- How is the Shift from Population-Based Protocols to Individualized Therapies Happening?
- How Does AI Power Personalized Diagnosis and Treatment?
- Which Disease Areas Are Seeing the Most Impact?
- AI in Oncology Treatment
- AI for Chronic Disease Management
- AI for Cardiovascular Disease
- Rare or Complex Diseases
- Autoimmune Disorders
- Mental and Behavioral Health
- Neurological Disorders
- Transforming Drug Discovery and Treatment Matching
- AI Accelerates Drug Development
- Repurposing What Already Works
- Matching Patients to Therapies, Not the Other Way Around
- AI for Individualized Treatment Matching
- How Generative AI Is Shaping Truly Personalized Treatment Plans
- Simulating Patient-Specific Outcomes
- Creating Synthetic Data for Rare Diseases
- Personalized Documentation and Education
- Accelerating Drug Discovery
- The Role of Digital Therapeutics in Personalized Care
- Companion Tools for Complex Conditions
- Optimizing for Adherence and Outcomes
- From Drug to Digital to Data
- What are the Ethical Considerations to Prepare for AI-Driven Personalized Care?
- Algorithmic Bias Isn’t Just a Technical Flaw It’s a Clinical Risk
- Consent and Transparency Must Be Built In
- Explainability Matters Especially at the Point of Care
- What is the Future of AI in Personalized Healthcare?
- Multi-Omics and Hyper-Personalization
- Edge AI and Wearable Health Streams
- AI Agents in Clinical Decision Support
- Decentralized Clinical Trials and Adaptive Research
- How AI is Shaping Personalized Care & How Appinventiv Can Help
- What to Adopt Now:
- What to Prepare For:
- FAQs
Key takeaways:
- AI enables precise, individualized treatment plans by analyzing patient data, genomic profiles, and clinical histories, moving away from generalized protocols.
- AI models help anticipate medical events and tailor care, improving outcomes through proactive, personalized interventions.
- AI integrates diverse data sources (EHRs, genetics, imaging) to provide faster, more accurate decision-making in clinical workflows.
- AI is enhancing treatments in oncology, chronic disease management, and rare genetic disorders by offering tailored, data-driven therapies.
Personalized care has always been the gold standard in medicine – hard to scale, harder to systematize. But artificial intelligence is changing that. Today, with AI in personalized treatment plans, we’re no longer guessing which therapy might work. We are analyzing real-time patient data, genomic profiles, and clinical histories to inform care with precision that was never possible before.
The surge in AI in personalized medicine is driven by a practical need: physicians and specialists are seeing more patients with overlapping conditions, unique genetic backgrounds, and unpredictable treatment responses. Relying on clinical averages just isn’t enough.
What’s emerging is a new, data-powered model – AI-driven precision medicine where algorithms help match patients to the therapies most likely to help them, not statistically, but individually. It’s a shift from reactive to predictive care, from broad-stroke treatments to deeply tailored protocols.
For US healthcare leaders and clinicians, this isn’t just exciting, it’s actionable. Because the infrastructure, data, and tools are already here. The question is: how do we integrate them in a way that actually improves outcomes?
This guide breaks it down, how AI is being used in real-world personalized care, where it’s making a difference across diseases, and what to consider when implementing it in your own care model.
You have the patient data. We have the AI engineering expertise to transform that data into predictive insights and deeply tailored treatment plans.
How is the Shift from Population-Based Protocols to Individualized Therapies Happening?
For decades, treatment plans were built around population averages – not people. It’s efficient, it’s evidence-based, but it rarely accounts for what makes each patient different: their genes, chronic conditions, lifestyle, even how they respond to medication over time. That gap between what’s standard and what’s personal? That’s where AI in personalized medicine is changing the game.
That’s where the shift is happening.
With AI for individualized treatment, we’re seeing the ability to analyze data points that go well beyond traditional EHR snapshots. Machine learning in disease treatment enables systems to recognize patterns across vast and diverse datasets – capturing the subtleties of how a specific patient may respond to a given therapy. Factors like metabolic differences, rare mutations, or overlapping chronic conditions are no longer barriers – they’re inputs.
That’s where deep learning in medical treatment is proving its worth. These algorithms aren’t just crunching numbers, they are recognizing patterns across EHR data, test results, imaging, and genetic markers that would take human teams weeks to untangle. They surface potential connections, risks, or opportunities which can directly help shape more precise, relevant therapies.
The real change? We’re starting to see AI-powered diagnosis and treatment plans tailored to a person’s actual clinical fingerprint, not a generalized template. This is AI for individualized treatment at work helping doctors fine-tune dosages, spot ineffective therapies earlier, and even design long-term care paths that account for someone’s real-world behaviors and conditions.
We’re not replacing doctors. We are simply giving them tools to finally treat patients the way medicine always intended: personally.
How Does AI Power Personalized Diagnosis and Treatment?
Modern healthcare has no shortage of data. Every patient encounter generates lab results, scans, EHR notes, genomic profiles and yet, much of this information lives in disconnected systems that rarely “talk” to each other. The real opportunity with AI in personalized treatment plans is its ability to bring all the data together and extract something that is clinically useful from it.
Instead of depending on manual cross-referencing or one-size-fits-all decision trees, AI tools can parse electronic health records, genetic data, even imaging studies all in one sweep. The goal? To turn noise into direction. What used to take days of review can now be distilled into AI-powered diagnosis and treatment plans tailored to the patient in front of you.
And this is where the shift truly matters. With the help of smart health platforms for personalized care, clinicians aren’t just looking at faster workflows – they’re seeing earlier interventions, clearer drug response predictions, and care plans that reflect a person’s actual medical history, not just statistical probabilities.
Take oncology, for example. Frederick Health implemented MEDITECH’s Expanse Genomics platform to allow clinicians to order and review genetic tests directly from within their EHR workflows. At one cancer center, clinicians saw a bottleneck: genomic test results were sitting in PDFs, while treatment decisions were happening elsewhere. So they built a workflow where genetic profiles could feed directly into the systems doctors already used. Suddenly, tumor board reviews became faster, and treatment choices more targeted.
This shift didn’t require a total reinvention – just the right data in the right place at the right time. It’s a working example of AI and patient-specific therapies being used not as a future goal, but as part of day-to-day clinical decisions. When hospitals streamline how complex data supports real patients, the promise of personalization becomes very real, very quickly.
In chronic disease management, machine learning is helping predict high-risk events well in advance. A Google AI study published in npj Digital Medicine trained deep learning models on de-identified EHRs from over 216,000 patients to predict hospital readmission and mortality. These models achieved high accuracy in forecasting outcomes, showing how deep learning in medical treatment supports proactive care.
Another example is Doctor AI, a predictive model developed by Sutter Health and researchers at UCSF using Recurrent Neural Networks to anticipate future diagnoses. The tool, referenced in a KDD Conference paper, demonstrated strong performance in predicting ICD-9 codes based on past visits. This represents the power of machine learning in disease treatment for streamlining care delivery and improving resource allocation.
At one hospital we consulted with, Care.ai’s platform became a turning point. Instead of depending on staff rounds or routine checkups, the system used ambient sensors and AI to quietly monitor patient activity picking up subtle changes that could signal a fall risk or early signs of infection. What made the difference was how it could pull everything together: live vitals, EHR data, even camera inputs – all becoming inputs for a real-time dashboard.
This is the kind of shift we’re seeing with smart health platforms for personalized care. The magic isn’t just in the data they collect, it’s in the way they analyze it. Through ongoing patient data analysis for treatment, these systems help clinicians intervene earlier, personalize care more accurately, and spend less time reacting and more time anticipating.
Looking to streamline diagnosis and deliver truly personalized treatment?.
Which Disease Areas Are Seeing the Most Impact?
While AI’s capabilities are often discussed in sweeping terms, its most profound impact lies in how it is transforming disease-specific treatment plans. Across a wide spectrum from high-burden chronic illnesses to rare genetic disorders – AI in personalized medicine is enabling hyper-targeted interventions that adapt to the individual rather than generalizing across populations.
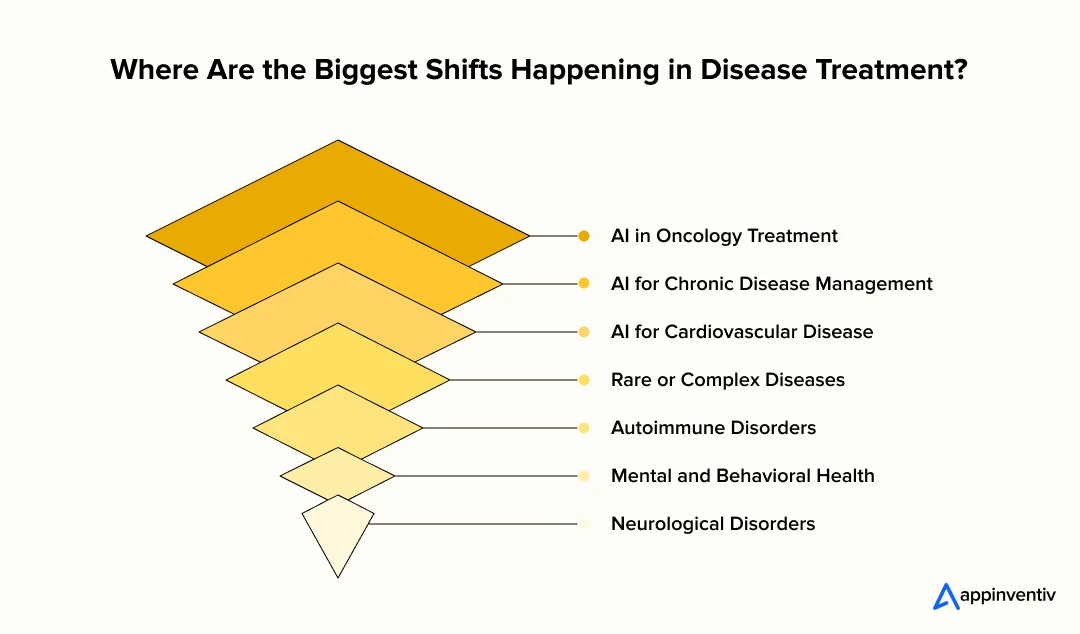
AI in Oncology Treatment
Cancer care is leading the charge in personalized medicine. These days, cancer treatment is starting to look very different from what it was even a few years ago. Doctors aren’t just going by cancer type anymore they’re digging into the genetics of the tumor. Tools like Tempus or IBM Watson for Oncology help with this. They use AI in oncology treatment to figure out which therapies might actually work, based on the patient’s own tumor profile. And it’s not just about picking the right drug – sometimes the AI suggests tweaking the chemo plan mid-way, depending on how the patient is responding. This is where genomic data and AI in personalized medicine really start to show their power.
AI for Chronic Disease Management
Chronic diseases don’t follow a schedule, they flare up in patterns shaped by sleep, stress, food, and a dozen other invisible cues. That’s where AI for chronic disease management is beginning to show real value. Platforms such Livongo and Omada don’t just log vitals; they learn from them. As patient behaviors shift it could be a skipped walk, rising glucose, or erratic sleep – the system adjusts its nudges, flags risks, and, when needed, brings in a clinician. It’s subtle but powerful: a digital hand on the shoulder, watching for changes long before they turn critical.
AI for Cardiovascular Disease
Heart disease remains the leading cause of death in the United States, but detection is starting to look very different. At the Mayo Clinic, algorithms trained on thousands of ECG records have picked up early signs of atrial fibrillation often before symptoms begin. Google’s health research arm has worked on similar models, layering imaging and wearable data to flag early signs of heart failure. This shift isn’t about replacing clinical intuition; it’s about giving cardiologists an earlier window into patient risk, when decisions can still change outcomes. The advantage lies in timing, not just accuracy
Rare or Complex Diseases
Patients with rare diseases often face delays in diagnosis simply because there isn’t enough clinical data for doctors to act on. But newer tools are helping close that gap. Some platforms now combine genomics with natural language processing to examine patterns in smaller datasets. Deep Genomics, for example, has worked on rare metabolic conditions, while inference is helping flag possible diagnoses earlier. These use cases show how AI in personalized treatment plans can unlock answers even when traditional approaches stall.
Also Read: 10 Use Cases on How AI is Transforming Genomics
Autoimmune Disorders
Autoimmune conditions don’t follow a script. One month a medication works, the next it doesn’t. That’s where AI has started to earn its place, not by making the decisions, but by watching closely. It looks at changes in lab tests, MRI scans, even how a patient reports feeling day to day. When something starts to shift, the system flags it. Sometimes it’s a dosage tweak, sometimes a combination that might work better. What we’re seeing is a move toward care that can adjust as the body does. That’s really what AI-driven precision medicine is about not a one-time treatment, but an ongoing, personalized response.
Mental and Behavioral Health
There’s been a quiet shift in how we think about mental health care. More people are turning to digital companions – not to replace therapy, but to bridge the in-between. Apps like Woebot and Ginger aren’t trying to act like doctors.
What they are doing is listening, nudging, and making space for people who might not pick up the phone to call a therapist. That matters. Because when anxiety creeps in at 2 a.m., or when depressive lows go unnoticed for weeks, AI-backed mental health tools can catch the signals and prompt action early. This is where digital therapeutics and AI are starting to show real value especially for communities that don’t always get seen.
Also Read: A Comprehensive Guide to Mental Health App Development
Neurological Disorders
Some neurological conditions don’t start with clear symptoms like a tremor or memory loss. That is where AI makes a mark. By studying voice changes, subtle shifts in how someone walks, or even brainwave signals, it’s helping doctors notice what might’ve gone unseen for months. Tools are already being tested for Parkinson’s, Alzheimer’s, and epilepsy spotting early signs before they become harder to manage. It’s not perfect, but it’s a step forward. Personalized treatment paths are then developed using a combination of neuroimaging and predictive modeling, truly a new frontier in AI in personalized medicine.
Learn how we implemented voice commands, head gestures, and customizable requests to create an inclusive communication platform that serves all patients, regardless of mobility.
Across these domains, the benefits of AI in tailored medical treatments are evident from digital therapeutics and AI-powered diagnosis to real-time, patient-specific therapies. What once needed months of trial-and-error can now get compressed into focused, data-driven care plans that are built upon live feedback loops and genomic insight.
Transforming Drug Discovery and Treatment Matching
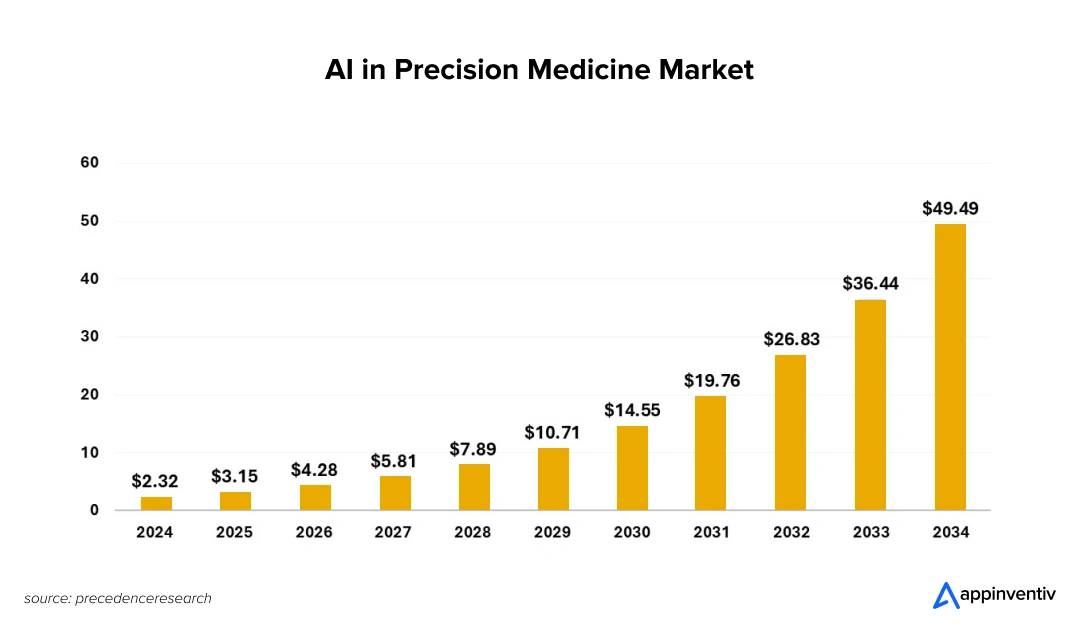
One of the most beneficial uses of AI in personalized treatment plans is how it has been reshaping drug discovery and therapy selection. For years, the process has been considered a high-risk, slow-moving process that takes 10 to 15 years and billions in investment to bring a single therapy to market. With personalized drug discovery with AI, however, these timelines are being shortened, and the outcomes are becoming more targeted.
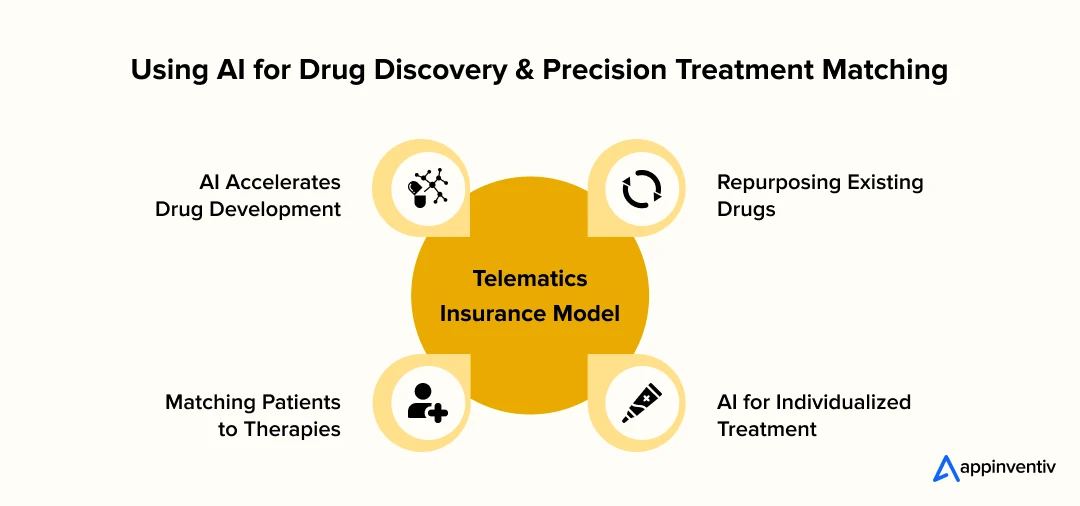
AI Accelerates Drug Development
AI models can simulate how every new compound interacts with human proteins, cutting down the time earlier spent on lab testing. Platforms like DeepMind’s AlphaFold have cracked the protein folding problem, enabling researchers to predict protein structures with unmatched accuracy – unlocking faster screening of molecules for specific diseases, especially genetic and rare conditions.
Repurposing What Already Works
Some of the biggest breakthroughs in medicine don’t always come from brand-new drugs – sometimes, they come from using old ones differently. That’s where AI is starting to make a real impact. During the early COVID days, when time was tight, researchers used AI tools to comb through approved medications, hoping to find anything that could match the virus’s structure. And a few options actually showed promise. Now, if that same process is applied to cancer or autoimmune diseases? It could speed things up massively. We’re talking about treatments with known safety records – getting to patients quicker, with fewer unknowns.
Matching Patients to Therapies, Not the Other Way Around
Traditionally, patients are fitted to broad treatment categories. But AI-driven precision medicine flips that model – analyzing each patient’s clinical, lifestyle, and genomic data to recommend interventions tailored to their biology. This is where genomic data and AI in personalized medicine come together to do something traditional methods simply can’t.
Take a cancer patient undergoing genomic profiling. Instead of depending entirely on population-wide treatment protocols, an AI system scans their gene variants to understand how they can metabolize different drugs. It fags treatments that are likely to work, highlights potential risks, and even suggests tailored dosages – often before a clinician has even finalized a plan.
In real-world settings, this isn’t theoretical. Platforms like Tempus, Foundation Medicine, and PathAI are already part of clinical workflows – using real-time data and predictive models to guide more targeted, precise therapies for oncology patients.
These tools aren’t theoretical; they are already helping clinicians treat individuals with greater accuracy.
AI for Individualized Treatment Matching
At the core of this shift is AI for individualized treatment – systems that don’t just stop at diagnosing, but actually help shape what happens next.
Let’s say a patient’s care team has access to their genomic profile, medical history, recent scans, and even lifestyle habits. With this rich data available in-hand, instead of guessing which drug might work best, the AI pulls all of it together – spotting patterns that a human doctor might miss. It weighs risk factors, compares outcomes, and recommends a protocol likely to work for that specific patient, not just someone like them.
The result? Fewer dead ends. Faster responses. And a treatment path that adapts over time, instead of getting locked in too early.
How Generative AI Is Shaping Truly Personalized Treatment Plans
Most of what we think of as “AI in medicine” so far has been about pattern recognition—finding signals in EHRs, scans, or genomics. But the next leap is happening right now with generative AI (Gen AI): systems that don’t just analyze data, but can actually create new, clinically relevant content or simulate scenarios for individual patients.
So what does that mean in practice?
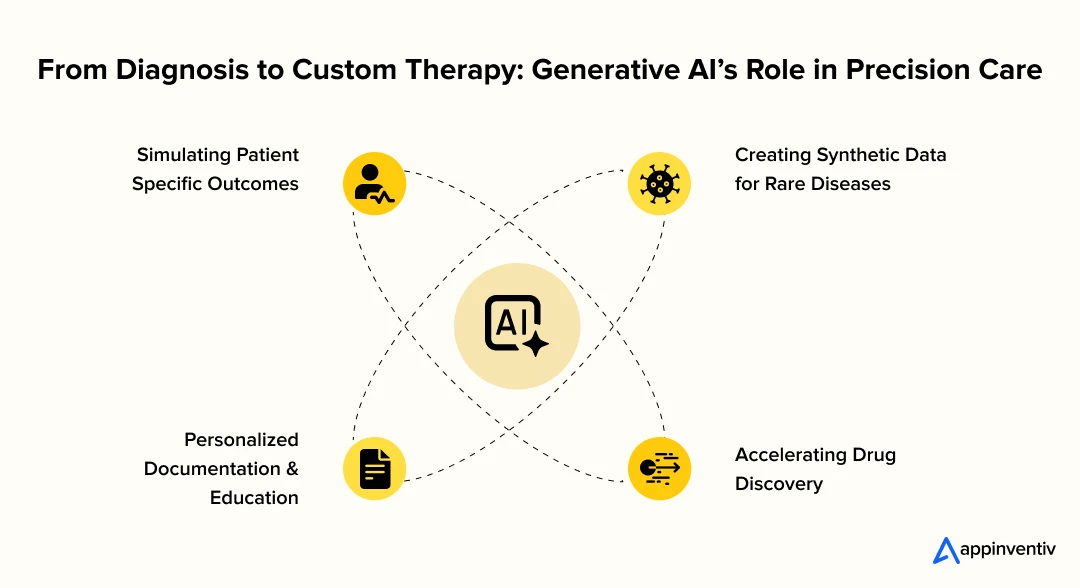
Simulating Patient-Specific Outcomes
Generative AI models can take a patient’s unique profile—genetics, medical history, lifestyle—and simulate how they might respond to different therapies. Instead of just matching to existing cases, Gen AI can forecast potential outcomes for new or rare combinations, giving clinicians a “what if” toolkit for complex cases.
Creating Synthetic Data for Rare Diseases
For rare conditions, data is often too sparse for traditional AI. Gen AI can generate synthetic patient data that mimics real cases, helping researchers and clinicians test new treatments or identify patterns that would otherwise remain hidden.
Personalized Documentation and Education
Gen AI can draft personalized care plans, patient summaries, and even educational materials tailored to the individual’s needs and comprehension level—saving clinicians time and making care more accessible for patients.
Accelerating Drug Discovery
By simulating how new compounds might interact with unique patient biology, Gen AI is speeding up drug development and matching therapies to the right individuals faster than ever before.
What’s the catch?
With all this power comes responsibility: these systems need careful validation, transparency, and oversight to avoid bias and ensure safety. But as Gen AI becomes part of the clinical toolkit, it’s opening up new frontiers in how precisely we can tailor care—moving from “what’s worked before” to “what’s possible for this patient, right now.”
Generative AI is still in its early stages of adoption across many industries, and organizations are exploring its potential to drive efficiency, innovation, and cost savings. Yet, one critical question remains: does it truly deliver measurable value?
According to a recent McKinsey report, while only a small share of respondents have fully implemented generative AI, nearly 60% believe it is already yielding a positive ROI. However, few have formally quantified its impact, with many still waiting for concrete, measurable results.
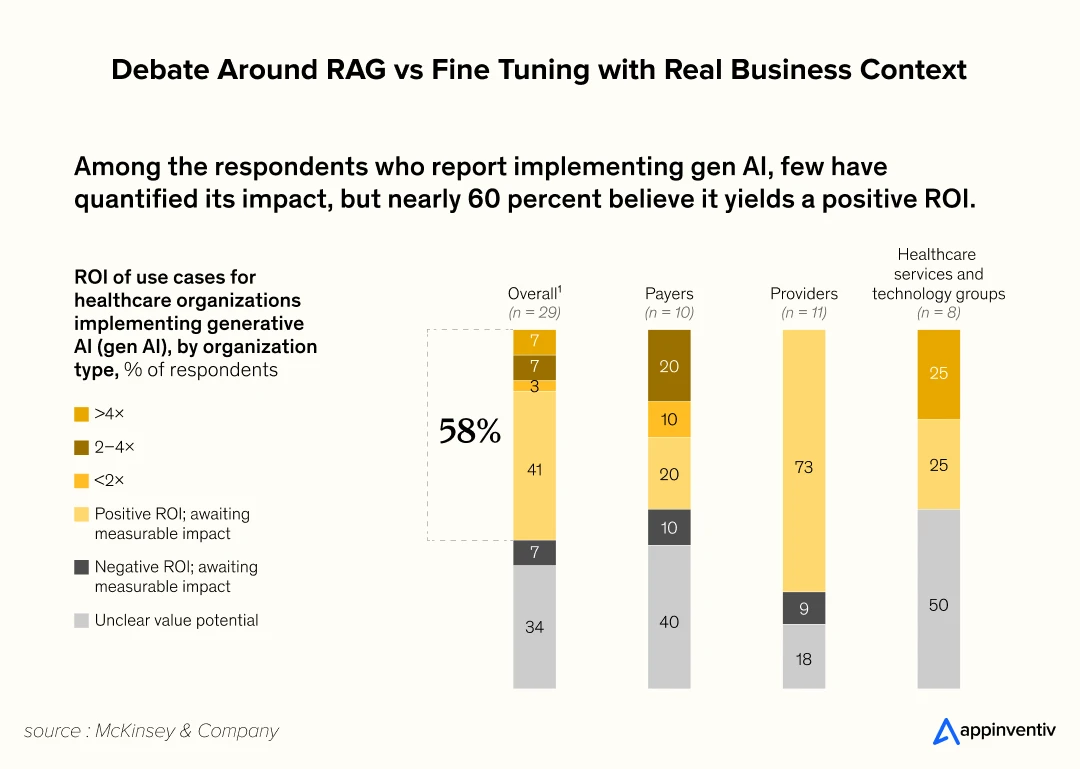
Like any major investment, demonstrating clear value is essential. Tangible outcomes not only validate the technology but also build confidence for broader adoption and further investment. Among those who have deployed generative AI, most either already see positive returns or expect to in the near future.
Also Read: Generative AI in Healthcare – 10 Use Cases and Examples
The Role of Digital Therapeutics in Personalized Care
A prescription tells you what to take. But staying on track? That’s a whole different story and that is where digital therapeutics step in – not as generic apps, but as structured tools designed to support people between clinic visits, especially ones suffering from long-term conditions like diabetes, anxiety, or insomnia.
Picture someone living with type 2 diabetes using a digital program to manage their daily routines – meals, meds, stress. At first, it sends a few nudges about breakfast timing. Nothing fancy. But a few weeks in, the system notices a pattern: blood sugar spikes tend to follow bad sleep or missed meals. Instead of repeating the same reminders, it changes course. Now the app focuses on improving sleep habits and making mornings more predictable.
It’s not just logging data. It’s adjusting to behaviour, in real time. AI makes it possible not by automating care, but by personalising it, quietly, behind the scenes.
Discover how we built the DiabeticU platform, a HIPAA-compliant, cloud-native platform that leverages AI to deliver personalized meal plans, track prescriptions, and provide real-time wellness recommendations.
Companion Tools for Complex Conditions
In AI in oncology treatment, digital therapeutics are no longer just nice-to-haves – they’re becoming everyday lifelines. Think less clipboard, more companions. You’ve got a cancer patient juggling meds, side effects, stress. This isn’t something a check-up every three weeks can catch in time. But the system? It’s there daily. It tracks if meds are skipped, notices a subtle rise in symptoms, maybe even flags that things are off before the patient realises. Sometimes it’ll suggest a gentle nudge. Other times, it’ll raise the flag for clinical teams to step in. Either way, it’s tuned in. Quietly supporting, always learning.
Optimizing for Adherence and Outcomes
Let’s be honest – adherence is where so many treatments fall apart. People forget. They lose motivation. Life gets in the way. But AI isn’t just another reminder system. It studies what causes people to drop off. Maybe it’s energy dips in the afternoon. Maybe weekends throw off the rhythm. Over time, it gets smart about it. Therapy prompts shift. Delivery changes. And suddenly, that “hard-to-stick-with” treatment fits into the person’s life more naturally. That’s the difference, convenience with clinical impact. Not just better compliance, but better outcomes.
From Drug to Digital to Data
Here’s where it gets interesting. The patient uses a digital therapeutic. That data doesn’t just sit somewhere – it flows back into the system. AI picks up patterns. Maybe the therapy’s working, maybe it needs a tweak and at some point, the system might even recommend a change in medication based on how someone’s responding day-to-day. That’s personalized drug discovery with AI in action, not a static prescription, but a care model that adjusts, refines, and learns as it goes. Digital and drugs aren’t separate lanes anymore. They feed each other. It’s still medicine but smarter, faster, more tuned in to the person at the centre of it all.
What are the Ethical Considerations to Prepare for AI-Driven Personalized Care?
There’s no doubt that AI is transforming personalized care. But as the wins pile up – faster diagnoses, smarter therapies – we also need to keep our footing. The expectations of better outcomes should never overrule the responsibility that comes with them. Especially when it comes to AI-powered diagnosis and treatment plans where trust, autonomy, and safety are not optional but a definite non-negotiable.
So yes, the tech is impressive. But the ethical considerations of AI in healthcare? They’re what determine whether that tech actually improves lives – or quietly reinforces old inequalities.
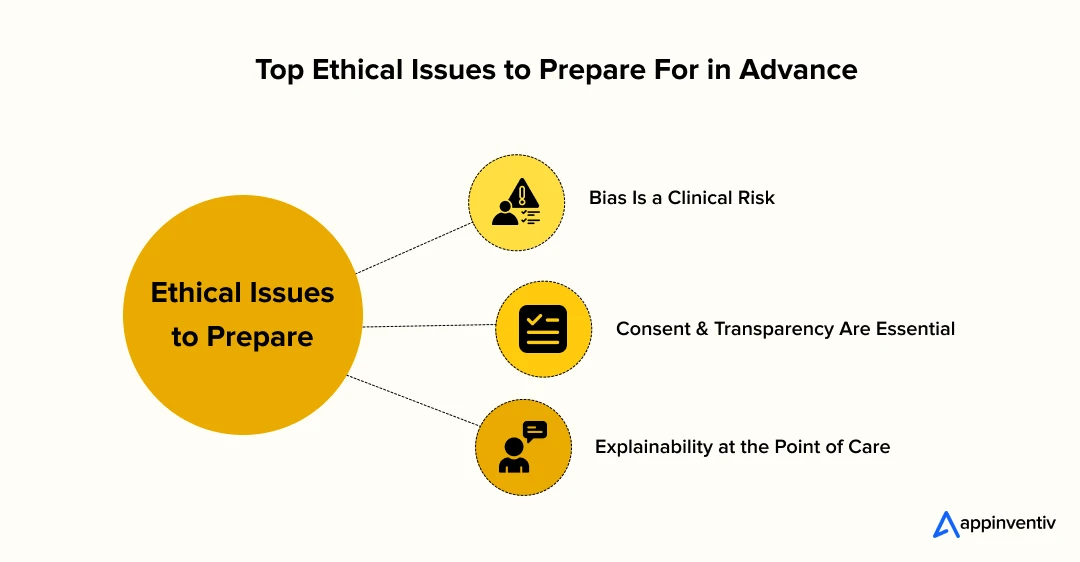
Algorithmic Bias Isn’t Just a Technical Flaw It’s a Clinical Risk
Here’s the problem. Machine learning in disease treatment is only as good as the data it learns from. And if that data skews, more samples from one ethnicity, gender, or age group, the AI’s recommendations will skew too. In the world of personalized medicine, that’s not just inconvenient. It’s dangerous.
What starts as a small data gap can lead to real-world harm: missed diagnoses, unequal treatment access, or biased clinical decisions. This isn’t a future problem. It’s already here.
The fix? It starts early – with bias audits during development and continues with real-world monitoring after deployment. Fairness can’t be patched in later. It has to be built in from day one.
Consent and Transparency Must Be Built In
The more advanced AI and patient-specific therapies get, the more data they need to operate. Genomics, wearables, EHRs, even lifestyle habits – it’s all up for grabs. But when does helpful insight cross the line and become “too much”?
Patients need to know exactly what data is being collected, why, and who gets access to them. And that consent? It can’t be buried in fine print. If we’re evolving the tech, the way we ask for permission has to evolve too. Transparency isn’t just a compliance checkbox. It’s what earns long-term trust.
Explainability Matters Especially at the Point of Care
A black-box algorithm might work in finance. In healthcare? Not so much. When AI-powered diagnosis and treatment plans are driving high-stakes decisions, maybe through cancer care or multi-drug management clinicians need to know why the AI suggested what it did.
That’s where explainable AI steps in. Not just outputs, but reasoning. Not just results, but confidence levels. If a doctor can’t explain a recommendation to a patient, how can they both trust it?
In the end, building ethical, explainable, and transparent systems isn’t about slowing down. It’s about scaling safely. Because machine learning in disease treatment isn’t just shaping medicine – it’s shaping people’s lives.
What is the Future of AI in Personalized Healthcare?
We’re no longer talking about the future of AI in personalized healthcare like it’s something years away. It’s already starting to show up in clinical pilots, in R&D hubs, even in the ways patients are being monitored today. The next wave? It’s not just smarter algorithms. It’s deeper integration. Every new layer of personal data – genomic, behavioural, environmental – is being pulled into a single, dynamic system. One that doesn’t just recommend treatment, but evolves with it.
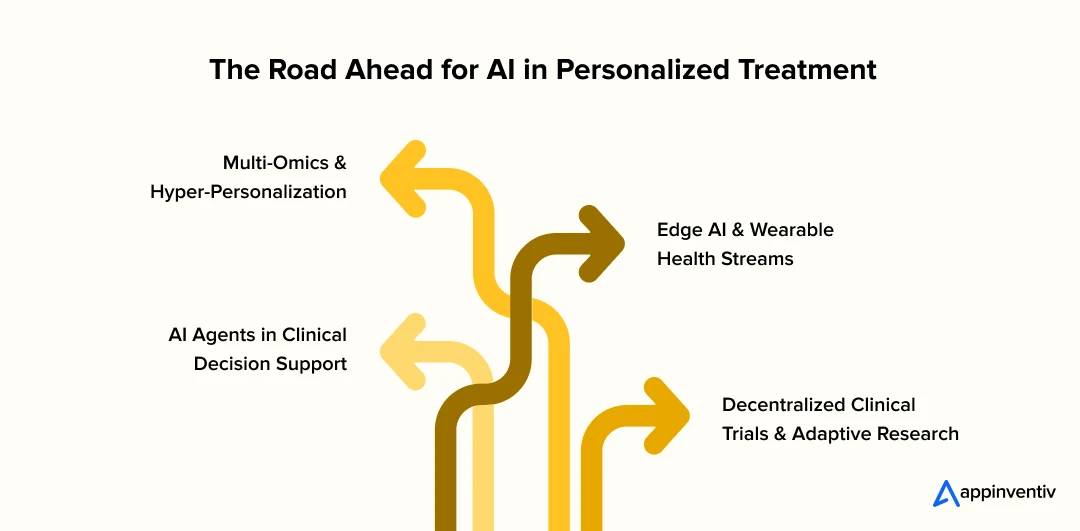
Multi-Omics and Hyper-Personalization
Right now, we’re just scratching the surface. AI in personalized treatment plans is heading into territory that goes well beyond genomics. We’re seeing algorithms decode proteomic shifts, microbiome imbalances, and metabolic markers – each adding new context to how a patient might respond to therapy.
It’s what the industry calls “multi-omics,” but in simpler terms – it’s the full-body picture. The power here lies in the detail. It means two patients with the same diagnosis won’t get the same care. That’s AI-driven precision medicine – less protocol, more person.
Edge AI and Wearable Health Streams
Until recently, health data had to travel – first to the cloud, then to the clinician, then back to the patient. But that’s changing. Thanks to edge AI, analysis is happening right on the device. A glucose monitor doesn’t just log numbers anymore, it learns patterns and adjusts, instantly.
This shift is huge for AI for chronic disease management. You’re not waiting on labs or weekly check-ins. You’ve got a system responding in the moment – whether it’s adjusting medication doses or spotting early warning signs before symptoms even start.
AI Agents in Clinical Decision Support
Doctors already have enough on their plates. But once you give them an AI co-pilot – one that can scan patient data, highlight risks, cross-check global trials in seconds they suddenly get time back. That’s why AI and patient-specific therapies are gaining traction – not for replacing decisions, but reinforcing them.
We’re talking about agents that don’t sleep, don’t overlook red flags, and never get overwhelmed. In high-stakes cases like oncology, that kind of backup is not just helpful – it could be lifesaving.
Also Read: How Much Does It Cost to Develop an AI Agent?
Decentralized Clinical Trials and Adaptive Research
There’s also a massive shift happening behind the scenes in how research is run. Forget clinical labs. Patients are enrolling, participating, and sharing data from their homes. AI-driven precision medicine is making these decentralized trials smarter, faster, and more inclusive.
AI adapts the study in real time. If a participant responds poorly, the protocol can adjust. If a treatment shows promise earlier than expected, the system learns. For researchers, it means real-world insight without waiting months for analysis. For patients, it’s a more responsive, less invasive experience.
What This Means for the Industry
Here’s the bottom line: Personalization in Healthcare isn’t a bonus feature anymore. It’s the baseline – health systems that still depend on one-size-fits-all approaches are going to feel increasingly outdated. To build what’s next in AI and patient-specific therapies, the focus should not just be on innovation – but also on integration. Can you make it work in real clinics? Can it talk to existing systems? Can it scale without losing safety or trust?
Because at the end of the day, the real breakthrough in AI-driven precision medicine won’t be in a lab. It’ll be in a patient’s life where it makes care feel less like a system, and more like it was made just for them.
The next step is scaling it safely, meaningfully, and in real-world settings.
How AI is Shaping Personalized Care & How Appinventiv Can Help
If you’re running a hospital or care network today, you’re likely not asking if AI fits in – you’re asking where to start without disrupting everything else. That’s the real shift. Because AI in personalized medicine is no longer just an innovation strategy; it’s quickly becoming part of daily clinical logic.
And no, you don’t need to blow up your whole system to begin. A few smart, low-friction moves can lay the right foundation.
What to Adopt Now:
- AI-powered diagnosis and treatment plans are already being used in places like dermatology and radiology. Start there and let the AI help sort patients and surface insights, especially in places where the case volumes are high and time is limited.
- Real-time patient data analysis for treatment decisions doesn’t have to be futuristic. Just having a unified view – lab results, images, history – in one interface can cut decision lag and reduce errors.
- Digital therapeutics can quietly extend your reach without demanding a system overhaul. They’re not replacing clinicians – but they’re helping patients stick to plans and report how they’re doing in between visits.
What to Prepare For:
- If you haven’t already, start conversations with genomics labs or AI research hubs. You’ll need partnerships to move into deeper personalization. That’s the direction most advanced players are heading in.
- One of the big challenges of implementing AI in personalized care is trust – both from your clinicians and your patients. If it feels like a black box, it’ll get pushback. Design for explainability, not just accuracy.
- And finally, infrastructure. Doesn’t have to be flashy, but it does need to be solid. Especially with data. The more sensitive and personal the inputs are, the more critical it will be to build with compliance and future-proofing in mind.
Appinventiv is an ISO certified, Deloitte awarded healthcare software development services company. We have worked with global health systems, hospitals, and research startups to build custom healthtech solutions – from AI-driven diagnostic tools and remote monitoring platforms to genomic data integrations and consent-based health record systems. Our AI services and solutions are built with compliance, scalability, and clinical efficacy in mind.
You don’t need some massive AI lab or overhaul to get started. Even if you’re just beginning to explore AI for individualized treatment, or your team’s already rolling with advanced workflows, it usually comes down to one thing: what fits in your clinical reality. We help figure that out – tech, compliance, people – all of it.
Our goal? Get you moving with the right tech, on your timeline, in a way that’s compliant and future-proof. Not theoretical. Practical. Get in touch!
FAQs
Q. How AI transforms healthcare delivery?
A. It’s different for every team. Like, how AI transforms healthcare delivery might just mean cutting down on time spent digging through records. For someone else, it could be catching things in lab reports a bit earlier – nothing fancy, just useful. And yes, in some places it does heavier lifting like suggesting what to look at next or flagging someone who might need attention soon. It’s no where a magic fix, but when you’re short on time and juggling ten things, even small shifts like that can help a lot.
Q. What are examples of AI in disease treatment?
A. You’ll see a lot happening in oncology, where AI helps with tumor profiling, or in cardiology with wearables catching early signs of arrhythmia. Chronic care platforms are using it too – watching trends in blood sugar or blood pressure in real time and nudging the patient before things get worse. These aren’t experimental anymore – they are already in rollout across some major systems.
Q. What are the best AI platforms for personalized medicine?
A. Some of the strongest players right now in AI in personalized medicine are Tempus, Owkin, IBM Watson Health, and PathAI. They’re not just building algorithms, they are embedding themselves into hospital workflows or working directly with genomic data to personalise treatment options. Many of them are also designed to work with existing EHR systems, which makes adoption easier.
Q. How to use AI in personalized treatment plans and medicine?
A. When it comes to how to use AI in personalized medicine and treatment plans, I’d say don’t overthink the first step. Most teams start by just connecting the dots – genetic info, lab results, vitals, all in one place. From there, you let the system highlight what’s worth looking at. You’re not handing the wheel to AI, you’re just letting it spot patterns faster than a person can. As trust builds, you can go deeper – treatment matching, response prediction, that sort of thing. But honestly? Just surfacing what matters is already a win.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
The Enterprise Buyer’s Checklist Before Hiring an AI Development Partner
Key takeaways: Choosing an AI development partner is less about technical demos and more about real-world fit, governance, and operational reliability. Internal alignment on outcomes, data ownership, and integration realities is essential before engaging any enterprise AI partner. Strong partners demonstrate delivery maturity through governance controls, security discipline, and lifecycle management, not just model accuracy.…

Proving the ROI of Copilot AI Sales Enablement Software for Global Teams
Key Takeaways The ROI of Copilot AI sales enablement software shows up in revenue moments, not in generic productivity reports. Organizations that treat Copilot as an AI-powered sales enablement platform tied to sales process maturity see measurable outcomes within two quarters. Global sales teams require region-aware deployment models to avoid uneven adoption and misleading ROI…

Real Estate Chatbot Development: Adoption and Use Cases for Modern Property Management
Key takeaways: Generative AI could contribute $110 billion to $180 billion in value across real estate processes, including marketing, leasing, and asset management. AI chatbots can improve lead generation outcomes by responding instantly and qualifying prospects. Early adopters report faster response times and improved customer engagement across digital channels. Conversational automation is emerging as a…