sensitive operations.
- Log every action involving patient data or configuration changes.
- Track patient consent explicitly. Apply retention policies matching HIPAA or GDPR requirements.
- Regular penetration testing is necessary, not just at launch. Threats evolve constantly.
6. Interoperability
Your PMS needs to communicate with the broader healthcare ecosystem, or it becomes an isolated tool.
- FHIR for modern integrations- REST-based, well-documented, increasingly standard.
- HL7 (v2/v3) for legacy systems. Most established hospitals still rely on these protocols extensively.
- DICOM for radiology and imaging integration.
- Build adapters for older systems that don’t follow standards. You’ll encounter them.
- Supporting multiple data exchange standards isn’t optional if you want broad market adoption.
The stronger your interoperability layer, the easier it becomes to future-proof your patient management software development investment.
Build a custom Patient Management Software System with EHR integration, AI scheduling, and real-time analytics, all tailored to your compliance needs.
Data Migration & Switching from Legacy Systems
Migrating from an old hospital system to a new medical patient management software is never just about transferring data- it’s about protecting years of medical history without disrupting ongoing care. Most hospitals underestimate this phase, but it’s where success or failure is often decided. That’s why it’s crucial to understand the complexities of migrating healthcare legacy systems.
Start with a solid migration plan
Migrating from old systems requires meticulous planning and careful execution to ensure accuracy and minimal disruption.
- Begin by identifying what data truly needs to move- patient records, lab reports, billing information, and access logs. Legacy systems are often cluttered with duplicates and outdated files, so this is the time to clean house.
- Use a mapping process to match old fields to new ones and test migrations to validate accuracy. ETL (Extract, Transform, Load) tools can automate much of this, but human review is still essential- a mislabeled allergy or incorrect ID can create real risks.
- Avoid “big bang” migrations. Instead, go incremental- move data in smaller batches while running both systems in parallel. This approach lets you monitor accuracy and performance without interrupting daily operations.
Handle downtime and data integrity carefully
A successful migration requires proactive planning to avoid disruption and ensure staff readiness.
- Schedule migrations during off-peak hours or weekends.
- Always have a rollback plan; if something goes wrong, you should be able to instantly restore data to its last stable state.
- Double-check consistency with audits after each phase of migration.
Train your people before flipping the switch
Ensuring your team is fully prepared is key to the successful implementation of new patient management software.
- Staff adoption is often overlooked. Before the go-live, walk teams through the new system using real scenarios- booking an appointment, finding a patient file, and generating a bill.
- Assign on-site support during the first few weeks to handle hiccups and build user confidence.
In a well-managed patient management software development process, migration shouldn’t feel like a launch- it should feel like continuity.
Regulations, Compliance & Risk Management
Compliance in healthcare protects patients and keeps your organization operational. Every patient record you handle represents potential legal liability. So your software for patient management must comply with multiple frameworks:
Understand Your Legal Requirements
Ensure compliance with relevant regulations for cross-border data.
- U.S. operations fall under HIPAA for patient data handling.
- European systems must meet GDPR requirements, which include stricter consent rules and mandatory data access rights.
- Regional laws now exist across GCC and APAC. Saudi Arabia has the PDPL. India has DISHA.
Figure out which regulations apply before you start working on it, especially if you’re handling data across borders.
Make Systems Transparent and Traceable
Implement audit trails and consent tracking to ensure data transparency and patient trust.
- Audit trails matter. Track who accessed which records, when, and why. Auditors ask for this first.
- Consent tracking needs to be clear. Patients should understand how their data gets used and be able to withdraw permission easily.
- Role-based access keeps staff from seeing information they don’t need for their job.
Design for Safety
Design interfaces with safety features to minimize errors and enhance usability for clinical staff.
- Bad interface design causes real problems. I’ve investigated medication errors that happened because a dropdown menu was confusing or a confirmation button wasn’t obvious enough.
- Confirmation prompts for critical actions. Validation rules that catch obvious mistakes. Automatic backups that prevent data loss.
- Test with actual clinical staff regularly. They spot usability issues that put patients at risk, issues developers never notice.
Get Certified
Certifications are essential for demonstrating data security and compliance.
- ISO 27001 and SOC 2 aren’t just paperwork. They demonstrate that you take security seriously.
- Hire legal counsel who knows healthcare IT. Generic corporate lawyers miss critical requirements in data-sharing agreements and privacy policies.
- Many hospitals won’t work with vendors lacking proper certifications. These credentials aren’t optional if you want market access.
Compliance Never Stops
Ongoing audits and updates are necessary to stay compliant and maintain patient trust.
- Regulations change. New privacy laws pass. Security threats evolve. Your compliance program needs to keep pace.
- Regular audits, updated training, policy reviews; these aren’t boxes to check annually. They’re how you avoid penalties and maintain patient trust.
Regulatory shifts are constant, which is why every patient care management software should have a continuous audit and review cycle.
Also Read: Medical Practice Management Software Development
Core Features of Patient Management Software System
Effective patient management system software needs to handle the basics exceptionally well before adding sophistication. Here are the essential patient management system features every healthcare organization needs.
1. Patient Demographics & Master Data
Ensuring accurate patient data from the beginning prevents long-term issues like duplicate records and billing errors.
- Get patient information wrong at the start, and you’ll fight those errors for years.
- Medical record numbers, national IDs, insurance references- these identifiers need to be correct and consistent. Demographics, emergency contacts, and provider assignments all live in one place. Insurance details link directly to billing records.
- An accurate database prevents duplicate records and billing mistakes that waste hours of staff time daily.
2. Health Records & Charting
Systematic and accessible clinical documentation improves decision-making and supports the continuity of care.
- Clinical documentation in medical patient management software is where care actually gets recorded- every encounter, diagnosis, test result, treatment decision.
- Notes, medications, outcomes, and progress updates are all documented systematically. Templates like SOAP or custom formats that match how your clinicians actually work are important. Supporting files are attached with proper version tracking.
- When physicians can see complete patient histories immediately, clinical decisions improve.
3. Appointment Booking & Scheduling
Clear visibility of availability and automatic alerts help optimize scheduling, reducing wait times and ensuring smooth operations.
- Scheduling gets complicated fast when you’re managing multiple providers across different locations.
- Calendar views need to show actual availability clearly. Recurring appointments, buffer times between visits, and automatic alerts when conflicts emerge. Capacity management that provides flexibility without creating constant overbooking problems.
- Effective scheduling cuts wait times and helps staff coordinate better. It’s the backbone of any AI-driven patient management system that optimizes utilization automatically.
4. Automated Reminders & Communication
Automated reminders and two-way communication systems reduce no-show rates and improve patient outcomes with minimal staff effort.
- Most patients who miss appointments simply forget. They didn’t choose to skip care.
- Automated reminders via SMS, email, or app notifications. Two-way messaging so patients can confirm or reschedule without calling your front desk. Follow-up messages after visits, checking on recovery or next steps.
- A good reminder system, ideally integrated through a CRM for patient management, cuts no-shows roughly in half for most practices. That’s recovered revenue and better patient outcomes.
5. Billing, Claims & Insurance Integration
Integrated billing and claims management systems streamline administrative tasks, saving time and ensuring smoother financial operations.
- Healthcare billing is complicated. Your software shouldn’t make it worse.
- Instant insurance verification before appointments. Electronic claim submission directly from the system. Denial and appeal management in the same interface, handling everything else. Co-pay and payment tracking without manual spreadsheet work. Integrated online payment processing.
- When billing runs smoothly, staff spend less time on administrative tasks and more time helping patients.
6. Patient Portal & Mobile Access
A cloud-based patient management system enhances patient engagement by providing easy access to health records, appointments, and payments from any device.
- Patients now compare healthcare access to their banking apps. That’s your competition for convenience.
- A well-designed cloud-based patient management system lets them view records, book appointments, and pay bills from any device.
- Easy access keeps patients engaged with their care and loyal to your practice.
7. Reporting & Analytics
Real-time data tracking and visualized performance metrics allow healthcare providers to identify issues early and make data-driven decisions for improved efficiency.
- Your practice generates enormous amounts of data daily. Most sit unused because analyzing them manually takes too long.
- Provider utilization tracking, facility usage patterns, department performance metrics. Revenue cycle monitoring, claim rejection rates, and attendance patterns. Dashboards showing what matters without requiring technical expertise to interpret.
- Real-time visibility lets you identify problems early and make decisions based on actual performance.
8. Security, Logs & Audit
Robust security measures, audit logs, and compliance tools ensure patient data integrity while safeguarding against breaches and maintaining trust.
- One serious data breach can cost millions in fines and destroy the patient trust you spent years building.
- Complete logs documenting who accessed which data when. Soft deletes allow recovery from accidental data removal. Automated monitoring flags unusual access patterns immediately.
- Strong security protects your organization’s reputation and viability. Meeting minimum compliance standards isn’t enough- actual protection matters.
Together, these patient management system features form the foundation of every scalable patient management software development initiative.
Patient Management Software Development Cost Examined
When healthcare organizations plan to build a Patient Management Software (PMS), one of the first questions that comes up is cost, and rightly so. Developing a system that manages patient data, billing, and operations across departments isn’t a small project. But when done right, it’s an investment that starts paying back faster than most expect.
The cost to build a Patient Management Software typically ranges from $40,000 to $400,000, depending on scale and complexity.
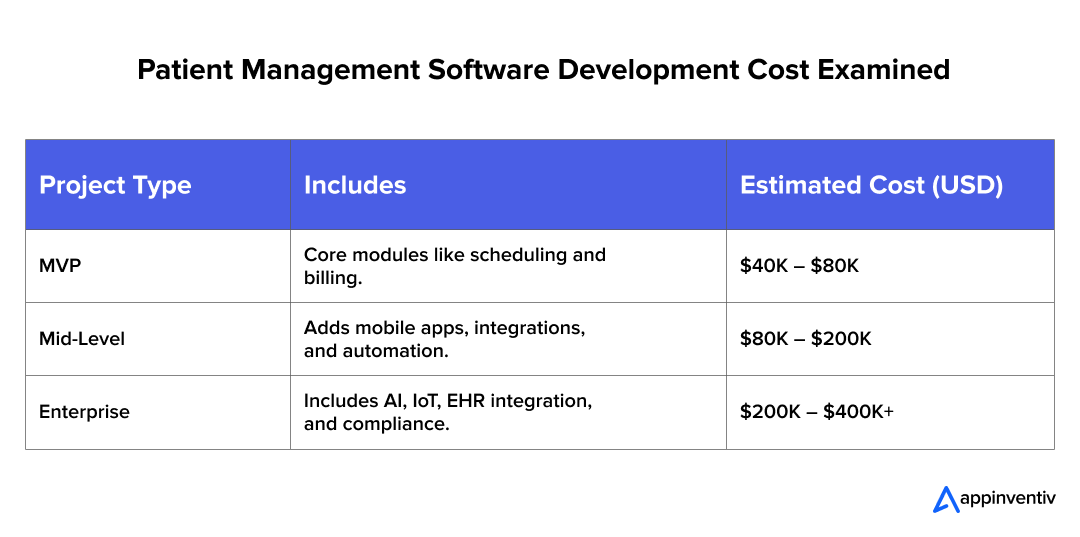
Here’s a cost breakdown of patient management software phase-wise:
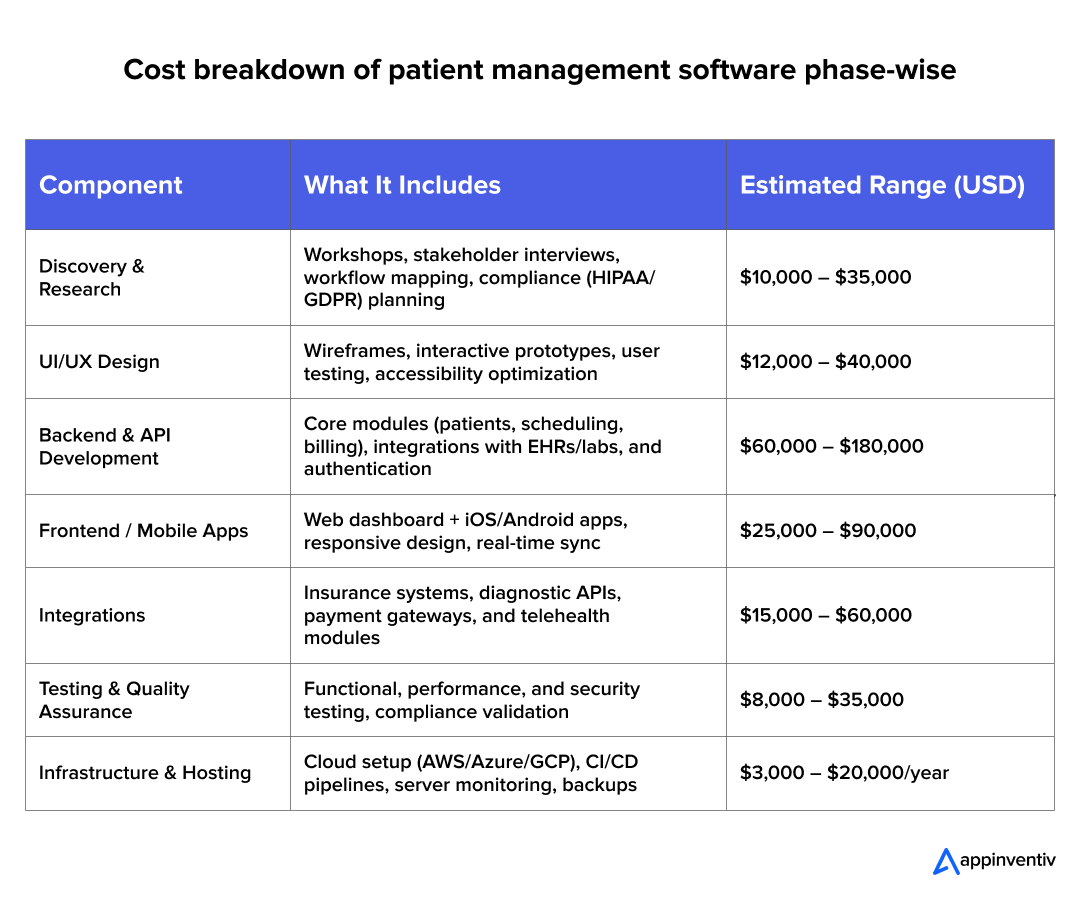
These numbers shift based on factors affecting patient management software cost- like region, developer expertise, integration complexity, and long-term support.
The Ongoing Investment
Going live doesn’t end the project- it starts a different phase. Most healthcare organizations budget roughly 15-25% of their initial development cost annually for maintenance and improvements.
That covers:
- New modules or features based on what staff actually need
- Compliance updates when regulations change (HIPAA modifications, new local requirements)
- Server capacity expansion as your data volume grows
- Performance monitoring and security oversight
- User support and training for staff changes or when needed
Your PMS needs to evolve with your organization. Regulations shift. Technology advances. Patient expectations change. Systems that can’t adapt become expensive problems.
Understanding ROI and Payback
The cost to build a patient management system pays off quickly: most hospitals see positive ROI within 12–18 months. That’s faster than many administrators expect when they’re looking at the initial price tag.
The improvements compound:
- Staff recover hours weekly through automated scheduling and billing. One hospital documented saving approximately 15 hours per week in administrative team time, which was redirected to patient care and reduced overtime costs.
- Fewer claim denials and faster payment processing improve cash flow noticeably. Revenue that used to take 45-60 days to collect often comes in within 30 days with proper systems.
- Patient retention improves when scheduling is easier, communication is better, and the overall experience feels less bureaucratic. Patients who can manage their care conveniently tend to stay with your practice.
A mature patient management software revenue model aligns cost savings with continuous operational improvements- a measurable, ongoing return on technology investment.
Also Read: Medical Scheduling Software Development Cost Estimation
Challenges in Patient Management Software Development
Building a patient management system software appears straightforward during initial planning. Reality proves more complex once development begins. Regulatory requirements, integration constraints, and organizational change management create challenges that experienced teams must navigate carefully.
These are the key challenges that experienced teams learn to navigate early in the patient management software development process.
1. Scope Creep and Feature Overload
It’s essential to stay focused on the core functionalities before expanding the scope of the software project.
- Stakeholders continuously request additional features. What begins as focused patient management software gradually expands into an enterprise platform attempting to address multiple organizational needs simultaneously.
- Each addition extends development timelines, increases costs, and compounds system complexity.
Lesson learned: Successful implementations start with a well-defined MVP. Build core functionality reliably. Introduce enhancements after validating system stability in production environments with actual users.
2. Data Privacy and Evolving Regulations
Adapting your system to meet evolving healthcare regulations is key to maintaining compliance.
- Healthcare regulations evolve continuously. HIPAA undergoes periodic updates. GDPR enforcement intensifies. New regional requirements emerge, such as PDPL. Systems require adaptation capacity without fundamental reconstruction.
- One healthcare organization spent six months retrofitting compliance into its existing architecture, costing approximately three times what a proper initial design would have required.
Tip: Design regulatory flexibility into your architecture from the beginning. Accommodating new privacy requirements shouldn’t necessitate rewriting core data management layers.
3. Integration with Legacy Systems
Successful integration of modern systems with older legacy platforms requires a careful, strategic approach.
- Many healthcare facilities operate on systems developed decades ago that predate modern integration standards. New medical patient management software implementations must interface with software using batch processing and proprietary protocols rather than contemporary APIs.
- This integration proves consistently more complex than initial assessments suggest.
Practical approach: Middleware or API gateway solutions become essential. They translate between modern systems and legacy infrastructure. Parallel operation of both systems often continues for extended periods, typically longer than initial projections, until complete modernization becomes feasible.
4. User Adoption and Change Resistance
Ensuring that users are engaged and involved early on helps overcome resistance and aligns the system with their workflows.
- Even the most elegant patient care management software fails if staff resist it. Clinicians already juggle heavy workloads and often fear added complexity.
- Technically sound systems fail when end users aren’t involved during development. By implementation, workflows don’t align with actual clinical practice patterns.
Pro insight: Engage end users throughout development. Conduct prototype testing with actual clinicians and staff. Incorporate their feedback systematically. Adoption rates improve significantly when users contribute to system design rather than having solutions imposed on them.
5. Technical Debt and Long-Term Maintenance
Planning for continuous improvements and addressing technical debt early can prevent complications down the line.
- Development pressure creates shortcuts. Documentation gets deferred. Refactoring gets postponed. Sprint timelines compress to meet milestones.
- These decisions accumulate as technical debt. Months after deployment, code complexity increases. Bug resolution becomes more time-consuming. Routine updates require extensive effort due to decreased system comprehensibility.
Best practice: Schedule code reviews and refactoring into development cycles, even if it slightly delays the initial deployment. The alternative involves spending substantially more time later addressing preventable problems.
6. Security Risks and System Vulnerabilities
Maintaining a proactive approach to security and continuous testing ensures the safety and integrity of sensitive patient data.
- Healthcare data remains a primary target for security breaches. Single vulnerabilities, even seemingly minor ones, can expose extensive patient information.
- Financial penalties prove severe. Reputational damage extends further. Patient trust erodes. Regulatory scrutiny intensifies. Institutional relationships suffer.
Tip: Conduct penetration testing regularly throughout the system lifecycle, not solely before initial launch. Enforce multi-factor authentication. Treat security as a continuous operational practice rather than a deployment requirement.
7. Migration Errors and Data Loss
A careful, step-by-step migration process is necessary to avoid data inconsistencies and potential disruptions in patient care.
- Transitioning from existing systems to new PMS exposes data inconsistencies that existed undetected for years. Patient records have inconsistent formatting. Duplicate entries under variant naming conventions. Billing codes are misaligned with current standards.
- Single errors in patient record matching can cause billing discrepancies or clinical documentation mistakes with significant consequences.
- Migrate systematically in stages. Validate thoroughly at each phase. Maintain comprehensive backup protocols. Operating both systems in parallel longer than the initial estimates suggest is necessary. Confirm accuracy across all critical data categories before the complete system transition.
What works: This approach requires more time. It costs substantially less than correcting migration errors in production environments where patient care depends on system reliability.
Connect with our healthcare tech experts and get a cost plan built around your goals.
The Future of Patient Management Software
The healthcare industry is evolving faster than ever, and Patient Management Software (PMS) is right at the center of that transformation. The next era of AI-driven patient management system design will focus on intelligence, connectivity, and ownership.
Here are a few trends already reshaping what tomorrow’s PMS will look like.
1. Smarter Care Through AI and Machine Learning
Artificial Intelligence is making patient management software development smarter. Modern PMS platforms are beginning to use AI to predict who might be at risk of complications, readmission, or chronic conditions before symptoms even appear.
For example, Hospitals are already using predictive models to identify high-risk patients and intervene early- reducing both costs and hospital stays.
AI is also helping automate repetitive tasks like coding, billing, and record updates, freeing medical staff to focus on what matters most- care delivery.
2. Real-Time Insights from Wearables and IoT Devices
Smartwatches, glucose monitors, and connected health sensors are no longer consumer gadgets; they’re becoming extensions of clinical monitoring.
When integrated with a cloud-based patient management system, these devices feed real-time data such as heart rate, oxygen levels, and sleep quality directly into a patient’s profile.
Why this matters: Doctors don’t have to wait for the next appointment to see if a patient’s condition is worsening; they can act the moment data shows a red flag. This kind of continuous monitoring is helping shift healthcare from reactive to preventive.
3. Patient-Owned Data and Blockchain Security
The conversation around patient privacy is changing. People no longer want just to access their health data; they want to own it.
Blockchain-based software for patient management is making that possible by creating secure, verifiable systems where patients control who can view or share their medical records.
The big shift: Instead of storing all data in centralized hospital servers, the future points toward decentralized systems that give patients ownership while improving transparency and reducing data tampering risks.
4. Open Ecosystems and Plug-In Marketplaces
Patient Management Software is starting to look less like a single application and more like a digital platform.
Hospitals now want flexibility, the ability to plug in telehealth, AI-powered diagnostics, or remote monitoring tools without rebuilding their system.
What’s next: Expect to see PMS platforms evolve into open, collaborative ecosystems, where healthcare providers, developers, and device manufacturers work together to deliver innovation faster.
How Appinventiv Can Help with Patient Management Software Development
At Appinventiv, we don’t just build digital platforms; we provide healthcare custom software development services that improve how care is delivered. Our team of over 1,600 specialists has delivered 250+ healthcare projects globally, including advanced patient management software development, EHR/EMR platforms, and full hospital management systems.
We’ve helped hospitals:
- Reduce nurse response times by 60% with building Healthcare queue management software like YouCOMM.
- Connect 200+ medical devices through Health-e-People for personalized data insights.
- Improve diabetes care through connected wearables in DiabeticU.
Whether you want to create a patient management system for hospitals, build a cloud-based patient management system, or integrate telehealth and EHR modules, our software team guides you from discovery through deployment and beyond.
We ensure every medical patient management software we develop is secure, scalable, and ready to evolve- combining technology excellence with compliance, usability, and long-term support.
If you’re ready to move from concept to execution, let’s connect. We can help you scope, estimate, or even build your next-generation PMS tailored for your clinic’s needs.
FAQs
Q. What is Patient Management Software?
A. Patient Management Software (PMS) is a digital system that helps hospitals and clinics manage everyday operations from scheduling and patient records to billing and communication. It connects clinical, financial, and administrative workflows, allowing teams to spend less time on paperwork and more time focusing on patient care.
Q. How much does it cost to build a patient management software?
A. The cost depends on the scale and complexity of the system. On average, building a custom PMS can range between $80,000 and $250,000+, depending on factors like integrations, compliance needs, and mobile app support. Smaller clinics may start at the lower end, while multi-location networks with advanced modules (AI, IoT, telehealth) typically require a larger investment.
Q. How to develop a Patient Management Software?
A. Developing a PMS involves several phases. Let’s know how to build patient management software
- Discovery & Planning: Understanding workflows and compliance needs.
- Design: Creating user-friendly interfaces and patient journeys.
- Development: Building core modules like records, billing, and scheduling.
- Integration: Connecting with labs, EHRs, or insurance systems.
- Testing & Deployment: Ensuring performance, security, and compliance.
A strong focus on user feedback throughout the process ensures the software aligns with real clinical needs.
Q. How long does it take to develop a PMS?
A. Most PMS projects take between 4 and 9 months, depending on the scope. A basic MVP for a single clinic might be ready in four months, while a feature-rich enterprise platform with multiple integrations can take close to a year. Timelines are shorter when the project starts with a clear scope and agile development approach.
Q. What are the benefits of Patient Management Software?
A. PMS simplifies hospital operations by automating manual processes. It:
- Operational Efficiency: Administrative tasks consume a significant portion of clinical staff time. By integrating PMS, hospitals can reduce time spent on manual documentation and administrative duties, allowing more time for direct patient care. This leads to a more efficient and productive environment for both staff and patients.
- Revenue Protection: Billing errors can lead to significant financial losses. PMS reduces these risks by automating billing processes, improving accuracy, and catching errors before claims are submitted. This ensures smoother revenue cycles and minimizes the potential for costly mistakes.
- Enhanced Patient Experience: A well-integrated PMS enables online booking, automated reminders, and easy access to medical records, which significantly enhances the patient experience. These tools not only improve appointment adherence but also contribute to a more efficient workflow, reducing no-show rates and increasing patient satisfaction.
- Actionable Data: A good PMS consolidates data across departments, providing real-time insights into operational performance. Dashboards allow healthcare managers to quickly identify bottlenecks, such as understaffed shifts or scheduling gaps, enabling proactive solutions that improve overall workflow efficiency.
- Streamlined Compliance: Compliance with healthcare regulations, such as HIPAA, is crucial. PMS solutions simplify the process by incorporating built-in access controls, audit logs, and encryption. This ensures that compliance standards are met without the need for constant manual monitoring, reducing the risk of violations and potential penalties.
- Scalability and Flexibility: A modular or cloud-based PMS is designed to scale with your healthcare organization’s needs. Whether adding telehealth features, integrating AI tools, or expanding to new departments, these systems provide the flexibility to grow without requiring a complete overhaul of existing infrastructure. This future-proofing ensures that the system evolves as your organization does.
Q. What are the compliance requirements for Patient Management Software?
A. Compliance depends on where the healthcare provider operates. In most regions, systems must meet:
- HIPAA (United States)
- GDPR (European Union)
- PDPL / NDPB (Middle East and GCC)
- ISO 27001 / SOC 2 certifications for global data security
These frameworks govern how patient data is collected, stored, shared, and audited. A compliant PMS should also include role-based access, consent tracking, and full audit trails.
Q. How do you integrate EHR/EMR into Patient Management Software?
A. Integration is achieved through secure APIs or middleware that connect your PMS with Electronic Health Record (EHR) or Electronic Medical Record (EMR) systems. Using healthcare standards like FHIR and HL7, data such as lab results, prescriptions, and patient charts can flow seamlessly between systems, eliminating manual entry and improving care coordination.
Q. What is the ROI of Patient Management Software for hospitals?
A. Hospitals typically start seeing measurable returns within 12 to 18 months of implementation. ROI comes from multiple areas: reduced administrative workload, faster billing cycles, fewer denied claims, improved patient retention, and higher staff efficiency. Beyond financial gain, the biggest return is in operational transparency and patient trust, two metrics that define long-term success in healthcare. The right patient management software revenue model combines operational savings with long-term growth potential.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…