- Telehealth is More Than Video: Redefining the Care Delivery Ecosystem
- Who Benefits from Telemedicine? Targeting Patients, Providers, and Business Models
- Types of Telemedicine Platform Development: Selecting the Right Platform
- General Telemedicine Apps
- Specialized Care Apps
- Remote Patient Monitoring (RPM) Apps
- Hospital/Clinic Integrated Platforms
- Video Consultation Platforms
- AI-Powered Diagnostic Tools
- E-Pharmacy Integration
- Why Telemedicine Apps Create Strategic Value: Market Drivers & Business Models
- Wider Patient Reach
- Lower Costs
- Higher Patient Engagement
- Operational Efficiency
- Reduced No-Shows
- Essential Features of a High‑Impact Telehealth App for Users and Providers
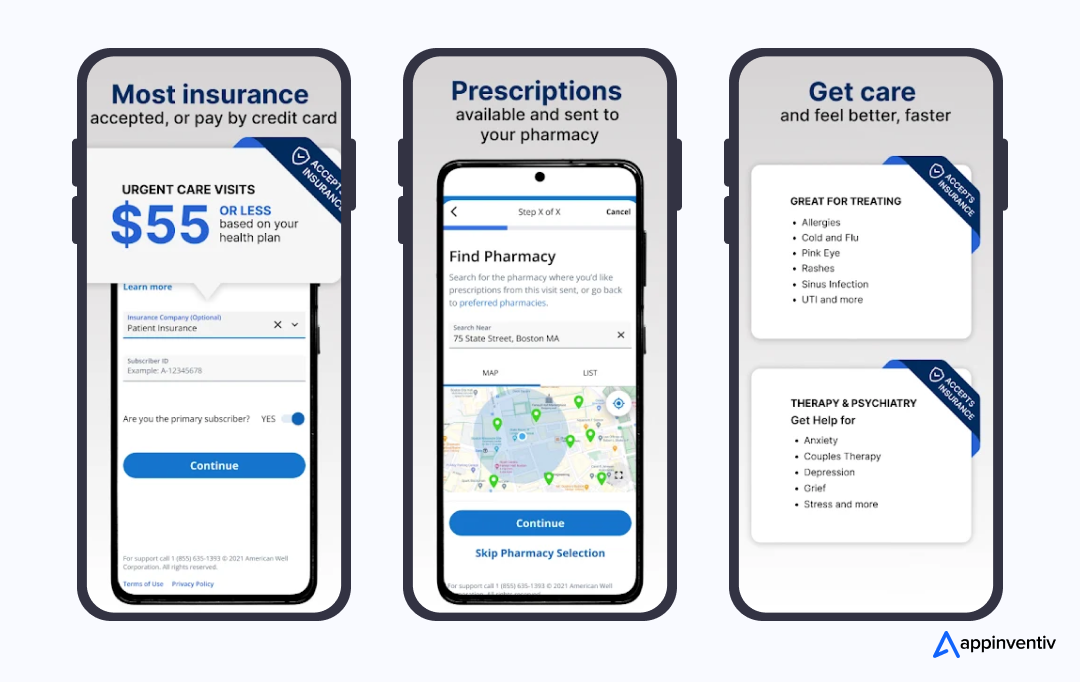
- Telehealth App Features for Patients
- Telehealth App Features for Doctors
- Telehealth Features for Admins
- Advanced Telemedicine Application Development Capabilities That Elevate Your Platform: Beyond the Basics
- AI-Powered Triage and Chatbots
- Remote Patient Monitoring with IoT
- Pharmacy and Lab Integrations
- Multilingual Support
- Cloud Scalability and Real-Time Sync
- Security & Compliance: Building Trust in Telemedicine from Day One
- Key Compliance Standards to Meet
- Security Best Practices
- How to Build a Successful Telehealth Application: From Idea to Launch and Scaling
- Market Research and Business Analysis
- Define Use Cases and Compliance Needs
- Craft UI/UX Design for Healthcare Environments
- Develop an MVP with Core Features
- Integrate with EHR/EMR and APIs
- Test the App for Functionality, Security, and Compliance
- Launch & Deploy the Telehealth Platform
- Post-Launch Support & Scaling
- Choosing the Right Tech Stack for Telemedicine App Development
- Sourcing Models for Telemedicine App Development: Freelancers vs. In-House vs. Outsourcing
- In-House Development
- Freelancers
- Outsourcing to a Healthcare Mobile App Development Company
- Challenges in Telehealth App Development & How to Overcome Them
- 1. Data Security and Compliance
- 2. Integration with Legacy Systems
- 3. Connectivity in Low-Bandwidth Regions
- 4. Building Patient and Provider Trust
- 5. Scalability Under High Demand
- Real-World Examples: Telemedicine App Success Stories That Inspire
- How Much Does Telehealth App Development Cost?
- What Are The Common Monetization Approaches For Telemedicine Apps?
- Emerging Trends and the Next Wave of Telehealth Platforms
- How Appinventiv Can Help You Build a Secure, Scalable Telehealth Platform
- FAQs
Key Takeaways
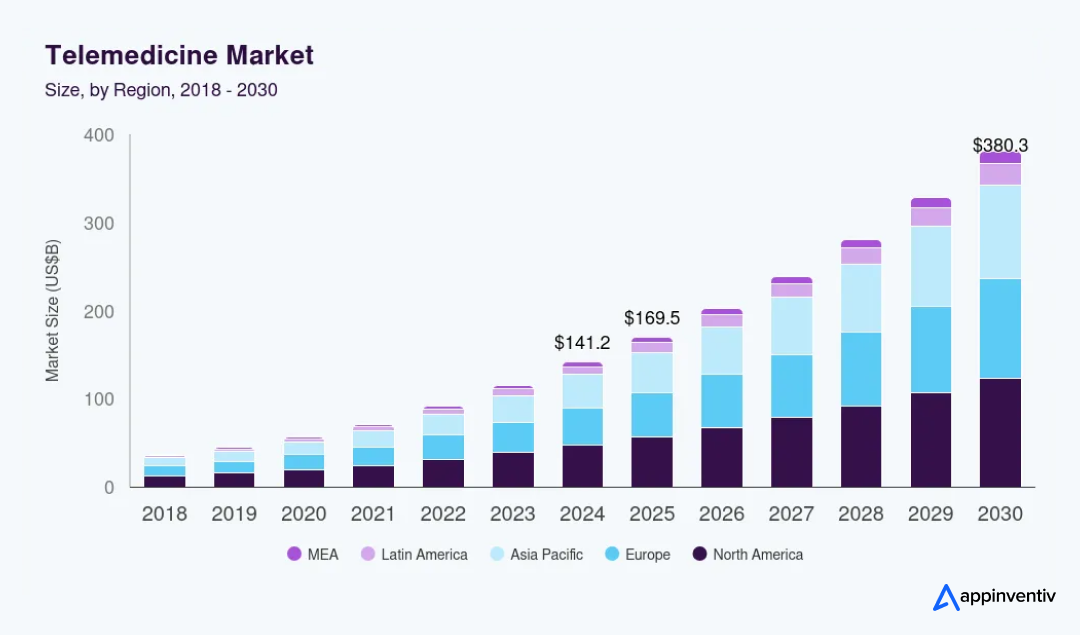
- The telemedicine market is growing rapidly and expected to reach US $380 billion by 2030.
- Focus on core features like video calls, scheduling, and e‑prescriptions, plus advanced options like AI triage.
- Compliance with HIPAA, GDPR, and security standards is essential for success.
- The development process requires a clear roadmap: research, design, MVP, integrations, testing, and scaling.
- Costs for telemedicine app development range from US $40K for basic apps to US $400K for complex platforms.
Remember those long, quiet hours in a doctor’s waiting room? The well-worn magazines, the rustle of a prescription pad, the subtle anxiety of being surrounded by strangers. For years, that was the baseline for healthcare.
Besides, healthcare professionals often lack the capacity to attend to everyone. We’re talking about the physician scarcity that’ll be short anywhere from 37,800 to 124,000 doctors by 2034 (AAMC Report).
And mental health? We’ve got only 30 psychologists per 100,000 people. Only 15 psychiatrists per 100,000 (Source: APA Healthcare Access Report). Meanwhile, anxiety and depression rates are climbing faster than Bitcoin in 2017.
But here’s the thing: smart leaders aren’t just complaining about this mess. They are building intelligent solutions. According to the McKinsey Telehealth Study, telehealth usage shot up 38 times higher than before the pandemic. And guess what? It was just the beginning of the telehealth revolution.
In 2024, the global telemedicine market was valued at $141.19 billion and is projected to reach $380.33 billion by 2030, growing at a CAGR of 17.55% from 2025 to 2030 (Source: Grand View Research). This isn’t just a market; it’s a movement. This market tells us two things. First, patient demand is not slowing down. Second, providers who move fast can capture new revenue streams. And for entrepreneurs, this is your chance to build the future of medicine.
So whether you’re running a hospital system, launching a startup, or just trying to figure out what the heck telemedicine application development actually involves, you’re in the right place.
This telemedicine app development guide will walk you through everything. It covers the types of telehealth platforms, their benefits, essential and advanced features, compliance requirements, costs, and future trends. By the end, you’ll know exactly how to develop a telemedicine app that’s secure, scalable, and ready for tomorrow’s patients.
Don’t miss your chance to capitalize on this thriving segment. Build your telehealth app today!
Telehealth is More Than Video: Redefining the Care Delivery Ecosystem
Telehealth is no longer a niche service. It’s a core pillar of healthcare delivery. What started as virtual consultations has now expanded into chronic care management, mental health therapy, teledermatology, and even remote surgery support.
So, as telehealth turns into a comprehensive healthcare solution, its benefits are not just limited to patients; it’s redefining the way providers deliver care as well as unlocking new business opportunities. Let’s dive into who exactly benefits from this shift and how different models are shaping the future of healthcare.
Who Benefits from Telemedicine? Targeting Patients, Providers, and Business Models
- Healthcare Providers: Hospitals and clinics get better workflows, faster reimbursements, and higher patient retention.
- Patients: Millennials prefer convenience, working individuals want to save time, while rural populations need access. Chronic disease patients value continuous monitoring. Telehealth apps serve all.
- Business Models:
- B2C apps connect patients directly with doctors.
- B2B platforms integrate telehealth into clinics and enterprise systems.
- B2B2C models let providers extend services under their own branding.
The lesson? The opportunity isn’t one-size-fits-all. So, before you even think about building an app, you need to choose your lane. Are you building a platform for everyone? Or are you a specialist? Think about platforms like Teladoc, which serve a broad audience. Their goal is to be the digital front door to healthcare. Then, you have the niche players, like behavioral health apps, elderly care platforms, and remote patient monitoring. Each segment has unique requirements. So, before you embark on your journey for custom telemedicine app development, consider who your target audience is.
Types of Telemedicine Platform Development: Selecting the Right Platform
Telemedicine is not a single product. It’s an umbrella of solutions, each designed for different care needs and business models. Understanding these categories is key before investing in telemedicine platform development.
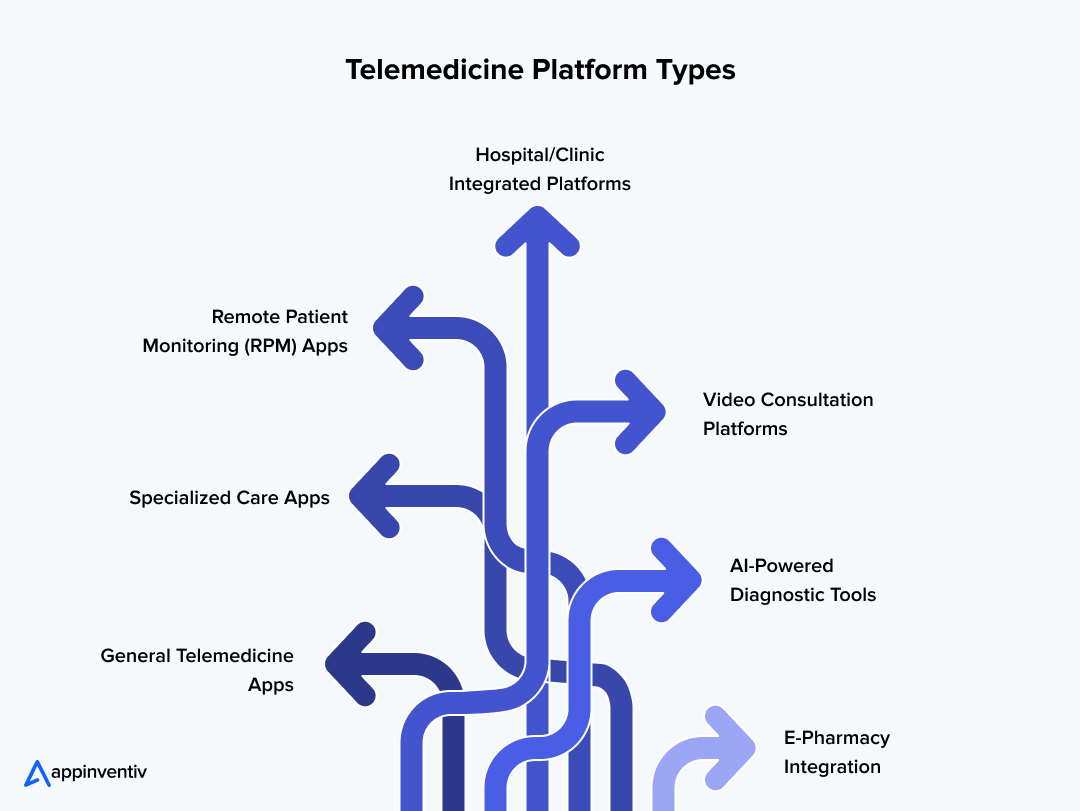
General Telemedicine Apps
These are the most common. They connect patients with doctors for everyday consultations. Think urgent care, flu symptoms, or basic follow-ups. They form the backbone of digital health.
These platforms connect patients with doctors for everyday consultations and immediate medical needs, making building an urgent care app a strategic investment for healthcare providers looking to offer 24/7 accessible care.
Specialized Care Apps
Some platforms go deep instead of wide. Mental health apps, such as Talkspace, as well as chronic care apps for diabetes and dermatology apps, fall under this category. Specialized platforms typically experience higher patient engagement because they address specific, targeted problems.
Remote Patient Monitoring (RPM) Apps
RPM combines telehealth device development with software. Patients use wearables or IoT-enabled devices to share vitals like blood pressure or glucose levels. Providers then track trends in real time, improving outcomes for chronic patients.
Hospital/Clinic Integrated Platforms
These solutions plug directly into existing hospital IT systems. They integrate EMR/EHR, scheduling, billing, and insurance. Enterprise-grade providers usually choose this path.
Video Consultation Platforms
This is a lighter version focused on secure video calls, file sharing, and prescriptions. This type of telehealth platform is often used by startups looking to launch quickly with white label telemedicine solutions.
AI-Powered Diagnostic Tools
AI-driven medical diagnostic platforms bring intelligence to the front. Symptom checkers, predictive analytics, and chatbots triage patients before they even meet a doctor.
E-Pharmacy Integration
Some pharmacy apps close the loop by connecting care with medication delivery. Patients receive prescriptions digitally and get medicines delivered at home.
Expert Insight: When deciding how to build a telemedicine platform, know that each of these models serves different needs. Some are taking care of compliance, feature, and scaling needs. That’s why custom telemedicine app development is rising. It adapts to both clinical goals and patient expectations.
Why Telemedicine Apps Create Strategic Value: Market Drivers & Business Models
Telehealth isn’t just about convenience. It changes the economics of care and reshapes how patients interact with providers. However, the benefits of telemedicine app development extend beyond the patient-provider interaction. They create value across the entire healthcare continuum. Here are the biggest benefits of investing in telehealth app development today:
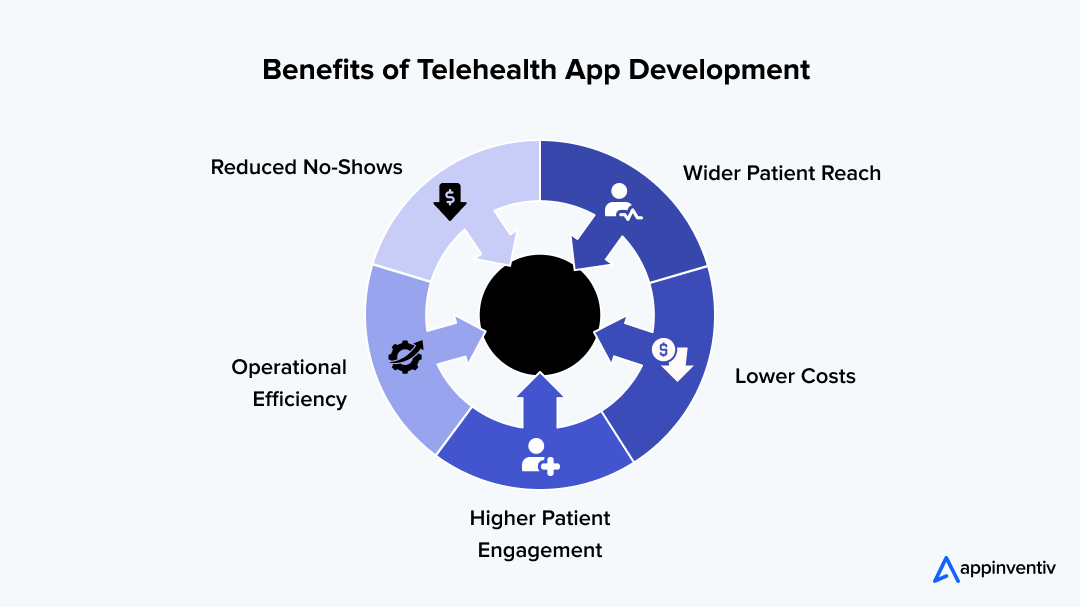
Wider Patient Reach
Geography is no longer a barrier. A patient in a rural town can access a top specialist in a major city with a few taps. That reach expands market share for providers and improves equity in care.
Lower Costs
Telehealth reduces overhead. Fewer in-person visits mean less strain on physical facilities. According to the National Institute of Health, telehealth was $3954 (total service cost) less expensive than a traditional in-person visit. That’s real money that can be reinvested in patient care. Patients save too; no travel, no waiting rooms.
Higher Patient Engagement
Telehealth app features like push notifications, digital prescriptions, and follow-up reminders keep patients connected. Engagement translates to better outcomes and higher satisfaction scores.
Operational Efficiency
Doctors optimize schedules. Admins get clearer data. Patients spend less time waiting. Efficiency builds loyalty, and loyalty drives retention.
Reduced No-Shows
Automated scheduling and virtual visits cut down missed appointments. This is one of the biggest sources of wasted revenue in healthcare.
Essential Features of a High‑Impact Telehealth App for Users and Providers
Feature selection makes or breaks your project. Different users need different stuff, but some features are absolutely essential. Here’s a breakdown of the core features your telehealth app can’t be developed without.
Telehealth App Features for Patients
Your patient’s experience has to be effortless. No one wants to spend hours trying to figure out how to book an appointment or join a consultation. Here’s how you create a frictionless experience.
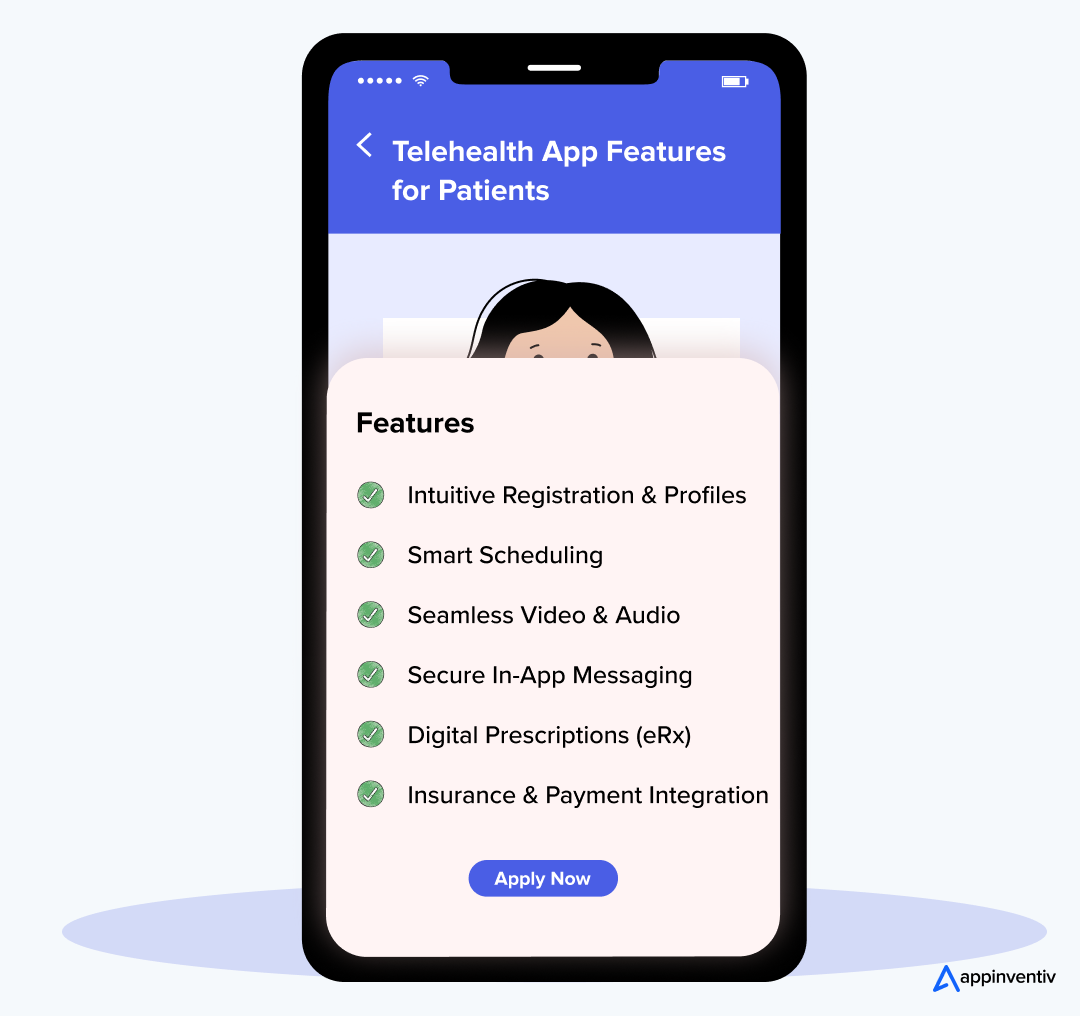
Intuitive Registration & Profiles
No one wants to fill out a 20-page form on their phone just for signing in. Keep it simple. Offer single sign-on (SSO) options via mail or social media platforms. This feature will help save time and reduce friction. A smooth, fast registration process builds trust right from the start.
Smart Scheduling
A real-time, dynamic calendar system that shows a doctor’s availability and allows patients to book instantly is non-negotiable. No more phone tag or endless back-and-forths with this feature. If possible, you should also consider integrating automated reminders to reduce no-shows.
Seamless Video & Audio
This feature is indeed the heart of your telemedicine platform. It needs to be crystal clear, smooth, and reliable. A connection dropping mid-consultation is a deal-breaker. Thus, you must use advanced video streaming protocols for minimal lag, especially for rural or low-bandwidth users.
Secure In-App Messaging
For quick follow-ups or clarifications, a secure chat system is essential. Before you implement a chatbot, make sure conversations are encrypted, stored in compliance with HIPAA/GDPR, and can be referred back to for future appointments. This provides a secure and organized communication channel, far better than unencrypted email or text.
Digital Prescriptions (eRx)
Allow doctors to send prescriptions directly to the patient’s pharmacy of choice. This feature will eliminate the need for manual handoffs, reducing mistakes and saving time. Offer features like a pharmacy locator or medication delivery integration for further convenience.
Insurance & Payment Integration
Make it easy for patients to pay. Whether through insurance verification, credit cards, or digital wallets like Apple Pay or Google Pay, make sure there are multiple secure options for payment. This improves accessibility and convenience for a broader audience.
Telehealth App Features for Doctors
Your app needs to be a helping hand, not a burden, for healthcare professionals. Thus, when considering how to develop a telemedicine app, you must add features that can make providers’ jobs easier and enhance their ability to provide quality care.
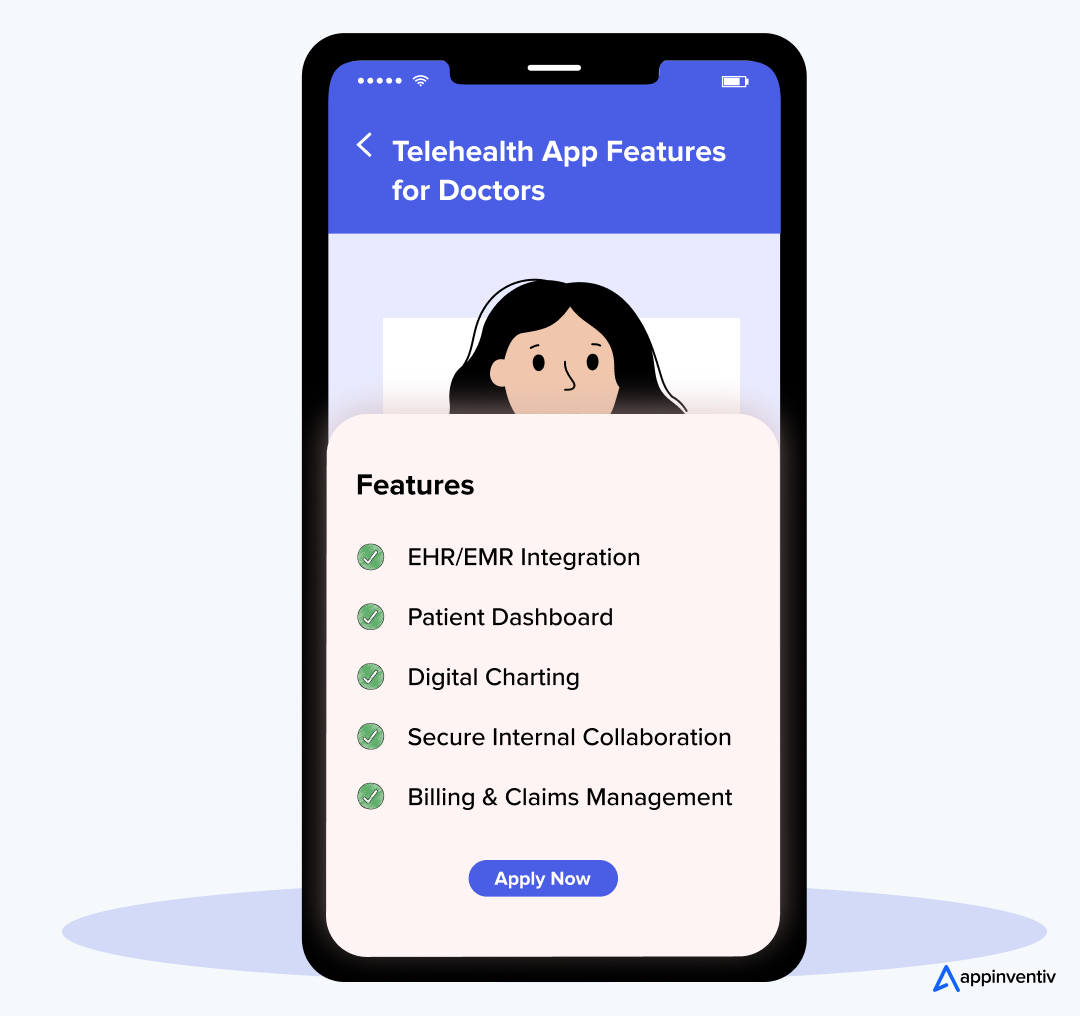
EHR/EMR Integration
This is a must-have feature. Doctors need the patient’s full medical history at their fingertips to make instant decisions at the time of emergencies. Thus, you must use FHIR (Fast Healthcare Interoperability Resources) as your standard for seamless integration with EHR systems to allow for smooth, real-time data exchange.
Patient Dashboard
This feature gives a single view of the patient’s profile, notes, records, and any relevant past consultations. This helps doctors quickly review health histories, treatment plans, and upcoming appointments, improving efficiency and diagnosis accuracy.
Digital Charting
Doctors need the ability to take real-time notes, add diagnoses, and create treatment plans within the app. This feature should enable voice-to-text functionality for quick updates and allow for the direct upload of images, such as X-rays and lab results.
Secure Internal Collaboration
A private and secure channel for doctors to consult with colleagues or specialists on complex cases. This feature could also allow for case sharing with secure permissions.
Billing & Claims Management
Streamlining the billing process can save doctors a lot of time. Automate billing and claims submission directly from the app. Integration with insurance systems and payment processors helps ensure revenue cycles remain smooth and free of manual errors.
Telehealth Features for Admins
Admins need the right tools to manage users, track performance, and ensure compliance. Thus, the telehealth app you build must have some essential features taht can simplify the administration process.
User Management
A simple admin dashboard is a must-have feature. This allows easy management of both patient and provider accounts. Admins should be able to view and update permissions, handle onboarding, and track activity in real time.
Robust Analytics
Data is power. Admins need insights into appointment trends, revenue cycles, patient retention, and user engagement. Thus, the telehealth platform must have built-in reporting tools that enable customizable data exports to meet various business needs.
Compliance & Audit Controls
The ability to log every action and access to patient data is an essential feature of a HIPAA-compliant telemedicine app. Admins should be able to track user activity, run security audits, and ensure that the platform is in line with all legal requirements.
Advanced Telemedicine Application Development Capabilities That Elevate Your Platform: Beyond the Basics
Basic telemedicine features get you into the game. But advanced features help you win it. Patients today are already comparing your platform with the high-end, consumer apps they use daily. That means speed, personalization, ease of navigation, and intelligence matter more than ever.
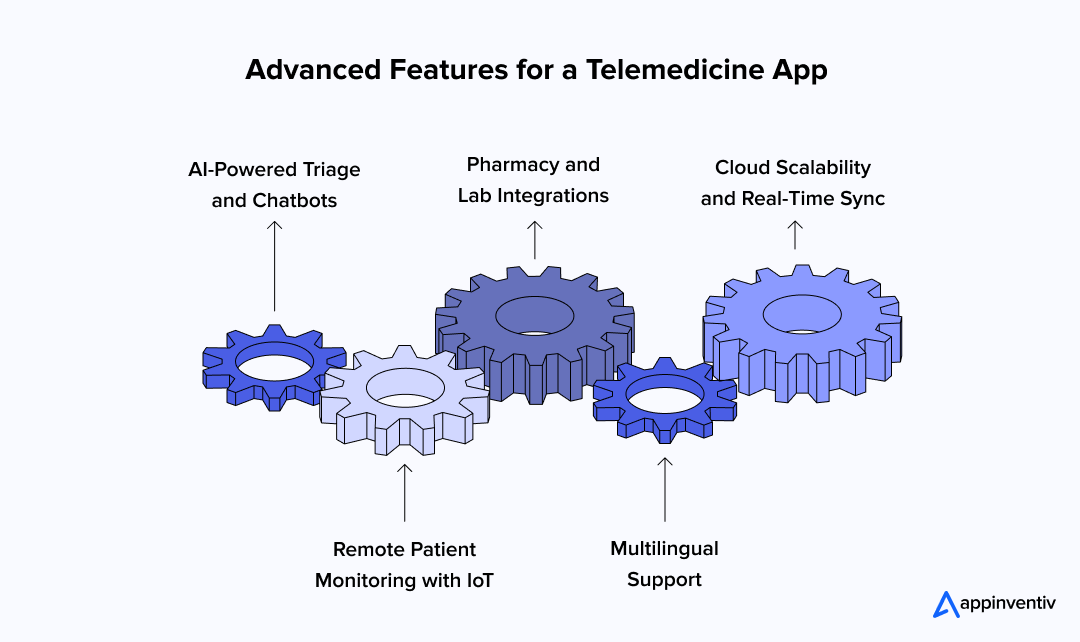
AI-Powered Triage and Chatbots
Gone are the days when AI chatbots used to be an optional functionality. Today, it has been a dire necessity to reduce patient wait times and improve operational efficiency. These bots can handle initial queries, gather symptoms, provide basic medical advice, and do a lot more. This frees up doctors to focus on more complex cases.
Also Read: What Is the Cost to Develop a Chatbot like Google’s AMIE?
Remote Patient Monitoring with IoT
Wearables and IoT-connected RPM devices can transmit real-time vital signs, such as heart rate, glucose levels, and oxygen saturation, directly to your app. This feature enables providers to access continuous, real-time data, providing a much deeper view of patient health. This feature also feeds into the growing trend of telehealth device development.
Pharmacy and Lab Integrations
Telehealth works best when it’s end-to-end. By integrating with pharmacies and labs, patients can easily refill prescriptions and receive lab results directly within the app. This experience reduces friction, improves patient satisfaction, and streamlines healthcare operations.
Multilingual Support
Expanding your reach isn’t just about geographic boundaries; it’s also about removing linguistic barriers. Offering services in multiple languages will ensure that your platform is inclusive and accessible to a broader market.
Cloud Scalability and Real-Time Sync
Video consultations and health data are not light tasks. Your platform must be capable of handling peak demand, particularly during periods of high activity. By opting for a cloud-native architecture, you ensure scalability and real-time synchronization between patients, doctors, and administrators.
Security & Compliance: Building Trust in Telemedicine from Day One
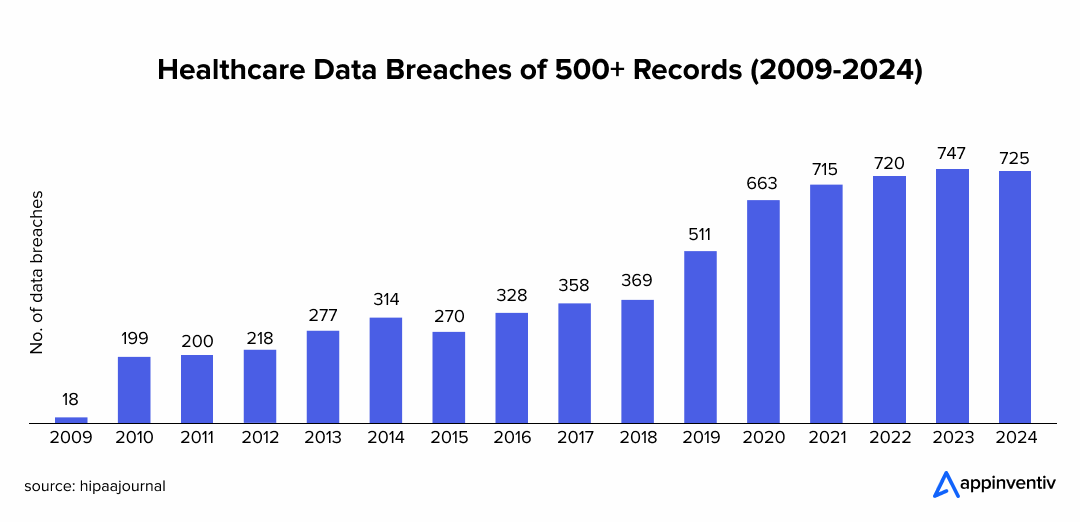
Healthcare apps don’t get second chances with trust. One breach, and patients never come back. As of January 28, 2025, 725 data breaches were reported to OCR, and out of those, over 133 million records were exposed or impermissibly disclosed. That’s not a fine; it is a business-ending risk (Source: The HIPAA Journal). That’s why secure telehealth platform development must start with compliance at its core.
Key Compliance Standards to Meet
- HIPAA (USA): Protects the storage and transfer of patient data. A must for any HIPAA-compliant telemedicine platform.
- GDPR (EU): Requires strict consent management and transparency in data usage.
- HL7 & FHIR: Standards that ensure seamless integration with EHR/EMR systems.
- HITECH: Extends HIPAA with stricter rules for electronic health records.
Security Best Practices
- End-to-End Encryption: The data encryption technique protects video calls, chats, and medical records.
- Role-Based Access: This security feature ensures only authorized staff have access to sensitive information.
- Audit Trails: Every action is logged for accountability and regulatory review.
- Secure APIs: Prevents data leaks during integrations with third-party tools.
How to Build a Successful Telehealth Application: From Idea to Launch and Scaling
Though telemedicine application development is a complex and challenging process, with a systematic approach, you can not only build a secure and scalable platform but also reduce risks and speed time-to-market. Not sure how to do it right? Well, this segment will help you walk through the steps on how to develop a telemedicine app, from concept to deployment and beyond.
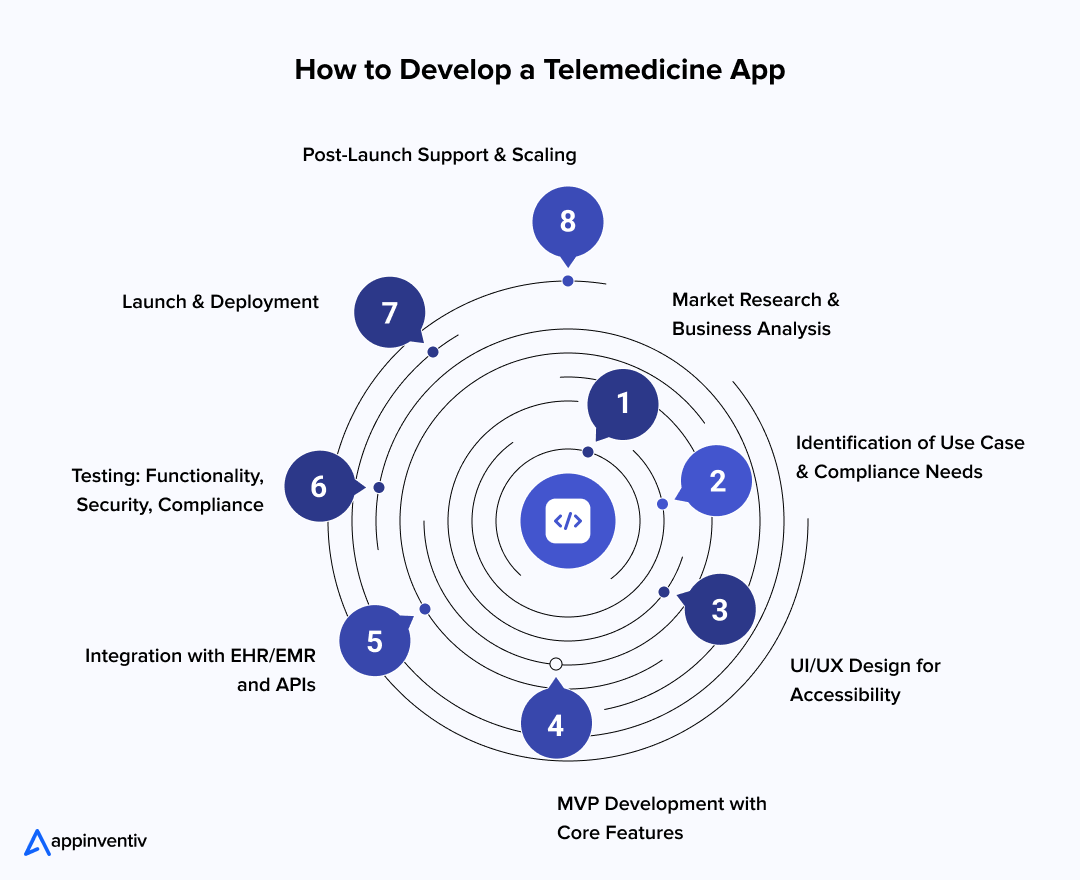
Market Research and Business Analysis
Don’t build what you think healthcare needs. Research what providers and patients actually struggle with. Doctors hate extra administrative work. Patients want convenience. Your platform must solve both problems without creating new ones.
Different medical specialties face unique regulations too. Mental health apps deal with different compliance rules than general practice platforms. International markets add another layer of complexity. Plan for these early or pay for expensive fixes later. Check competitor reviews, and users complain about real problems there.
Define Use Cases and Compliance Needs
Write detailed user stories that capture real workflows. “I want to schedule appointments” is too vague. “As a working parent, I need same-day pediatric consultations after 5 PM” gives you actual requirements to build against.
List every regulation that applies. HIPAA, state licensing, prescription rules – missing one can kill your project. Plan compliance early or rebuild later.
Craft UI/UX Design for Healthcare Environments
Healthcare users are not typical app users. Elderly patients need bigger buttons and clearer instructions. Busy doctors need workflows that don’t waste their time. Design for both without making compromises that hurt either group.
Accessibility isn’t just about compliance; it expands your market. Screen readers, keyboard navigation, and proper color contrast help everyone, not just users with disabilities. They often become the reason healthcare organizations choose your platform over those of your competitors.
Most patients will use your app on their phones. Most doctors prefer larger screens for detailed work. Your design needs to work well on both without feeling like a compromise on either platform.
Develop an MVP with Core Features
When starting with a Minimum Viable Product (MVP), start with the basics that prove users actually want your service. Video calls, scheduling, user profiles, and payment gateway integrations; get these essential features right before adding fancy AI features or device integrations.
Healthcare projects work well with agile development. Short sprints enable you to adapt quickly when regulations change or user feedback reveals issues. Regular check-ins with stakeholders catch compliance issues while they’re still inexpensive to fix.
Build your APIs first, then your interfaces. This approach makes it easier to add mobile apps, web portals, and partner integrations later without rebuilding everything from scratch.
Integrate with EHR/EMR and APIs
EHR integration is challenging but essential. EHR integration makes or breaks healthcare platform adoption. Doctors won’t use platforms that create extra work. Providers won’t use systems that force them to duplicate data entry or switch between multiple applications during patient visits.
Thus, connect your app with existing hospital records and billing systems. Use FHIR APIs to keep data consistent and secure. Often, integration complexity exceeds initial estimates, so ensure you allow buffer time in your project plan.
Test the App for Functionality, Security, and Compliance
Healthcare testing is life-or-death serious. Test with actual providers during clinic hours to see real performance. Hire security specialists familiar with healthcare threats. Healthcare data sells for 50x more than credit cards on dark markets.
Get third-party compliance audits. Enterprise customers need proof that your platform meets regulations.
Launch & Deploy the Telehealth Platform
Roll out gradually. Start with small provider groups, identify problems, then expand. Deploy across iOS, Android, and Web. Ensure you meet app store guidelines, especially around privacy and security disclosures. App store approval takes longer for healthcare apps. Submit early and expect multiple review rounds.
Post-Launch Support & Scaling
Monitor 24/7. Medical emergencies don’t follow business hours. Gather feedback from patients and providers. Providers complain directly. Patients suffer silently. Watch usage patterns for hidden problems.
Plan for ongoing compliance updates and scale your cloud infrastructure to handle peak demand.
Also Read: The Essential Guide to Healthcare Mobile App Development
Choosing the Right Tech Stack for Telemedicine App Development
Choosing the right tech stack makes the difference between a scalable platform and one that fails under pressure. In telemedicine app development, the stack must balance performance, security, and future adaptability. Here’s a breakdown of the tech stack used in telemedicine app projects today:
| Layer | Recommended Tools/Frameworks | Why It Matters |
|---|---|---|
| Frontend | React Native, Flutter, Swift (iOS), Kotlin (Android) | Delivers smooth cross-platform apps with responsive interfaces. |
| Backend | Node.js, .NET, Python, Java | Ensures scalability, flexibility, and fast response times for heavy workloads. |
| Database | PostgreSQL, MySQL, MongoDB | Handles sensitive health records with reliability and speed. |
| Cloud Hosting | AWS, Azure, Google Cloud | Offers HIPAA-compliant infrastructure with elastic scalability. |
| APIs | Twilio (video), Stripe/PayPal (payments), Redox/FHIR (EHR) | Adds secure video, payments, and medical data interoperability. |
| Security Layer | OAuth 2.0, JWT, SSL/TLS | Protects data with authentication, encryption, and safe transactions. |
Expert Insight: For custom telemedicine app development solutions, the right combination depends on your specific project needs and business goals, whether you are building a lightweight consultation app or a full-scale hospital platform.
Sourcing Models for Telemedicine App Development: Freelancers vs. In-House vs. Outsourcing
How you build a telehealth app is as important as what you build. Businesses exploring custom telemedicine app development usually choose one of three sourcing models:
In-House Development
You hire your own team of developers, designers, and compliance experts. This gives you full control and alignment with your vision. But it’s expensive and slow. Recruiting HIPAA-savvy engineers is not easy.
Freelancers
Freelancers are cheaper and faster to onboard. But they come with risks such as a lack of healthcare domain expertise, uneven quality, and compliance gaps. For regulated industries like healthcare, this route is often too risky.
Outsourcing to a Healthcare Mobile App Development Company
Partnering with a specialized telehealth app development company strikes the balance. You get scalability, proven expertise, and faster time-to-market. Most importantly, these firms already understand compliance frameworks like HIPAA, GDPR, and HL7.
Comparison of Different Sourcing Models for Telemedicine App Development
| Sourcing Model | Pros | Cons | Ideal For |
|---|---|---|---|
| In-House Development |
|
| Large companies with long-term projects |
| Freelancers |
|
| Startups or small projects with tight budgets |
| Outsourcing |
|
| Enterprises needing expert help and quick results |
Expert Insight: For enterprises, outsourcing is usually the smarter option. It lets you focus on strategy while experts handle execution and compliance.
The next step in healthcare innovation starts with you. Discuss your app development journey with us and shape your telemedicine vision now.
Challenges in Telehealth App Development & How to Overcome Them
Telehealth has promise, but execution isn’t simple. Businesses often underestimate the hurdles, which result in costly penalties later. To help you steer away from such situations, here is a breakdown of the most common challenges and how to develop a telemedicine app to avoid them.
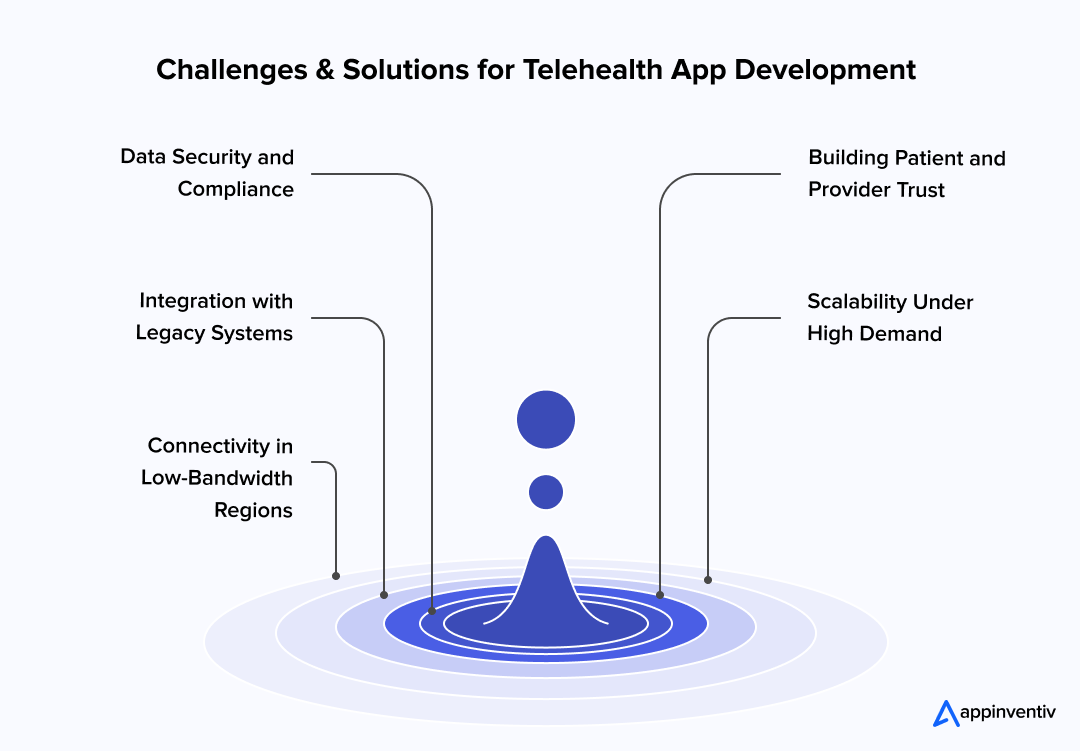
1. Data Security and Compliance
Challenge: Healthcare data is the top target for cyberattacks. A single breach can ruin trust and invite fines.
Solution: Build the telehealth app with a compliance-first design, end-to-end encryption, role-based access controls, audit trails, and HIPAA-ready hosting.
2. Integration with Legacy Systems
Challenge: Many hospitals still run on outdated IT. Integrating telehealth with EHRs can feel like forcing two different worlds together.
Solution: Use FHIR-based APIs and middleware. They bridge old systems with new apps smoothly.
3. Connectivity in Low-Bandwidth Regions
Challenge: Patients in rural areas face dropped calls or lag during consultations. That hurts adoption.
Solution: Adaptive video streaming, offline functionality, and lightweight design improve accessibility.
4. Building Patient and Provider Trust
Challenge: Not everyone is ready for virtual visits. Some people, particularly elderly ones, are more comfortable with in-person visits. Trust is fragile.
Solution: Focus on UX simplicity. Add patient education modules. Train providers to blend digital with in-person care.
5. Scalability Under High Demand
Challenge: Scalability is a major challenge. COVID-type pandemics or seasonal spikes (like flu season) can overwhelm servers.
Solution: Cloud-native, microservices architecture with auto-scaling ensures you’re always ready for demand surges.
Real-World Examples: Telemedicine App Success Stories That Inspire
Real adoption stories prove the business case for telemedicine mobile app development. The most successful platforms share three traits: trust, scalability, and compliance.
Teladoc Health
Teladoc is a leader in virtual care with over 55 million members across 175+ countries. Its strength lies in scale, covering general care, chronic conditions, and even mental health on one platform.
Also Read: Cost to Develop an App Like Teladoc
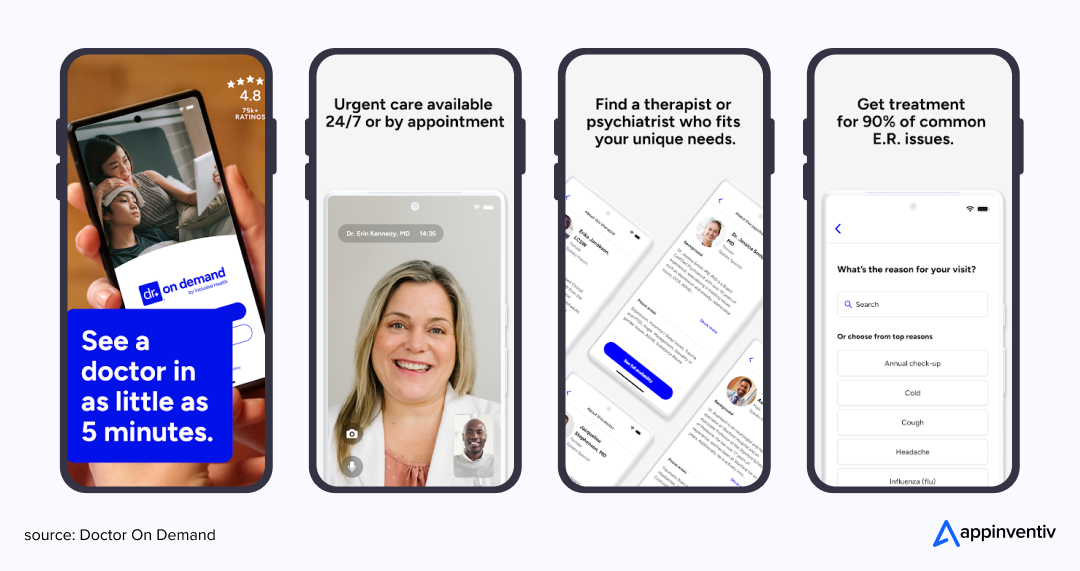
Doctor on Demand
Doctor on Demand app expanded into chronic care management with remote patient monitoring tools. Patients track vitals through wearables while doctors monitor them remotely.
MDLIVE (acquired by Cigna)
Offers 24/7 urgent care and behavioral health. It integrates insurance claims directly into the app, showing how business models can align with patient convenience.
How Much Does Telehealth App Development Cost?
Let’s talk about money. The cost to develop a telehealth mobile app development project isn’t a flat fee. It’s a spectrum, and it depends on a few key factors.
- Complexity: A basic MVP with just a video chat feature will cost far less than a platform with AI-powered diagnostics and telehealth device development integrations.
- Features: The more features you add, the higher the cost. Features like EHR integration and IoT connectivity can be particularly expensive.
- Team Location: The hourly rate of a development team in the U.S. will be much higher than that of a team in Eastern Europe or India.
- Platform Choice: The platform you choose, iOS, Android, or Web, affects the telemedicine mobile app development cost.
- User Roles: More roles (patients, doctors, admins, insurers) = higher build cost.
- UI/UX Design: Offering enhanced accessibility features or multilingual support will require more design effort, which in turn drives up costs.
- Compliance Implementation: Ensuring compliance with HIPAA, GDPR, HL7, and FHIR standards adds both legal and technical costs.
Here’s the breakdown of telemedicine app development costs and timeline based on the project’s complexity level.
| App Type | Estimated Cost Range | Estimated Timeline |
|---|---|---|
| MVP (core features) | $40,000 – $100,000 | 4 to 6 months |
| Moderate apps | $100,000 – $200,000+ | 6 to 8months |
| Advanced apps | $200,000 – $400,000+ | 8 to 12+ months |
| Enterprise-level platforms | $400,000 – $600,000+ | 12 to 18+ months |
What Are The Common Monetization Approaches For Telemedicine Apps?
Now that you have a clear idea of the telemedicine app development costs, it’s time to think about how your telemedicine app will make money. The right monetization strategy ensures your app not only serves its users but also generates lucrative ROI. Let’s dive into the most popular ways to monetize telemedicine apps.
Subscription Model
Users (patients or healthcare providers) pay a recurring fee, either monthly or annually, for access to the app’s services. This is ideal for platforms offering ongoing care, wellness programs, or premium features.
Pay-Per-Consultation
In this model, users pay each time they schedule a consultation or use specific features. This is common for apps offering urgent care, one-time consultations, or specialized services like mental health therapy.
Enterprise Licensing
Businesses or healthcare organizations can purchase licenses for their staff, patients, or members. This model is best for large clinics, hospitals, or corporations that want to integrate telehealth services into their operations.
Freemium Model
Basic services are provided for free, while premium features, such as extended consultations, priority scheduling, or specialized care, are available for a fee. This model helps attract a larger user base while generating revenue from advanced features.
Emerging Trends and the Next Wave of Telehealth Platforms
Telehealth is evolving fast. What feels advanced today will be standard in a few years. Here’s what’s shaping the future trends in telemedicine application development:
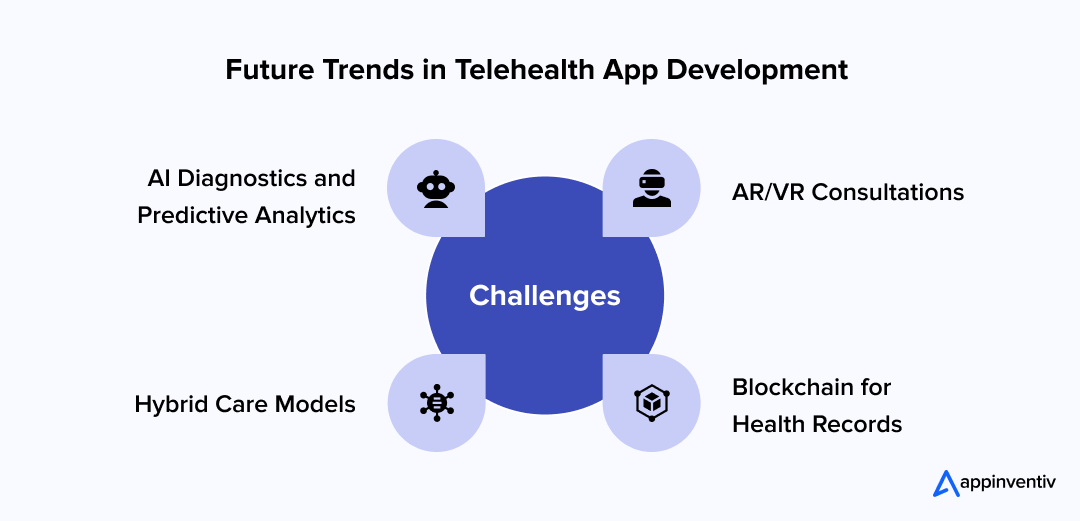
- AI Diagnostics and Predictive Analytics
AI in telemedicine platforms will move from triage to diagnostics. Think early cancer detection or predictive heart risk assessments, built into the app. - AR/VR Consultations
From virtual therapy to surgical assistance, immersive technologies are finding a home in remote care. - Blockchain for Health Records
Secure, immutable storage of patient data will reduce fraud and strengthen patient control. - Hybrid Care Models
The most effective platforms will blend telehealth with physical care, offering flexibility instead of a digital-only approach.
With new future trends in healthcare technology like AI diagnostics and remote patient monitoring, building a secure, scalable telemedicine platform is crucial for staying ahead.
With new trends like AI diagnostics and remote patient monitoring, it’s crucial to stay ahead. Get in touch to start your project today!
How Appinventiv Can Help You Build a Secure, Scalable Telehealth Platform
Telemedicine mobile app development isn’t just another app project. It demands domain knowledge, compliance expertise, and scalable architecture. That’s where Appinventiv comes in.
As a reputed healthcare mobile app development company, we’ve delivered over 3,000 digital solutions, including secure and compliant telemedicine platforms.
Why Partner With Us
- 10+ years of healthcare expertise building HIPAA-ready healthcare apps.
- A team of 1600+ developers, skilled in AI, IoT, blockchain, cloud, and other tech trends.
- CMMI Level 2 and ISO-certified processes ensure quality and compliance.
- Recognized by Deloitte, Statista, Clutch, and Times Business Awards for tech excellence.
- Proven track record with healthcare leaders like Soniphi, Health-e-People, and DiabeticU.
To bring our insights into focus, here are four standout healthcare projects where we turned healthcare vision into reality. Each case delivers tangible outcomes through innovation, compliance, and performance.
Health-e-People Assessment App: Unified Health Insights
Imagine consolidating data from over 200 devices into one health profile. Our client’s project Health‑e‑People does exactly that, combining wearable data, caregiver connections, and predictive analytics.
The result: streamlined clinical decision making, improved patient care, and support for medical research.
DiabeticU: Secure, Scalable Diabetes Management
We developed DiabeticU, a HIPAA-compliant platform for tracking blood glucose levels, medications, meal plans, and facilitating remote consultations.
The outcome? Development of an app that supports scalable growth, zero security incidents, and enhanced patient engagement.
YouCOMM Health App: Enhancing In-Hospital Care
We tackled the inefficiencies in call bell systems. With YouCOMM, patients can summon nurses via voice, head gestures, or simple selections, right from their bedside.
The result? A 60% improvement in nurse response time and early adoption across multiple U.S. hospital chains.
Soniphi Vitality Health App: Wellness via Voice
We developed Soniphi, which captures 94% of voice resonance data to assess user vitality. The challenge: filtering ambient noise and extracting meaningful health signals from voice alone.
The outcome: a bioacoustic system adopted by millions for proactive wellness monitoring.
These case studies prove choosing Appinventiv means more than hiring a tech partner. It means working with a telehealth app development company that understands regulations, scalability, and patient trust.
So, why wait? Partner with Appinventiv now and take your telemedicine vision to the next level.
FAQs
Q. Can I develop a cross-platform telemedicine app?
A. Yes, absolutely, and it’s a brilliant idea. A few years ago, you had to choose between building an app for Apple or for Android, or spend a fortune creating two separate apps. Now, thanks to modern frameworks like Flutter and React Native, that’s no longer the case.
Think of it like this: these frameworks let you write the code once and deploy it on both iOS and Android. It’s a huge time-saver and a major win for your budget. You get to reach a wider audience right out of the gate, and managing a single codebase makes ongoing updates and maintenance so much easier. You’re not just saving money; you’re future-proofing your product.
Q. How do you build a telemedicine platform?
A. Telemedicine app development is a journey, not a single step. You can’t just jump straight into coding. It’s all about following a clear roadmap to make sure your app is not only functional but also safe, legal, and truly useful.
Here’s the path we typically follow:
- Start with Why: Before anything else, you need a clear vision. Who is this app for? What problem are you solving? This is the “research and discovery” phase, where we define your unique purpose.
- Lock Down Compliance: This is the most critical part. You have to get the regulatory and security requirements right from the beginning. We’re talking about HIPAA and GDPR. It’s non-negotiable and requires a “security-by-design” approach.
- Design for Humans: Your app has to be intuitive and accessible for everyone, from a tech-savvy physician to an elderly patient. This is where user experience (UX) and user interface (UI) design become crucial.
- Build the MVP: Instead of building everything at once, we start with a Minimum Viable Product (MVP). It has the core features you need to get to market quickly, test your idea with real users, and then iterate based on their feedback.
- Integrate and Connect: The real power of a telemedicine app lies in its connections. We integrate essential APIs for things like secure video calls, payment processing, and linking up with existing electronic health record (EHR) systems.
- Test, Test, Test: This is where we break things to make sure they won’t break on your users. We test everything: security, performance, and usability to ensure the app is rock-solid.
- Launch and Evolve: After a successful launch, the work isn’t over. A successful app is always evolving. We monitor performance and feedback to plan for future updates and improvements.
Q. How is telemedicine transforming clinics and hospitals?
A. Telemedicine is doing more than just adding a video chat option; it’s fundamentally changing how clinics and hospitals operate. It’s a total game-changer for everyone involved.
- For the Clinic: It’s all about efficiency. Telemedicine dramatically reduces waiting times and no-shows, and it helps clinics utilize their staff and resources more effectively. A doctor can manage a follow-up appointment with a patient from anywhere, which frees up clinic space and streamlines their day. It’s a more profitable model for them.
- For the Patient: The benefits are enormous. Telehealth makes care more convenient and accessible. It’s a lifesaver for patients in rural areas or those with mobility issues. And with features like remote monitoring and automated follow-ups, patients feel more connected and engaged in their own care, which leads to better health outcomes in the long run.
Q. How much does it cost to develop a telehealth application?
A. That’s the million-dollar question, right? The honest answer is that it varies a lot, but you can think of it as a spectrum. Here is an average breakdown of telehealth application development costs.
- For an MVP: A basic, no-frills app with essential features like video calls and scheduling might run you anywhere from $40,000 to $100,000. This is the best way to get started if you’re on a tight budget.
- For a Feature-Rich Platform: If you want a full-scale, enterprise-grade platform with advanced features like AI-powered chatbots, IoT integration for remote monitoring, and complex data analytics, the cost can go up to $600,000 or more.
What really drives the price? The complexity, the number of features, the level of security and compliance you need, and, of course, where your development team is located.
Q. How long does it take to develop a HIPAA-compliant telemedicine platform?
A. When it comes to building a HIPAA-compliant platform, you have to be patient because security takes time.
- For an MVP, you’re looking at a timeline of about 4 to 6 months. This includes the time spent on strategic planning, design, core development, and the crucial step of rigorous security testing to ensure compliance.
- For a full-scale, enterprise app, that timeline extends to 12 to 18 months or longer. This is because you’re adding more complexity, more features, more integrations with EHR systems, and more layers of security, all of which require extensive testing to make sure everything is watertight.
Rushing this process is not an option. A HIPAA violation can come with huge fines and destroy a company’s reputation overnight.
Q. How do I make a telehealth app secure?
A. Think of security as the foundation of your house. If it’s not solid, the whole structure is at risk. For a telehealth app, security isn’t a feature you add at the end; it’s a core philosophy.
Here are the key principles:
- Encryption is Everything: All data, whether it’s a video call or a patient’s medical history, must be encrypted. This makes it unreadable to anyone who isn’t authorized to see it. It’s like using a secret code that only the right people can decipher.
- Access Control: The rule here is simple: “need to know.” Only people with the right permissions should be able to access specific data. A doctor can see their patients’ records, but they can’t access another doctor’s patient list. This is called role-based access.
- Secure APIs: Every time your app communicates with a server or another system, it needs to be through a secure channel. We use APIs with strong authentication to make sure no one can eavesdrop on that conversation.
- Partner with the Pros: Don’t try to do this yourself. You need to work with developers who are experts in secure telehealth platform development and have a track record of handling sensitive health information. They know the ins and outs of building a secure, compliant platform.
Q. How do I ensure HIPAA/GDPR compliance in a telemedicine app?
A. Ensuring HIPAA and GDPR compliance isn’t a checklist you tick off; it’s a deep commitment to protecting patient privacy. You have to build it into the DNA of your app.
- Explicit Consent: Your app must get explicit, documented consent from patients before it can collect or share their data. And this process has to be transparent; no fine print or confusing language.
- Audit Trails: Every single action taken on your platform, from a user logging in to a doctor viewing a patient’s chart, must be logged. If anything ever goes wrong, you need a full record of who did what and when.
- Certified Hosting: You can’t just host your data anywhere. You have to use a certified cloud provider like AWS or Azure that offers HIPAA-compliant infrastructure. These services are built with the necessary security controls to protect sensitive data.
- Partner Legally: When you work with a development company, they must sign a Business Associate Agreement (BAA). This is a legal contract that obligates them to protect patient data and ensures you’re not held solely responsible if something goes wrong.
Q. How will AI agents and automation help in telemedicine?
A. AI agents and automation will make telemedicine faster and more efficient. They can help schedule appointments, remind patients about their visits, and even answer simple health questions. Automation can also help doctors track patient progress and analyze health data more easily. This will save time and allow doctors to focus on more important tasks, improving care for patients.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How to Build a Custom Pediatric EMR and EHR System?
Key takeaways: Clinical Precision: Custom systems accommodate pediatric-specific data points like percentile curves and weight-based longitudinal dosing. Interoperability: Seamless data exchange via HL7 FHIR ensures your practice stays connected to pharmacies, labs, and state registries. Regulatory Resilience: Built-in compliance with HIPAA, HITECH, and MACRA/MIPS reduces legal friction. Enhanced Engagement: Parent portals reduce administrative overhead by…

Change Management in Healthcare: Principles, Processes, and Models
Key Takeaways Change in healthcare fails quietly when ownership, workflow alignment, and follow-through are missing. Successful change management in healthcare focuses on adoption, not just system implementation. Clinical workflows and workforce capacity determine whether transformation sticks or stalls. Governance, clear accountability, and post-go-live support matter more than the model used. Sustainable healthcare transformation depends on…
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…