- Why Unified Systems Drive Competitive Advantage in Healthcare
- The Central Role of Telehealth-EHR Integration
- The Critical Question Every Business Leader Must Ask
- The Power of Unified Data Ecosystems
- Real-World Impact: Use Cases That Deliver a Difference.
- Market Positioning Through Advanced Integration Capabilities
- The Right Tools for the Job: Must-Have Features in a Modern System
- Implementation Strategy: Executive Roadmap for System Integration
- Discovery and Strategy
- Selecting the Right Integration Partner
- API and Middleware Development
- Testing and Quality Assurance
- Deployment and Training
- Strategic Implementation Framework for Healthcare Leaders: Best Practices
- Investment Analysis: Total Cost of Ownership vs. Strategic Value
- Executive Risk Management: Overcoming Integration Challenges
- Why Choose Appinventiv for Seamless Telehealth EHR Integration
- Frequently Asked Questions (FAQs)
- Competitive Differentiation: (38x Higher Patient Engagement Rates) Organizations with seamless telehealth EHR integration achieve dramatically higher patient retention and satisfaction compared to competitors with fragmented systems.
- Operational Excellence: (Unified Data Architecture Eliminates Silos) Integrated systems enable proactive care models, predictive analytics, and comprehensive clinical decision-making for superior patient outcomes.
- Strategic Risk Mitigation: (Future-Ready Infrastructure Investment) Today’s integration investments position organizations for value-based care, AI-powered delivery, and patient-centric service expectations.
- Financial Impact: (30% Cost Reduction + $86,400 ROI Per Provider) Measurable returns through $86,400 savings per provider and 30% operational cost reductions across healthcare organizations.
In the dynamic landscape of modern healthcare, conversations have moved far beyond initial digital tool adoption. Strategic focus now centers on creating seamless, interconnected systems that improve care delivery while enhancing operational efficiency and financial health. But what drives this technological convergence?
Healthcare technology’s true power emerges not through separate tools, but by uniting them into cohesive ecosystems. For those shaping their healthcare organizations’ future, synergy between robust telehealth platforms and Electronic Health Record (EHR) systems transcends mere options—it becomes a foundational pillar for sustainable growth and superior patient outcomes.
This represents a deep dive into strategic considerations that matter most. Moving from disparate digital tools to fully integrated, streamlined ecosystems requires careful exploration. How do organizations bridge this transformation gap?
The insights that follow provide comprehensive, actionable roadmaps for organizations ready to leverage to their fullest potential. This discussion centers on real-world implications of strategic decisions, from tangible benefits of connected systems to practical implementation steps, without basic definitional digressions.
Bonus Read: Guide On EHR Software Development
Learn how integrating telehealth with EHR systems boosts care efficiency and satisfaction. Partner with Appinventiv to implement a solution that works for you.
Why Unified Systems Drive Competitive Advantage in Healthcare
Healthcare organizations today operate in an ecosystem where data remains the most valuable asset, yet this critical information often creates more problems than solutions. Fragmented approaches emerge when telehealth platforms exist separately from core EHR systems, leading to disjointed patient experiences and multiplying administrative burdens. Organizations lose their single source of truth for clinical data, making telehealth EHR integration a strategic imperative rather than a luxury feature.
Must Read: Rise of Telehealth Adoption Amidst Coronavirus
The Central Role of Telehealth-EHR Integration
The role of Electronic Health Records (EHR) in telehealth integration is to function as the central nervous system for modern healthcare delivery. When telehealth platforms integrate with EHRs successfully, something remarkable happens:
- Automatic data capture – Every virtual consultation, lab result, and patient message flows directly into patient files
- Eliminated manual processes – Time-consuming data entry disappears entirely
- Reduced human error – Manual transcription mistakes become obsolete
- Comprehensive visibility – Providers access complete patient histories regardless of visit type
This seamless connectivity drives superior clinical decision-making through single-point information access.
Bonus Read: Ways Electronic Health Records Will Continue to Improve in 2025
The Critical Question Every Business Leader Must Ask
Does your current technology architecture enable seamless information flow, or are you inadvertently creating operational silos with every new digital tool adoption?
The pressure to deliver exceptional patient care has never been higher, and disconnected tech stacks simply can’t support this mission. Consider these realities:
- Modern patients expect cohesive, integrated experiences
- Clinicians demand efficient, consolidated workflows
- Integration failures create cascading problems: clinician burnout, skyrocketing costs, eroded competitive positioning
The Power of Unified Data Ecosystems
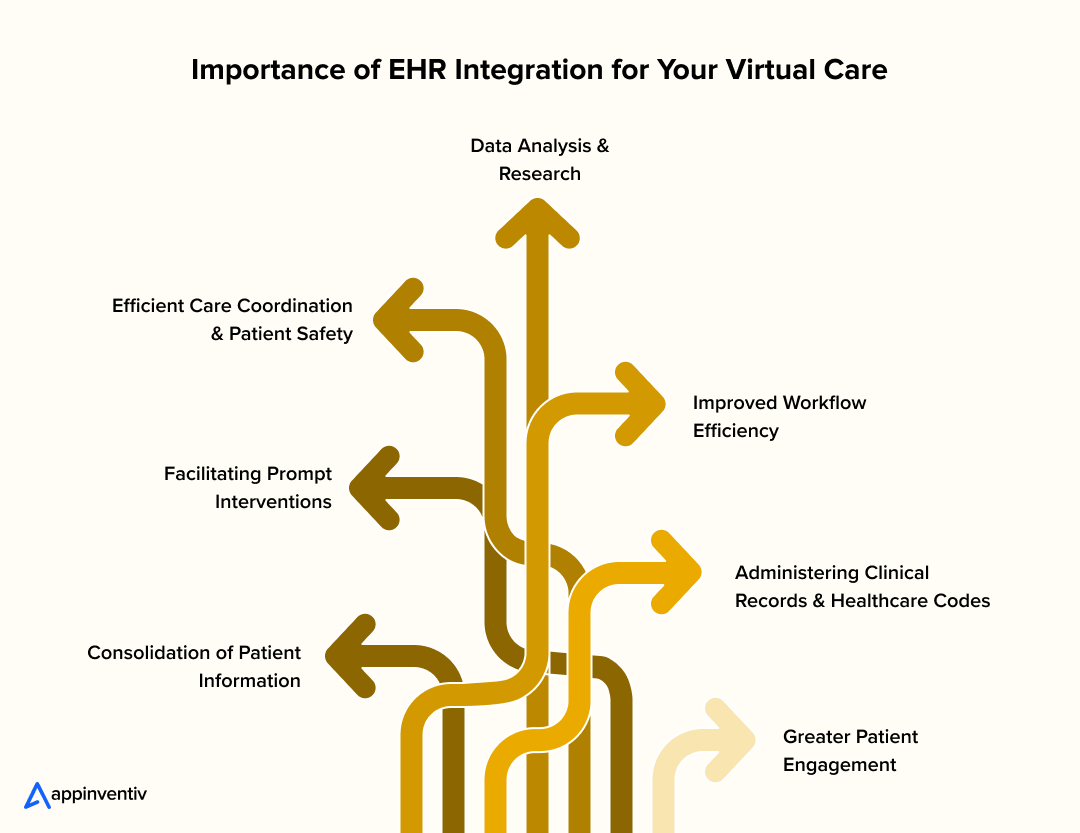
When rich, longitudinal EHR data combines with telehealth’s real-time capabilities, organizations unlock transformative potential. This foundation enables:
Strategic Capabilities:
- Proactive care model development
- Advanced predictive analytics deployment
- Personalized patient journey creation
- Intelligent healthcare delivery optimization
Operational Benefits:
- Reactive-to-proactive care transformation
- Comprehensive patient context integration
- Enhanced clinical decision-making frameworks
- Future-ready healthcare delivery systems
Thoughtful telehealth EHR integration serves as the critical bridge connecting patient history with virtual care, enabling healthcare organizations to deliver more intelligent, insightful patient experiences while positioning themselves for sustainable competitive advantage.
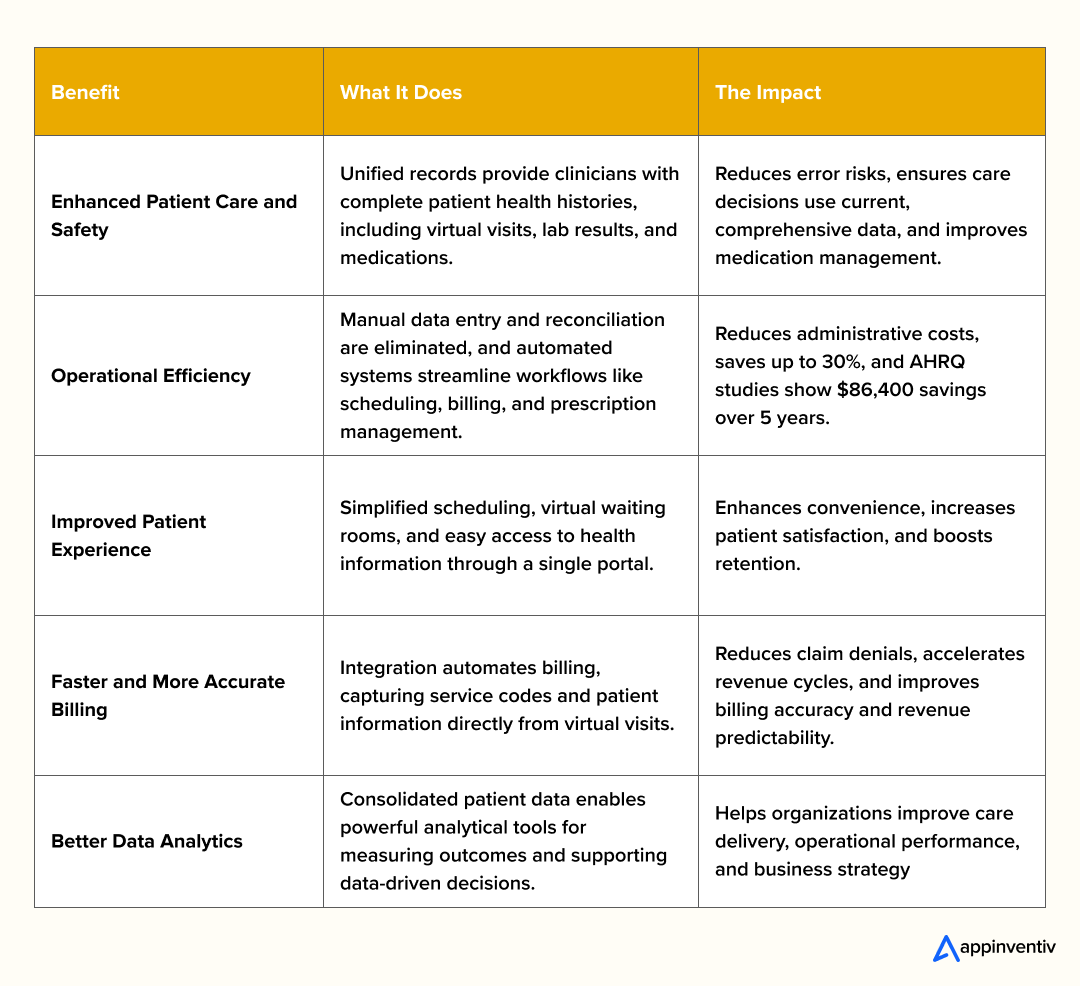
Here are some summarized benefits of integrating telemedicine with EHR:
Real-World Impact: Use Cases That Deliver a Difference.
EHR and telehealth integration creates transformative value across clinical settings. Seamless systems empower providers with real-time data, enhancing care delivery. Use cases of integrating EHR in telehealth span diverse scenarios, as shown in these real-world examples:
Post-Surgical Follow-Ups: Cleveland Clinic leverages telehealth-EHR integration for virtual check-ins. Surgeons review recovery progress via video, with notes auto-syncing to patient charts, ensuring continuity and reduction in office visits. This strengthens patient-provider trust through convenient, high-quality follow-up care. It also optimizes resource allocation by prioritizing in-person visits for complex cases.
Remote Patient Monitoring: Kaiser Permanente’s MyChart, integrated with Cerner EHR, uses patient monitoring platforms to track diabetes patients’ vitals via connected devices. Abnormal readings trigger instant alerts, enabling proactive interventions and cutting readmissions. This fosters a proactive care culture, empowering clinicians to anticipate needs. It enhances patient autonomy by supporting self-management at home.
Tele-specialty Consultations: Teladoc Health’s platform, integrated with Epic EHR, enables specialists to access full patient histories during virtual consults. Notes sync seamlessly through MyChart integration, eliminating manual transcription and reducing errors. This streamlines specialist workflows, improving care coordination across teams. It also elevates patient confidence in virtual specialty care delivery.
Chronic Disease Management: Mayo Clinic’s COVID-19 Remote Patient Monitoring Program, with all patient data integrated into Epic EHR systems, achieves high engagement, reducing hospital admissions and supporting rural care. Responses trigger alerts based on predetermined parameters, enabling proactive interventions through centralized nursing teams. This builds scalable models for managing chronic conditions remotely. It strengthens community health by bridging access gaps for underserved populations.
Rural Telehealth Access: Rural healthcare facilities leveraging federal HITECH Act funding for EHR implementation successfully overcome financial barriers and achieve improved patient care through integrated digital health solutions. This expands market reach by serving remote communities effectively. It positions organizations as leaders in equitable healthcare delivery.
Future trends signal deeper connectivity. Value-based care demands unified data for analytics, impossible without integration. AI in EHR, like Epic’s predictive tools, delivers personalized care recommendations by identifying at-risk patients early. Tech-savvy patients expect data control, driving integrated systems to empower users.
Must Read: 11 Ways AI is Transforming the Telemedicine Sector
Market Positioning Through Advanced Integration Capabilities
Understanding EHR with telehealth architecture matters when making system decisions. Components of telehealth EHR integration typically include these essential pieces:
- Telehealth Platform: Front-end application where patients and providers conduct virtual consultations.
- EHR System: Central database storing patient health data—medical histories, lab results, billing details, everything.
- Integration Middleware: “Connector” software enabling secure data exchange between systems. Handles data mapping and synchronization tasks.
- APIs (Application Programming Interfaces): Software protocols allowing different applications to communicate effectively.
Types of telehealth EHR Integration offer strategic decision-makers several pathways:
- Partial Integration: Limited data sync sharing only essential information like patient demographics between systems. Perfect starting point for organizations with basic requirements.
- Comprehensive Integration: Full-scale integration synchronizing nearly all relevant patient data in real-time. Delivers maximum workflow efficiency and data integrity benefits.
- Embedded Integration: Telehealth functionality lives directly inside the EHR system itself. Providers never leave their EHR dashboard—an ultimate seamless experience.
Every EHR integration for telehealth brings trade-offs. Your choice hinges on organizational needs, available budget, and strategic objectives.
The Right Tools for the Job: Must-Have Features in a Modern System
Well-architected telehealth EHR integration succeeds through core functionality that serves clinicians and patients effectively. When evaluating platforms or integration projects, focus on essential features for telehealth EHR integration that drive real results. Modern EHR telemedicine solutions must address current needs while anticipating future requirements, maintaining strategic value over time.
These features include:
- Scheduling Automation: Integrated systems let providers manage in-person and virtual appointments from single calendars, automatically updating EHRs.
- Real-Time Data Synchronization: Instant patient data updates across both systems prevent errors while ensuring providers have access to current information.
- Secure Messaging: Integrated secure messaging enables provider-patient and provider-clinician communication directly from platforms, with all communications logged in patient records.
- E-Prescribing: Providers send prescriptions securely to pharmacies directly from telehealth platforms, with prescription records automatically added to patient files.
- Billing and Coding Integration: Automated billing captures all virtual visit services accurately and sends data to billing departments, reducing revenue losses.
Digital tools define modern healthcare landscapes. Organizational success depends on how well these tools collaborate. Investing in a robust EHR for telehealth solutions represents foundational decisions, preparing organizations for today’s challenges and tomorrow’s opportunities. Strategic foresight separates market leaders from followers. Building resilient, efficient, patient-centric healthcare delivery systems requires well-planned integration as the most impactful step.

Moving forward with comprehensive telehealth EHR integration transcends technology decisions. It represents a commitment to delivering superior care standards through investments in efficiency, accuracy, and patient-provider well-being.
Implementation Strategy: Executive Roadmap for System Integration
Successfully navigating the technical and logistical complexities of EHR integration for telehealth demands thoughtful, systematic approaches. This strategic project transcends simple software installation requirements. Organizations seeking to maximize synergy benefits must implement carefully planned, precisely executed processes.
Related Read: White Label Telemedicine Platform Development
The process to build an EHR-integrated telehealth app typically includes the following steps:
Discovery and Strategy
Initial phases demand comprehensive infrastructure analysis. Which EHR platform does your organization currently utilize? How do clinical teams structure their specific workflow requirements? Strategic planning emerges through outlining integration objectives, selecting optimal integration methodologies, and establishing measurable performance indicators. Potential roadblocks require identification alongside corresponding risk mitigation frameworks.
Selecting the Right Integration Partner
Development team selection hinges on deep healthcare regulation expertise (HIPAA compliance) combined with modern API-based integration mastery. These partners must comprehend organizational uniqueness while demonstrating successful implementation histories. Exceptional partners function as strategic consultants beyond mere technical vendors, navigating project intricacies with seasoned guidance.
API and Middleware Development
Integration architecture relies fundamentally on APIs (Application Programming Interfaces). These digital communication bridges enable seamless telehealth platform and EHR system interactions. Middleware layers—specialized software positioned between disparate systems—manage data transformation processes while maintaining secure information transmission protocols. API reliability and security architecture determine integration success or failure.
Testing and Quality Assurance
Extensive testing protocols verify data integrity alongside security compliance standards. Testing encompasses data synchronization accuracy, user workflow optimization, and system performance under variable operational loads. Thorough QA methodologies guarantee integrated system functionality before organizational deployment phases.
Deployment and Training
Verified integrations undergo controlled environment deployment procedures. Staff training programs target both clinical and administrative personnel, facilitating seamless operational transitions and accelerated user adoption rates. Comprehensive training investment ensures personnel confidence and workflow proficiency within newly integrated operational frameworks.
Strategic Implementation Framework for Healthcare Leaders: Best Practices
Successful telehealth EHR integration doesn’t happen by accident—it demands strategic planning and proven methodologies. Best practices exist specifically to reduce risks, streamline processes, and maximize solution value. Here’s what many organizations miss: integration never truly ends. It’s an ongoing optimization, not a checkbox project. New telehealth features roll out regularly. EHR systems get updated constantly. Your integration must evolve alongside these changes to maintain seamless interoperability.
- Define Clear Goals: What does success actually mean for your project? Better patient satisfaction scores? Slashed administrative costs? Revenue growth? These targets drive every decision you’ll make. Focus on patient retention alone, and you’re looking at serious ROI boosts through increased lifetime patient value with EHR integration for telehealth.
- Prioritize Data Security: Security comes first. Build robust encryption, strict access controls, and bulletproof compliance protocols from day one. Patient data protection can’t be an afterthought.
- Choose a Flexible API: Your integration needs modern, adaptable APIs that won’t break when platforms update. Future-proofing isn’t optional—it’s survival. Rigid systems become expensive headaches later.
- Involve End-Users Early: Get clinicians, nurses, and admin staff involved during planning and testing. Their real-world insights on EHR telemedicine beat theoretical workflows every time. Co-creation drives adoption success.
- Plan for Continuous Monitoring: Deployment isn’t the finish line. Monitor performance, data integrity, and security vulnerabilities constantly. Proactive beats reactive when system stability matters.
Healthcare’s technology adoption history spans decades, but real transformation happens when systems actually talk to each other. The synergy of EHR and Telehealth proves this point perfectly. Done right, it multiplies impact rather than just adding features. Consider this: one extra consult per physician daily generates $80,000 additional revenue annually. That’s the power of streamlined workflows.
Smart EHR for telehealth integration isn’t just tech upgrades—it’s strategic positioning. Organizations deliver superior care, slash operational waste, and build financial resilience simultaneously.
Connect with our development team to explore how your organization can replicate these proven efficiency gains through strategic system integration
Investment Analysis: Total Cost of Ownership vs. Strategic Value
Strategic decision-making invariably centers on financial implications. The cost to integrate EHR software in telehealth varies dramatically across organizational contexts. Multiple variables influence pricing: existing EHR system complexity, selected integration methodologies, and project scope parameters. Initial investments may appear substantial, yet long-term ROI perspectives reveal different calculations. Well-executed telehealth electronic health record integrations optimize resource utilization while substantially reducing manual labor expenditures.
While costs vary widely, healthcare organizations need realistic investment expectations. Let us break down current industry figures:
- Small to Mid-Sized Practices:
- Initial Setup/Implementation: Software, hardware, and setup costs? Small-scale healthcare providers typically see $20,000 to $65,000. Mid-sized healthcare providers face a $65,000 to $200,000 range.
- Data Migration: Patient record transfers present significant variables. Expect $5,000 to $150,000+, depending on your data’s volume and structural complexity.
- Custom Development: Need something built from scratch? Basic projects begin around $50,000. Complex systems easily reach $500,000 or higher.
- Large Hospitals & Health Systems:
- Enterprise implementations aren’t cheap. We’re talking $400,000 to $600,000+ territory, scaling with facility count and user populations.
But wait—there’s more. Ongoing costs hit your budget yearly:
- Annual Maintenance & Support: Mid-sized institutions budget $10,000 to $50,000 annually. Large hospitals? Think hundreds of thousands.
- Licensing Fees: Per-user charges add up fast: $100 to $500 monthly per provider for most commercial solutions.
- Staff Training: Initial training runs $1,000 to $5,000 per person. Annual refreshers cost $500 to $1,200 per user.
Here’s the thing about vendor selection—price tags lie. Real value emerges from partnerships that evolve with your growth trajectory. That “bargain” upfront price? It often masks expensive limitations or surprise fees later.
Related Read: Cost and Features of Developing a Telemedicine App Like Altibbi
Executive Risk Management: Overcoming Integration Challenges
While benefits appear obvious, the challenges of integrating EHR in telehealth create genuine obstacles demanding proactive solutions. Technical, operational, and regulatory barriers merge into complex problems. Success depends on combining technical knowledge with strategic planning. Take data synchronization—massive patient record volumes create serious technical headaches. Smart partners develop clear protocols for secure, efficient data management.
The most common challenges include:
- Legacy Systems: Many healthcare organizations rely on older EHR systems with limited or outdated APIs. These integrations become complicated, often demanding custom development work. Partners experienced in legacy system modernization prove invaluable here.
- Data Security and Privacy: HIPAA compliance isn’t optional. EHR telemedicine Integrations require bulletproof security protocols protecting sensitive patient information during inter-system transfers. A comprehensive EHR with telehealth solutions must prioritize security above everything else.
- Technical Complexity: Telehealth and EHR architectures get messy fast. Data synchronization, duplicate prevention, and real-time information exchange need specialized expertise. One mistake creates cascading problems.
- User Adoption: Poor training equals clinician resistance. New integrated workflows fail without smooth user experiences. Change management strategies determine rollout success or failure.
What’s blocking unified approaches in your organization? Technical complexity fears? Security concerns? Stakeholder buy-in challenges?
Why Choose Appinventiv for Seamless Telehealth EHR Integration
As a leading telehealth app development company, Appinventiv brings unparalleled expertise in creating seamless integrations between telehealth platforms and Electronic Health Records (EHR) systems. With over a decade of experience, our team of 1,600+ tech experts has successfully delivered 3,000+ solutions for renowned healthcare clients, including Soniphi, DiabeticU, Health-e-People, YouComm, and global brands like KFC, IKEA, and Adidas.
Appinventiv holds ISO 13485, 27001, and 9001 certifications, ensuring quality, security, and operational excellence in healthcare development. Our industry recognition showcases our commitment to innovation and client success. Our HIPAA-compliant solutions with HL7/FHIR standards implementation and end-to-end encryption ensure seamless telehealth EHR integration while maintaining the highest security and regulatory compliance standards for modern healthcare delivery.
Our prestigious awards include:
- Consecutive Deloitte Technology Fast 50 Awards (2023 & 2024) with #1 ranking in Digital & Cloud Tech category
- “Tech Company of the Year” at Times Business Awards 2023
- Clutch Global Champ Award 2025 for Chatbots & Android
Ready to transform your healthcare delivery with seamless telehealth EHR integration? Partner with Appinventiv today and leverage our award-winning expertise to build secure, scalable, and interoperable healthcare solutions that drive better patient outcomes and operational efficiency.
Frequently Asked Questions (FAQs)
Q. Why Should You Invest in EHR-Integrated Telehealth Apps?
A. Healthcare shifts toward digital solutions rapidly, making Telehealth EHR Integration based apps smart investment opportunities. These platforms streamline patient data management while expanding care access, creating significant cost savings for providers through integration that eliminates duplicate data entry. Medical errors have reduced substantially as workflows become more efficient throughout the process.
The growing demand for remote healthcare services continues accelerating alongside regulatory support that strengthens market positioning. Strong revenue potential becomes evident while patient satisfaction improves through convenient medical record access and seamless care coordination that enhances user experience. These combined factors make them valuable long-term investments.
Q. How Do You Ensure Data Security in a Telehealth-EHR Integrated App?
A. Data security in telehealth-EHR apps demands multiple protective layers that function cohesively to safeguard sensitive information. End-to-end encryption becomes essential for patient communications while robust authentication systems need implementation alongside multi-factor verification that adds crucial security depth. Regular security audits identify vulnerabilities before problems emerge, ensuring comprehensive protection.
HIPAA compliance isn’t negotiable, it’s fundamental for maintaining patient trust since heavy penalties await non-compliant organizations. Role-based access controls restrict sensitive information viewing to authorized personnel only while secure cloud storage provides additional protection through automatic backups that prevent data loss scenarios. This comprehensive approach ensures healthcare providers maintain accessibility when patient information becomes critical.
Q. How Does EHR Integration Enhance the Telehealth Experience for Patients?
A. EHR integration transforms telehealth by providing patients seamless access to complete medical histories during virtual visits, allowing doctors to review past treatments instantly while medications and test results become immediately available. More informed decisions result from this comprehensive access as care quality improves substantially since patients avoid repeating medical histories repeatedly. Appointments become more efficient and less frustrating for everyone involved.
Prescription management flows more smoothly since providers check current medications quickly while potential interactions get identified faster through integrated systems. This integration enables superior follow-up care coordination where treatment plans update automatically across all platforms and visit notes sync seamlessly between systems. Continuity remains consistent whether patients see specialists or primary care physicians throughout their healthcare journey.
Q. How Is Telehealth Currently Integrated in Healthcare?
A. Telehealth has become deeply embedded in modern healthcare systems through various channels where hospitals offer virtual consultations for non-emergency cases, while primary care practices use video calls for routine check-ups and follow-up appointments that happen remotely. Mental health services embrace telehealth particularly enthusiastically, as therapy sessions occur remotely with great success since insurance providers cover telehealth visits frequently.
Financial accessibility improves significantly for patients while healthcare networks integrate these platforms directly into existing EHR systems, making seamless documentation possible as care coordination flows more smoothly. Rural areas benefit especially from telehealth’s capabilities since patients can connect with specialists who might be hundreds of miles away through these integrated systems.
Q. How to Make a Telemedicine EHR System HIPAA Compliant?
A. Creating HIPAA-compliant telemedicine EHR systems demands strict attention to patient data protection standards, where strong encryption for data transmission needs implementation first, while storage security requires equal priority. All communications must remain secure throughout the process before comprehensive access controls are established to limit patient information viewing based on user roles specifically.
Regular risk assessments help identify potential system vulnerabilities, while staff training on HIPAA regulations proves essential since human error causes breaches frequently without proper education. Security measures require thorough documentation alongside audit trails of data access that need constant maintenance. Business associate agreements with third-party vendors ensure compliance standards so that protected health information handling meets requirements across all partnerships.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…