- Why EHR Optimization Is a Strategic Priority in 2026?
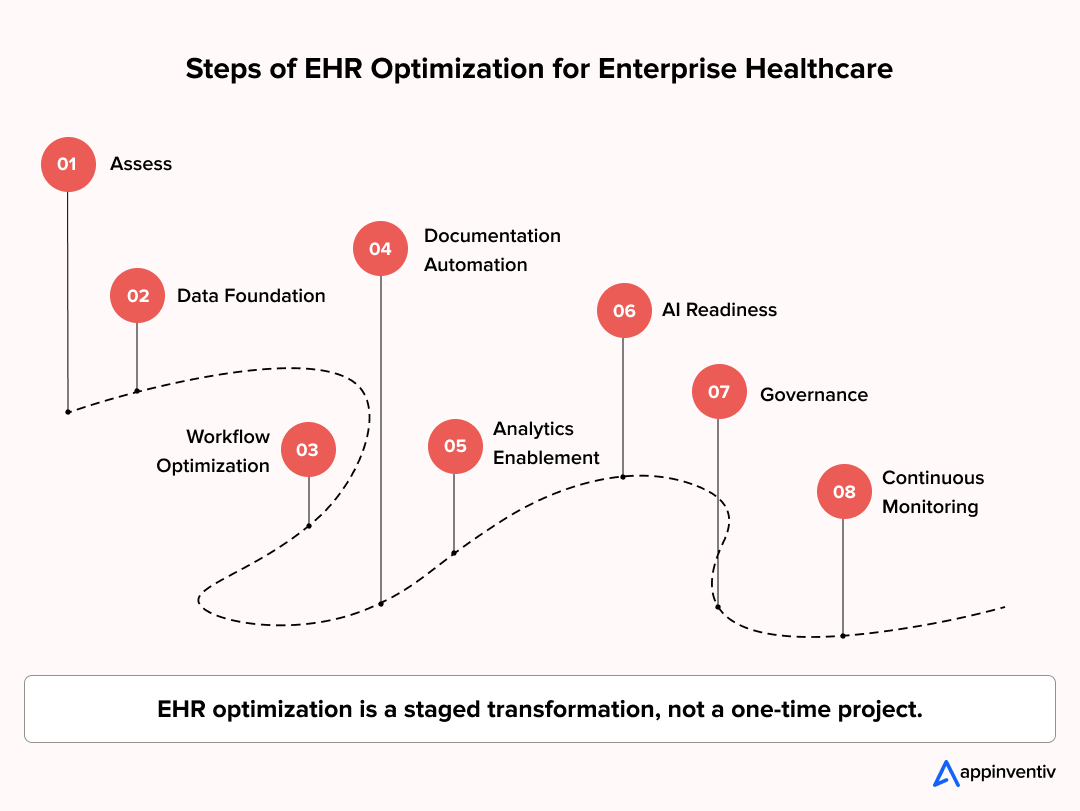
- What Are the Key Aspects of EHR Optimization for Enterprise Healthcare?
- Workflow Intelligence and Role-Based Experience
- Interoperability and Data Liquidity
- Clinical Documentation Acceleration
- Analytics and Clinical Intelligence Readiness
- Security, Privacy, and Compliance Architecture
- AI Enablement Layer
- Common EHR Bottlenecks: Legacy vs Optimized Workflows
- How Do Technology and Security Enhancements Strengthen EHR Optimization?
- Security Measures Enterprises Prioritize
- Technology Enablement for Security Operations
- Scalability via Microservices and Cloud-Native EHR Architecture
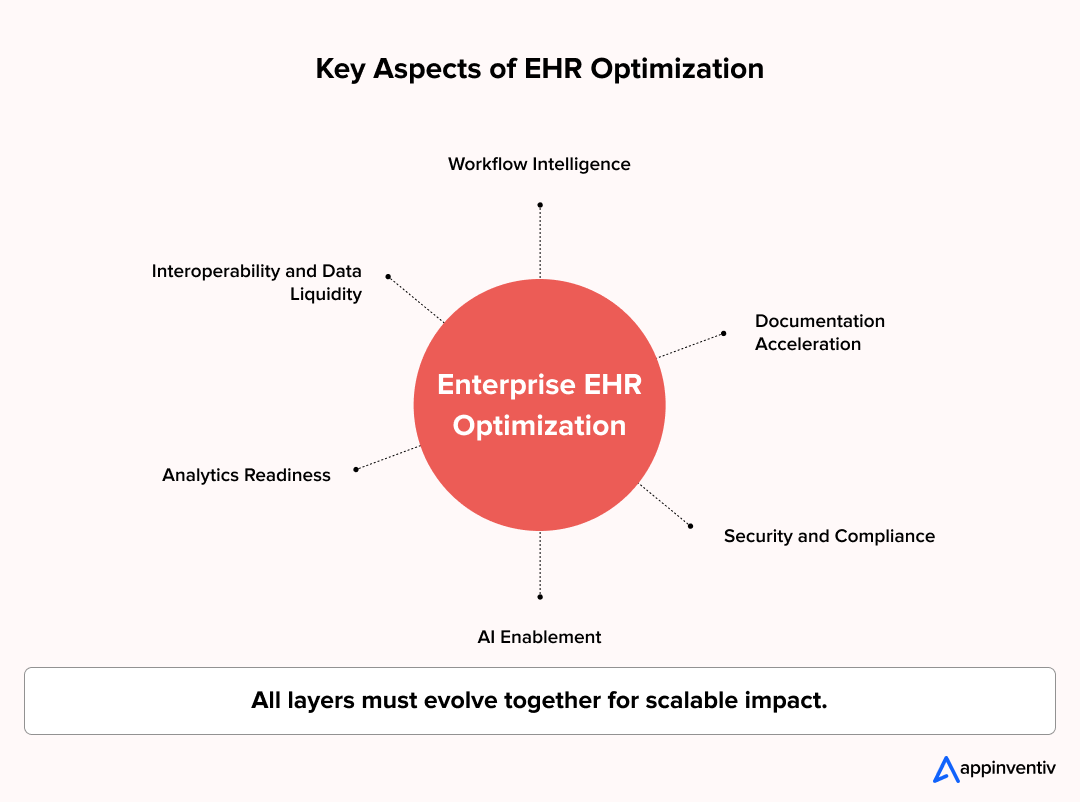
- What Does an Enterprise EHR Optimization Plan Look Like in Practice?
- Step 1: Baseline Assessment and Workflow Mapping
- Step 2: Data Architecture and Interoperability Strategy
- Step 3: Workflow and Interface Optimization
- Step 4: Documentation and Automation Acceleration
- Step 5: Analytics and Clinical Intelligence Integration
- Step 6: AI Readiness Enablement
- Step 7: Governance, Training, and Change Management
- Step 8: Continuous Performance Monitoring
- How Do Governance and Management Drive Enterprise EHR Optimization?
- What Enterprise Governance Structures Include
- Management Practices That Sustain Momentum
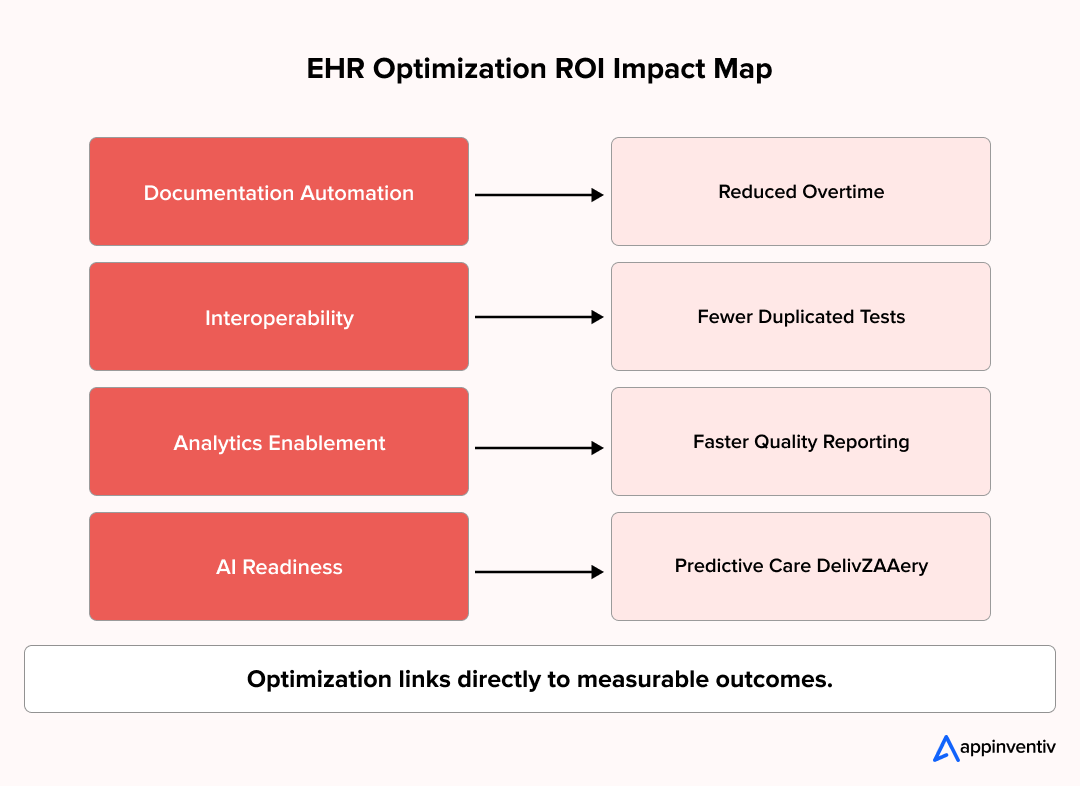
- Which EHR Optimization Strategies Deliver Measurable ROI?
- Specialty-Specific Configuration
- Clinical Decision Support Tuning
- Ambient and Voice-Based Documentation
- Revenue Cycle and Coding Optimization
- Interoperability Expansion
- AI-Powered Triage and Risk Scoring
- What Real World EHR Optimization Use Cases Show Enterprise Impact?
- Cleveland Clinic, USA: Streamlined nursing documentation
- Royal Children’s Hospital Melbourne: Mobile EHR at the bedside
- Hamad Medical Corporation, Qatar: Training-led optimization
- How Does EMR Cost Optimization Deliver Financial Impact?
- Key Cost Drivers in EMR Cost Optimization
- How Does NextGen EHR Optimization Enable AI-Driven Healthcare Evolution?
- Where Nextgen EHR Optimization Is Heading?
- What Enterprises Must Build To Support AI
- In-House vs Outsourced Models for EHR Optimization Support
- What Challenges Do Enterprises Face While Optimizing EHRs?
- Legacy Data Fragmentation
- Clinician Resistance to Change
- Over-Customization Debt
- Integration Sprawl
- Governance and Ownership Gaps
- What Are the Benefits of EHR Optimization for Healthcare Enterprises?
- Stronger EHR Efficiency Across Clinical Teams
- Improved Patient Experience and Continuity of Care
- Better Data Governance and Decision Intelligence
- Financial and Revenue Performance Gains
- AI-Ready Healthcare Operations
- Why Choose Appinventiv for Enterprise EHR Optimization?
- Frequently Asked Questions
Key Takeaways
- EHR optimization shifts healthcare systems from digital records to intelligent clinical operations.
- Workflow, data, security, and AI readiness drive sustainable EHR efficiency.
- Structured optimization roadmaps reduce clinician burden and improve care delivery outcomes.
- Interoperability and data liquidity unlock value-based care and advanced analytics.
- Security, governance, and compliance ensure scalable and risk-resilient EHR transformation.
Most healthcare leaders I speak with describe the same moment. The EHR is live. The rollout happened years ago. Clinicians are using it every day. Yet somewhere between the morning clinic rush and the end-of-day backlog, the system feels like it is working around your teams instead of with them.
That is where many US healthcare enterprises stand today. EHR adoption is no longer the milestone. EHR efficiency is.
In 2026, the difference between high-performing care networks and struggling ones often comes down to how well their digital backbone supports clinical work, data flow, and decision-making. An EHR that slows documentation, traps data in silos, or resists interoperability quietly erodes patient experience, clinician satisfaction, and operational margins. You see it in overtime hours. You feel it in delayed analytics. You hear it in physician frustration.
This is why EHR optimization in healthcare has shifted from an IT improvement project to a board-level strategy. Healthcare EHR optimization today is about reshaping workflows, unlocking data liquidity, preparing for AI-driven care models, and strengthening EHR for patient care at scale. It is not about adding features. It is about making the system finally work the way your organization needs it to.
This guide walks through how enterprises approach optimization of EHR with technical depth, practical steps, and measurable outcomes in mind. The goal is simple. Help your healthcare offering run smarter, faster, and ready for what comes next.
94% hospitals use EHRs, but few achieve true efficiency
Why EHR Optimization Is a Strategic Priority in 2026?
Not long ago, EHR conversations lived inside IT teams. Today, they appear in executive reviews and clinical leadership meetings. The reason is simple. The EHR now runs the operational core of healthcare enterprises.
The market reflects this shift. The global electronic health records market is projected to grow from USD 29.84 billion in 2025 to USD 45.55 billion by 2035, with an expected CAGR of 4.32%. Investment is rising because healthcare organizations know digital records alone are no longer enough. EHR optimization for healthcare efficiency and performance now define competitive advantage.
If your organization is pursuing growth, value-based care, or AI adoption, your EHR becomes either the accelerator or the constraint. There is no middle ground.
Several forces are driving this urgency.
Regulatory and Interoperability Pressure
US healthcare is moving toward enforced data sharing.
- TEFCA is expanding nationwide exchange expectations.
- FHIR APIs are standard for payer and provider connectivity.
- Information blocking penalties create operational risk.
- Audit readiness for data traceability is under tighter scrutiny.
Unoptimized systems struggle here. Integration backlogs grow. Compliance teams spend time addressing gaps rather than advancing capabilities.
Clinician Time as a Cost Center
Enterprises now measure documentation burden in dollars.
- Excess clicks extend patient visits.
- After-hours charting increases over time.
- Inefficient workflows delay throughput.
EHR workflow optimization directly impacts staffing cost and retention.
Value-Based Care and AI Readiness
Outcome-based reimbursement and clinical AI both rely on clean, real-time data. Without EHR data optimization, analytics stall and AI pilots fail to scale.
Rising Patient Expectations
Patients expect unified records, faster coordination, and seamless digital access. These are the expectations shaped by the evolution of mHealth applications and consumer health technology. Nextgen EHR optimization now influences satisfaction and loyalty for patient care across facilities.
In 2026, healthcare EHR optimization decides whether your organization operates as a connected care network or a set of disconnected departments. Organizations looking to implement a comprehensive EHR optimization strategy can benefit from understanding the entire transformation landscape.
What Are the Key Aspects of EHR Optimization for Enterprise Healthcare?
At some point, most enterprise healthcare teams realize the same thing. Buying a leading EHR platform did not automatically deliver efficiency, interoperability, or intelligence. The real gains come from how the system is shaped after go-live.
EHR optimization for healthcare efficiency succeeds when multiple layers evolve together. Not just interfaces. Not just workflows. The full operating model.
Below are the key aspects that separate surface-level tuning from enterprise-grade transformation.
Workflow Intelligence and Role-Based Experience
Clinicians do not work in generic screens. Neither should EHRs. Effective EHR workflow optimization focuses on:
- Role-based interfaces for physicians, nurses, care coordinators, and billing teams.
- Specialty-specific templates and order sets.
- Reduced navigation depth for high-frequency tasks.
- Context-aware clinical prompts instead of static alerts.
A common example. Emergency departments often redesign triage documentation flows to cut assessment time per patient. Small changes here scale into major throughput gains across hospital networks.
Interoperability and Data Liquidity
Modern care delivery is distributed. Data must move just as fast. Achieving true interoperability in healthcare requires strategic planning across technical, semantic, and organizational layers. EHR data optimization at enterprise scale requires:
- FHIR-based APIs for external data exchange.
- SMART on FHIR frameworks to securely embed third-party clinical and AI applications inside the EHR environment.
- TEFCA-aligned network connectivity.
- Integration with labs, imaging, pharmacies, payers, and HIEs.
- Unified patient identity management across facilities.
Without this layer, care teams waste time hunting records. Analytics teams waste time reconciling data sources. Interoperability stops being a technical goal and becomes an operational necessity.
Clinical Documentation Acceleration
Documentation is still the single largest friction point inside most EHR environments. Optimization efforts here include:
- Specialty-aligned note structures.
- Voice-based and ambient documentation tools.
- Auto-population from prior encounters.
- Real-time coding assistance.
This is where EHR efficiency becomes visible to clinicians. Fewer clicks. Less after-hours charting. More time in front of patients.
Analytics and Clinical Intelligence Readiness
An optimized EHR is not only a record system. It is a data engine. Key focus areas:
- Standardized data models.
- Real-time clinical dashboards.
- Quality measure automation.
- Population health data pipelines.
- Research and registry data extraction.
Without this foundation, advanced reporting and AI initiatives remain manual and slow.
Security, Privacy, and Compliance Architecture
Optimization cannot compromise trust. Enterprise healthcare EHR optimization must reinforce:
- HIPAA-aligned access controls.
- Zero-trust security models.
- Fine-grained audit trails enhanced by emerging technologies like blockchain in healthcare for immutable record-keeping.
- Encryption across data at rest and in transit.
- Controlled third-party API access.
Security teams increasingly evaluate EHR changes as part of enterprise risk posture, not application-level checklists.
AI Enablement Layer
Many organizations want AI copilots, predictive risk models, and clinical decision support. Few prepare the groundwork. Successful AI integration in EHR systems starts with:
- Clean and structured data.
- Stable integration interfaces.
- Defined data governance policies.
- Monitoring of model outputs inside clinical workflows.
Without this, AI pilots remain isolated demos instead of embedded clinical tools.
Key aspects of EHR optimization strategy work like interlocking gears. Workflow improvements depend on data liquidity. AI enablement depends on analytics readiness. Security touches every layer. Enterprises that address these aspects together see durable gains. Those who treat them separately end up with scattered improvements that never scale.
Common EHR Bottlenecks: Legacy vs Optimized Workflows
Most EHR inefficiencies hide in daily clinical routines. A few extra clicks. A delayed record lookup. A manual workaround. Over time, these bottlenecks compound into lost productivity and clinician fatigue.
The table below highlights where legacy workflows slow enterprises down and how optimized environments remove friction.
Legacy vs Optimized EHR Workflows
| Workflow Area | Legacy Experience | Optimized Experience |
|---|---|---|
| Clinical documentation | Manual entry and long templates | Voice and ambient documentation with auto-populated fields |
| Order management | Multiple screens and confirmations | Streamlined order sets with context-aware prompts |
| Patient record access | Fragmented data across systems | Unified longitudinal patient view |
| Interoperability | Custom point-to-point interfaces | FHIR-based API data exchange |
| Alerting | High volume of low-value alerts | Context-driven clinical decision support |
| Analytics reporting | Manual extraction and delayed reports | Real-time dashboards and automated reporting |
| Identity management | Separate logins across tools | Unified identity and single sign-on |
| Downtime handling | Manual fallback processes | Automated failover and high availability |
Key takeaway: Optimized workflows return clinician time, reduce error risk, and improve care continuity at scale.
How Do Technology and Security Enhancements Strengthen EHR Optimization?
Most healthcare leaders have experienced a security review that raised uncomfortable questions. A shared workstation left logged in. A mobile device used across shifts. An audit that took longer than expected. These moments highlight a simple reality. Optimization cannot succeed without strong compliance and security foundations.
As clinical workflows become more connected and mobile, healthcare IT security must protect data without slowing care delivery. Organizations building or modernizing their platforms should understand the fundamentals of EHR software development with security built in from the ground up.
Security Measures Enterprises Prioritize
Enterprises focus on security measures that protect patient data without slowing clinical workflows.
- HIPAA compliance embedded into clinical workflows.
- Identity management solutions that unify user access across facilities.
- Role-based access and multi-factor authentication.
- Access and authentication controls for shared mobile devices.
- Continuous monitoring for unauthorized access attempts.
- Audit trails that support annual compliance reviews.
Security improvements must also reduce workflow disruptions. Single sign-on, biometric logins, and intelligent session timeouts allow clinicians to move quickly without compromising protection.
Technology Enablement for Security Operations
Healthcare IT teams rely on technology enablement to detect threats early and respond to incidents without disrupting care delivery.
- Real-time visibility into EHR access logs.
- API traffic monitoring for third-party integrations.
- Automated alerts for emerging threats.
- Technical assistance tools for rapid incident response.
When compliance and security are built into EHR workflow optimization, protection stops feeling like friction. It becomes part of everyday clinical operations. That balance is what mature healthcare enterprises aim for.
Scalability via Microservices and Cloud-Native EHR Architecture
As healthcare networks expand, traditional EHR architectures face performance limits. Cloud-native and microservices-based designs solve this by allowing EHR functions to scale independently without disrupting clinical operations.
Monolithic vs Cloud-Native EHR Architecture
| Capability | Traditional Monolithic EHR | Cloud-Native Microservices EHR |
|---|---|---|
| System scalability | Scales as a single large system | Services scale independently based on demand |
| Feature deployment | Large upgrades with downtime risk | Continuous updates with minimal disruption |
| Integration | Tightly coupled interfaces | API-first, loosely coupled services |
| Performance under peak load | Degradation during high usage | Elastic scaling during peak hours |
| AI integration | Limited flexibility for new tools | Easy integration of AI and third-party apps |
| Disaster recovery | Manual recovery procedures | Automated failover and geo-redundancy |
| Infrastructure cost | Fixed capacity overhead | Pay-for-use cloud consumption |
Key takeaway: Cloud-native EHR architectures transform scalability from a technical constraint into a growth enabler.
What Does an Enterprise EHR Optimization Plan Look Like in Practice?
Most large healthcare organizations do not struggle with optimization due to a lack of technology. EHR adoption is already widespread.
In the United States, 86% of office-based physicians and 94% of hospital-based physicians now use an electronic health record, driven in part by the Health Information Technology for Economic and Clinical Health Act. Implementation is no longer the challenge. Making these systems work efficiently is.
An effective optimization plan brings all these threads into a single execution path. Not as a one-time project, but as a staged transformation program.
Below is a roadmap that enterprise healthcare networks are adopting to drive sustained EHR efficiency.
Step 1: Baseline Assessment and Workflow Mapping
Every optimization program starts with visibility. You cannot fix friction you cannot see. Teams focus on understanding how work actually happens inside the system.
- Measure documentation time per role.
- Map high-frequency clinical workflows.
- Identify navigation and click bottlenecks.
- Review downtime incidents and system latency.
- Gather clinician feedback from live environments.
A common early discovery is variation. Two departments performing the same procedure often follow completely different EHR paths. Once workflows are mapped, standardization opportunities become obvious.
Step 2: Data Architecture and Interoperability Strategy
Optimization stalls when data remains fragmented across systems. This phase establishes the technical foundation for reliable data flow.
- Define enterprise data models.
- Standardize terminologies and code sets.
- Establish FHIR API strategies that leverage healthcare APIs for business growth and operational efficiency.
- Connect HIEs and external data sources using cloud-based solutions like the Google Cloud Healthcare API for scalable data management.
- Build master patient identity governance.
This is where EHR data optimization moves from concept to technical architecture.
Step 3: Workflow and Interface Optimization
Now visible change begins for frontline teams. The focus here is removing friction from daily clinical work.
- Design role-based screens.
- Create specialty-specific templates.
- Simplify order and result flows.
- Reduce alert fatigue.
- Configure context-aware clinical prompts.
Quick wins at this stage build early clinician trust in the optimization program.
Step 4: Documentation and Automation Acceleration
Once workflows stabilize, documentation load can be addressed. This step targets the biggest driver of clinician fatigue.
- Voice-enabled note capture.
- Ambient documentation integration.
- Auto-fill from prior encounters.
- Coding assistance at point of care.
- Smart defaults for recurring actions.
This directly improves EHR efficiency and reduces after-hours charting.
Step 5: Analytics and Clinical Intelligence Integration
An optimized EHR must support operational and clinical decision-making. This phase turns EHR into a data engine.
- Real-time dashboards for care teams.
- Automated quality measure reporting.
- Population health data pipelines.
- Research and registry data extraction.
At this point, data starts driving strategy instead of manual reporting.
Step 6: AI Readiness Enablement
Many enterprises add AI too early. Successful programs prepare first. This step ensures AI tools can integrate safely into clinical workflows.
- Standardized data labeling.
- Controlled model integration points.
- Monitoring of AI-driven recommendations.
- Governance for model updates and validation.
AI in EHR optimization becomes sustainable when these foundations exist.
Step 7: Governance, Training, and Change Management
Technology changes fail without adoption. This phase builds organizational alignment.
- Clinical super-user networks.
- Continuous training programs.
- Release management cycles.
- Feedback loops with frontline staff.
Some hospitals now run weekly optimization huddles where clinicians log friction points into a shared backlog. It keeps improvement continuous.
Step 8: Continuous Performance Monitoring
Optimization never ends. Enterprises track performance to sustain progress.
- Documentation time trends.
- Order turnaround time.
- Interface response latency.
- Integration uptime.
- Clinician satisfaction scores.
This keeps the optimization plan active long after rollout.
Steps of EHR optimization work best when executed as an enterprise transformation roadmap, not a series of disconnected configuration projects. Organizations that commit to structured execution see lasting improvements in care delivery, operational stability, and technology readiness.
Most enterprises uncover major friction during EHR assessments
How Do Governance and Management Drive Enterprise EHR Optimization?
EHR optimization often slows for one reason. Too many teams own pieces of the system, and no one owns the whole outcome. Clinical leaders focus on workflows. IT manages system performance. Compliance enforces HIPAA policies. Without shared governance, progress becomes fragmented.
Strong governance turns an optimization plan into a continuous improvement engine.
What Enterprise Governance Structures Include
Effective governance creates shared ownership across clinical, technical, and compliance teams, ensuring optimization decisions stay aligned with organizational priorities.
- Cross-functional optimization councils.
- Defined ownership for configuration and release cycles.
- Quarterly audits for security controls and workflow standards.
- Annual compliance reviews tied to HIPAA policies.
- System performance dashboards for executive oversight.
- User feedback loops to identify bottlenecks early.
Small operational habits make a difference. Some health systems run monthly workflow review sessions where clinicians log friction points directly into optimization backlogs. Issues get prioritized instead of lost.
Management Practices That Sustain Momentum
Strong management practices keep optimization programs moving forward even as technology, regulations, and clinical needs evolve.
- Long-term optimization strategies aligned to growth plans.
- Change management programs for new releases.
- Readiness planning for regulatory shifts.
- Risk assessments for emerging threats.
In enterprise healthcare, governance is what keeps EHR optimization aligned with strategy, compliance, and clinical reality. Without it, improvements remain isolated. With it, optimization becomes part of how the organization operates.
Which EHR Optimization Strategies Deliver Measurable ROI?
At some point, every healthcare executive asks the same question. Where will optimization actually move the needle? Not just improve usability, but deliver measurable returns.
The answer lies in focusing on strategies that touch revenue, cost, and care outcomes at scale. Below are EHR optimization strategies enterprises are investing in to generate tangible ROI.
Specialty-Specific Configuration
One-size-fits-all templates slow clinicians.
High-performing networks:
- Build service line-specific documentation flows.
- Create specialty-based order sets.
- Align clinical pathways with EHR logic.
- Standardize best-practice configurations across facilities.
This reduces variation in care delivery and improves documentation consistency for quality reporting.
Clinical Decision Support Tuning
Many EHRs suffer from alert overload.
Effective strategies include:
- Removing low-value alerts.
- Introducing context-aware recommendations.
- Linking prompts to evidence-based protocols.
- Tracking override rates to refine logic.
The result is better clinical guidance without interrupting care delivery.
Ambient and Voice-Based Documentation
Documentation time remains a top driver of burnout.
Enterprises now deploy:
- Ambient listening tools for visit summaries.
- Voice dictation for structured notes.
- Auto-suggested problem lists and orders.
A small operational detail. Some outpatient networks report same-day note completion rates rising sharply after ambient documentation rollout. That translates into faster billing cycles.
Revenue Cycle and Coding Optimization
Optimization often unlocks financial gains that were previously hidden.
Common initiatives:
- Real-time coding suggestions.
- Automated charge capture.
- Documentation completeness scoring.
- Integration with billing and claims systems.
These strategies reduce revenue leakage and accelerate reimbursement.
Interoperability Expansion
Data exchange improves both care coordination and financial performance.
Organizations focus on:
- Automated external record retrieval.
- Direct payer data integration.
- Referral workflow automation.
- Cross-facility care continuity.
This supports smoother transitions of care and fewer duplicated procedures.
AI-Powered Triage and Risk Scoring
Advanced enterprises move beyond passive records.
They deploy:
- Predictive models for readmission risk.
- AI-driven care gap identification.
- Automated patient outreach triggers.
- Intelligent scheduling recommendations.
This is where AI in EHR optimization shifts from pilot to operational impact.
EHR optimization strategies that deliver ROI share one trait. They are designed around clinical and financial outcomes, not software features. Enterprises that anchor optimization to measurable performance indicators see sustained leadership buy-in and faster transformation.
What Real World EHR Optimization Use Cases Show Enterprise Impact?
Enterprise leaders often ask where optimization delivers real operational change. Not in theory. In hospitals, clinicians feel the difference daily. The following examples show how targeted efforts translate into measurable EHR optimization for healthcare efficiency and better patient care.
Cleveland Clinic, USA: Streamlined nursing documentation
Cleveland Clinic launched an EHR Excellence initiative to reduce nursing documentation burden inside its Epic environment. The focus was simple. Remove unnecessary work from daily clinical routines.
Optimization actions
- Care plan documentation reduced 60 percent.
- Flowsheets expanded to allow concise charting for twice as many patients.
- Wound images added directly into patient records for real-time tracking.
- Redundant medication alerts reduced by 30 percent, nearly 3,000 fewer alerts per day.
Outcome
Nurses spent less time clicking screens and more time with patients. Post-initiative surveys showed higher nurse satisfaction and improved direct care time.
Royal Children’s Hospital Melbourne: Mobile EHR at the bedside
Royal Children’s Hospital equipped nurses with tablets running mobile EHR workflows. Documentation moved from stationary workstations to the patient bedside.
Optimization actions
- Bedside charting through mobile EHR access.
- Real-time record updates during care delivery.
Outcome
Nurses reported higher EHR satisfaction and faster, accurate documentation. Patient safety metrics improved as records stayed current during care interactions.
Hamad Medical Corporation, Qatar: Training-led optimization
Hamad Medical Corporation invested in comprehensive EHR onboarding for nurses to improve workflow adoption from day one.
Optimization actions
- Structured EHR proficiency training during onboarding.
- Ongoing workflow reinforcement sessions.
Outcome
Nurses reported above-average EHR satisfaction. Well-trained teams spent less time navigating the system and more time focused on patient care.
These examples show a consistent truth. Successful EHR optimization is not just technology. It is about removing friction from clinical work so care teams can focus on patients, not screens.
Global leaders already cut documentation burden by 60%
How Does EMR Cost Optimization Deliver Financial Impact?
Most healthcare enterprises do not struggle to justify EHR spend. They struggle to explain why costs keep rising while efficiency gains feel small. Licensing grows. Integrations multiply. Support contracts expand. Meanwhile, clinicians still chart late at night.
Understanding the distinction between EHR vs EMR systems helps organizations target optimization efforts more precisely. EMR cost optimization changes this equation. Not by cutting technology investment, but by making the EHR operate with fewer hidden drains on time, staffing, and revenue capture. When optimization is approached as a financial strategy, not just a technical initiative, cost control becomes sustainable.
Below is how cost ranges typically appear across large-scale EHR optimization programs in the US market.
Typical Enterprise EHR Optimization Cost Ranges
| Optimization Area | Typical Enterprise Cost Range | Primary Financial Outcome |
|---|---|---|
| Workflow and template redesign | $250K to $1M | Reduced clinician documentation time |
| Interoperability and API modernization | $500K to $2M | Lower integration maintenance cost |
| Documentation automation tools | $300K to $1.5M | Reduced overtime and faster billing |
| Analytics and data pipeline modernization | $400K to $2M | Improved quality reporting and population health ROI |
| AI readiness and clinical intelligence enablement | $500K to $3M | Foundation for predictive and decision support tools |
| Governance and training programs | $150K to $600K | Higher adoption and reduced rework |
Actual investment varies by network size, EHR platform, and existing technical debt. Still, most enterprises recoup returns through operational savings and revenue recovery within 12 to 24 months when execution is structured.
Key Cost Drivers in EMR Cost Optimization
Several factors shape where budgets are spent and where savings are unlocked.
- Legacy customization cleanup that reduces long-term maintenance load.
- Interface consolidation that lowers third-party integration fees.
- Documentation acceleration that cuts clinician overtime expenses.
- Coding and charge capture improvements that reduce revenue leakage.
- Automated reporting that lowers manual quality and compliance labor.
- Standardized configurations that reduce cross-facility training costs.
In simple terms, cost effectiveness of this optimization is not measured only by technology spend. It is measured by reclaimed clinician hours, recovered revenue, reduced compliance risk, and a lower cost of operating the digital backbone of care.
How Does NextGen EHR Optimization Enable AI-Driven Healthcare Evolution?
Years ago, most healthcare companies spoke of AI as long-term ambition. Today, many are testing clinical copilots, automated visit summaries, and predictive risk models. Still, in most environments, these tools sit beside the EHR instead of inside it.
That is where nextgen EHR optimization becomes essential. Understanding the broader impact of emerging technology on EHR systems helps organizations prepare for intelligent, integrated care delivery.
AI cannot deliver real clinical value if it operates outside core workflows. Enterprises that are serious about AI in care delivery are reshaping their EHR environments to support intelligent, governed, and real-time experiences.
Where Nextgen EHR Optimization Is Heading?
Healthcare organizations are focusing on practical AI-driven capabilities:
- Clinical copilots that assist with documentation and order selection.
- Predictive risk scoring is integrated into rounding and discharge planning.
- Ambient clinical intelligence that drafts visit summaries in real time.
- Intelligent scheduling aligned to patient urgency and provider availability.
- Automated care gap detection that triggers outreach workflows.
These capabilities depend on continuous EHR data optimization and alignment with current healthcare app trends driving patient engagement and clinical innovation. Without structured, accessible data, AI remains a side dashboard rather than a frontline tool.
What Enterprises Must Build To Support AI
AI in EHR optimization requires strong foundations:
- Standardized clinical terminologies and data models.
- Real-time data pipelines for continuous information flow.
- Secure API gateways for model integration.
- Governance processes for validating model outputs.
- Audit trails for AI-assisted clinical decisions.
Some hospital networks now run AI validation committees alongside clinical governance teams to review model accuracy and bias before deployment. That practice is becoming standard.
Nextgen EHR optimization is not about futuristic features. It is about turning the EHR into an intelligent operating layer that supports clinicians and scales with evolving care models.
In-House vs Outsourced Models for EHR Optimization Support
Most healthcare enterprises begin EHR optimization with in-house IT teams. Over time, integrations multiply, infrastructure ages, and uptime expectations rise. Internal capacity eventually becomes the constraint.
This is where sourcing strategy shapes long-term success. Organizations typically choose between building internally, buying managed services, or partnering with specialized healthcare IT providers.
EHR optimization support models
| Model | What It Means | Where It Works Best | Common Limitations |
|---|---|---|---|
| Build in-house | Internal IT teams handle EMR optimization, integrations, and support | Organizations with mature healthcare IT departments and stable environments | Limited scalability, higher downtime risk during peak demand |
| Buy managed services | Healthcare managed IT services oversee hosting, monitoring, and maintenance | Enterprises seeking predictable operations and reduced downtime | Less control over deep clinical workflow customization |
| Partner for optimization | Specialized healthcare IT consulting services lead EMR optimization programs | Enterprises pursuing large-scale transformation and modernization | Requires strong internal governance alignment |
Key decision factors
- Need for specialized knowledge in interoperability and security.
- Downtime tolerance and uptime requirements.
- Scalability during mergers and facility expansion.
- Cost savings from shared service models.
- Internal team bandwidth for long-term optimization.
Many enterprises adopt hybrid models. In-house teams retain clinical ownership. Outsourced healthcare IT partners manage infrastructure, integrations, and continuous tuning. This balance keeps systems stable while freeing internal teams to focus on care delivery.
What Challenges Do Enterprises Face While Optimizing EHRs?
Most healthcare leaders enter optimization with strong intent and clear goals. Still, progress often slows once real-world constraints appear. These challenges are not about lacking technology. They come from legacy complexity, competing priorities, and change fatigue inside large organizations.
Below are the most common barriers enterprises encounter, along with practical ways to move past them.
Legacy Data Fragmentation
Many health systems operate multiple EHR instances, inherited platforms, or disconnected departmental systems. Clinical data sits in different formats, code sets, and storage layers, which makes EHR data optimization slow and error-prone.
How enterprises address it
- Establish enterprise-wide data models.
- Standardize terminologies and patient identity management.
- Build FHIR-based integration layers.
Clinician Resistance to Change
Even well-designed improvements can face pushback when staff are already under pressure. New workflows may feel disruptive before benefits become visible.
How enterprises address it
- Involve frontline clinicians in design sessions.
- Launch small pilot rollouts before network-wide deployment.
- Create super-user support teams inside departments.
Over-Customization Debt
Years of ad-hoc EHR changes often create fragile configurations that are difficult to upgrade or scale. Optimization efforts then risk breaking existing workflows.
How enterprises address it
- Audit current customizations.
- Retire low-value legacy configurations.
- Shift toward standardized, template-driven design.
Integration Sprawl
Multiple point-to-point interfaces and third-party tools increase maintenance costs and failure points. Interoperability becomes reactive instead of strategic.
How enterprises address it
- Consolidate integrations through API gateways.
- Adopt FHIR-first integration strategies.
- Centralize interface governance.
Governance and Ownership Gaps
Optimization programs stall when responsibility is split across IT, clinical leadership, and compliance teams without clear accountability.
How enterprises address it
- Establish cross-functional optimization councils.
- Define release and change management processes.
- Tie optimization KPIs to executive oversight.
In practice, challenges in EHR optimization strategy are manageable when approached with structure and shared ownership. Enterprises that treat optimization as continuous transformation, not periodic repair, sustain momentum and measurable progress.
Unresolved EHR challenges compound cost and compliance risk
What Are the Benefits of EHR Optimization for Healthcare Enterprises?
Most healthcare organizations do not invest in optimization just to improve software usability. They do it to change how care is delivered, how teams work, and how efficiently the business runs. When optimization is executed with the right strategy, benefits appear across clinical, operational, and financial layers.
Below are the outcomes enterprises see when EHR optimization becomes part of long-term transformation.
Stronger EHR Efficiency Across Clinical Teams
Optimized workflows remove friction from daily routines. Clinicians spend less time navigating screens and more time with patients.
Enterprise impact
- Shorter documentation cycles.
- Reduced after-hours charting.
- Faster order turnaround.
- Higher staff retention in high-burnout departments.
Improved Patient Experience and Continuity of Care
Patients notice when systems work smoothly behind the scenes. Records follow them. Appointments run on time. Communication becomes consistent.
Enterprise impact
- Unified patient records across facilities.
- Faster referrals and care transitions.
- Higher patient satisfaction and loyalty.
- Lower administrative call volumes.
Better Data Governance and Decision Intelligence
Clean and accessible data changes how leaders make decisions. Reporting becomes real-time. Insights replace assumptions.
Enterprise impact
- Automated quality measure reporting.
- Reliable population health analytics.
- Stronger regulatory compliance.
- Faster executive decision cycles.
Financial and Revenue Performance Gains
EHR optimization often reveals hidden financial leaks and process waste that were accepted as normal.
Enterprise impact
- Improved coding accuracy.
- Reduced revenue leakage.
- Lower integration maintenance costs.
- Faster reimbursement cycles.
AI-Ready Healthcare Operations
Enterprises preparing for AI-driven care need structured data and stable workflows. Optimization builds that foundation.
Enterprise impact
- Faster deployment of clinical AI tools.
- Safer integration of decision support.
- Scalable innovation pipelines.
Simply put, optimization benefits compound over time. The more aligned the EHR becomes with clinical and business goals, the more resilient, intelligent, and efficient the healthcare enterprise becomes.
Why Choose Appinventiv for Enterprise EHR Optimization?
Most healthcare enterprises do not need another technology vendor. They need a partner who understands clinical reality, data complexity, and the pressure to comply. That is where Appinventiv fits.
We bring a decade of healthcare engineering experience into EHR integration services and optimization programs designed for scale.
Healthcare delivery at enterprise scale
- 500+ digital health platforms delivered.
- 450+ healthcare clients served.
- 10+ years in HealthTech projects.
- 300+ connected medical devices integrated.
- 99.90% uptime for critical systems.
Proven operational impact
- 45% hospital operational efficiency gains.
- 90%+ clinical data accuracy achieved.
- 95% patient satisfaction across deployed apps.
Our case work reflects this depth. From remote care platforms like YouComm and Soniphi to population health and chronic care solutions like Health-e-People and DiabetiCu, we build systems that manage real clinical workloads, not prototypes.
Appinventiv helps enterprises turn EHR optimization into a sustained capability, not a one-time project. Let’s connect and start your optimization roadmap.
Frequently Asked Questions
Q. What is EHR Optimization?
A. Most healthcare leaders already live with an EHR. Optimization is what happens after implementation, when the focus shifts to improving workflows, data flow, usability, interoperability, and analytics readiness. It turns the EHR from a digital filing system into a clinical and operational engine that supports care teams, business goals, and long-term technology strategy.
Q. How to improve electronic health records optimization?
A. Improvement starts with understanding real workflow friction. Enterprises map clinical processes, clean and standardize data, modernize integrations, simplify interfaces, and introduce automation where it reduces manual effort. Training and governance keep changes sustainable. The most successful programs treat optimization as a continuous roadmap, not a one-time configuration exercise.
Q. Why is EHR Optimization important in 2026?
A. Healthcare is moving toward connected data ecosystems, value-based care, and AI-assisted clinical decision-making. Unoptimized EHR cannot support these shifts. In 2026, optimization is essential for interoperability compliance, clinician efficiency, patient experience, analytics reliability, and AI readiness. It directly influences care quality, operating cost, and competitive position.
Q. What type of challenges are faced while optimizing EHRs?
A. Common challenges include fragmented legacy data, over-customized systems, integration sprawl, clinician resistance to change, and unclear governance ownership. These slow progress and increase risk. Enterprises overcome them through standardization, API-led integration, clinician involvement in design, phased rollouts, and cross-functional optimization councils.
Q. What is the cost-effectiveness of EHR optimization?
A. Cost effectiveness comes from reclaimed clinician time, reduced overtime, improved coding accuracy, lower integration maintenance, and avoided compliance penalties. While optimization requires investment, most enterprises see measurable operational savings and revenue recovery within one to two years. The long-term value lies in building an EHR that scales with growth and innovation.
Q. How do education and training support successful EHR optimization?
A. Even the best EHR optimization fails if users are not prepared to work differently. Enterprises invest in clinician-led training, hands-on training sessions, and updated training materials aligned to new workflows. Staff training programs also reinforce HIPAA awareness, healthcare compliance practices, and the secure use of systems. Ongoing training program updates, technical support access, and workflow training ensure teams adapt smoothly to system upgrades and remain audit-ready during compliance audits.
Q. How does system customization improve EHR optimization?
A. System customization enables healthcare enterprises to align the EHR with real clinical workflows rather than forcing teams to adapt to rigid interfaces. IT team testing, on-site sessions, and workflow redesign help tailor templates, alerts, and features to department-specific best practices. Identity management solutions and access and authentication controls ensure security during customization. Structured system updates prevent system instability while maintaining hardware and security compliance.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How to Build a Custom Pediatric EMR and EHR System?
Key takeaways: Clinical Precision: Custom systems accommodate pediatric-specific data points like percentile curves and weight-based longitudinal dosing. Interoperability: Seamless data exchange via HL7 FHIR ensures your practice stays connected to pharmacies, labs, and state registries. Regulatory Resilience: Built-in compliance with HIPAA, HITECH, and MACRA/MIPS reduces legal friction. Enhanced Engagement: Parent portals reduce administrative overhead by…

Change Management in Healthcare: Principles, Processes, and Models
Key Takeaways Change in healthcare fails quietly when ownership, workflow alignment, and follow-through are missing. Successful change management in healthcare focuses on adoption, not just system implementation. Clinical workflows and workforce capacity determine whether transformation sticks or stalls. Governance, clear accountability, and post-go-live support matter more than the model used. Sustainable healthcare transformation depends on…
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…