- What Is Telemental Health?
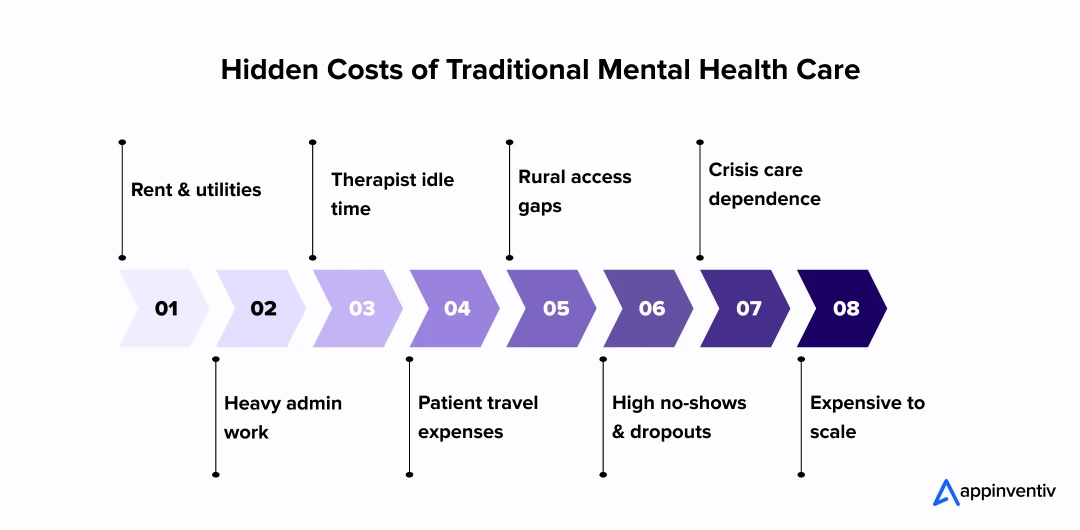
- Cost Challenges in Traditional Mental Health Care
- 1. Physical Infrastructure & Facilities
- 2. Operational Staff & Administrative Burden
- 3. Therapist Time Waste and Idle Gaps
- 4. Patient Travel and Time Costs
- 5. Geographic and Access Barriers
- 6. Drop-off and Continuity Problems
- 7. Crisis and Emergency Overuse
- 8. Scaling Limitations
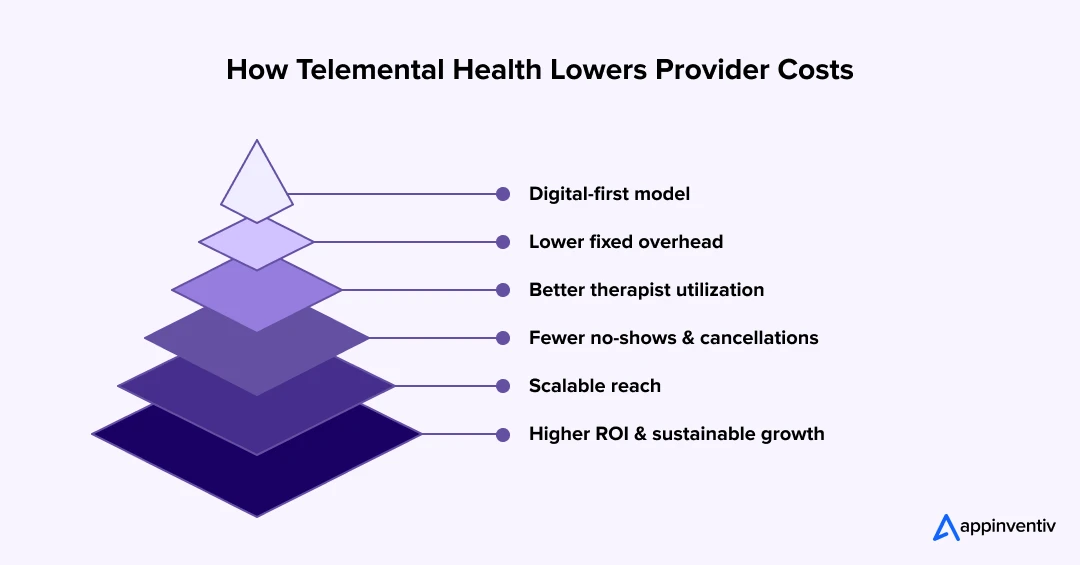
- Cost Benefits of Telemental Health for Healthcare Providers
- 1. Reduced Facility and Real Estate Costs
- 2. Higher Therapist Utilization and Efficiency
- 3. Reduced No-Show and Cancellation Rates
- 4. Scalable Reach Without Proportional Cost Increase
- 5. Lower Clinical and Administrative Overheads
- 6. Improved Access and Demand Management
- 7. Digital Transformation Synergies
- 8. Mitigating System Overload
- Cost Benefits of Telemental Health for Patients & Caregivers
- Real Life Examples of Telemental Health Services
- Kaiser Permanente – Making Mental Health Care Easier to Reach
- Cleveland Clinic – Bringing Therapy to Every Zip Code
- Cleveland Clinic and Ayble Health – Treating Body and Mind Together
- FTI Consulting – When Digital Care Makes Financial Sense
- Kaiser Permanente – Using AI to Support Clinicians, Not Replace Them
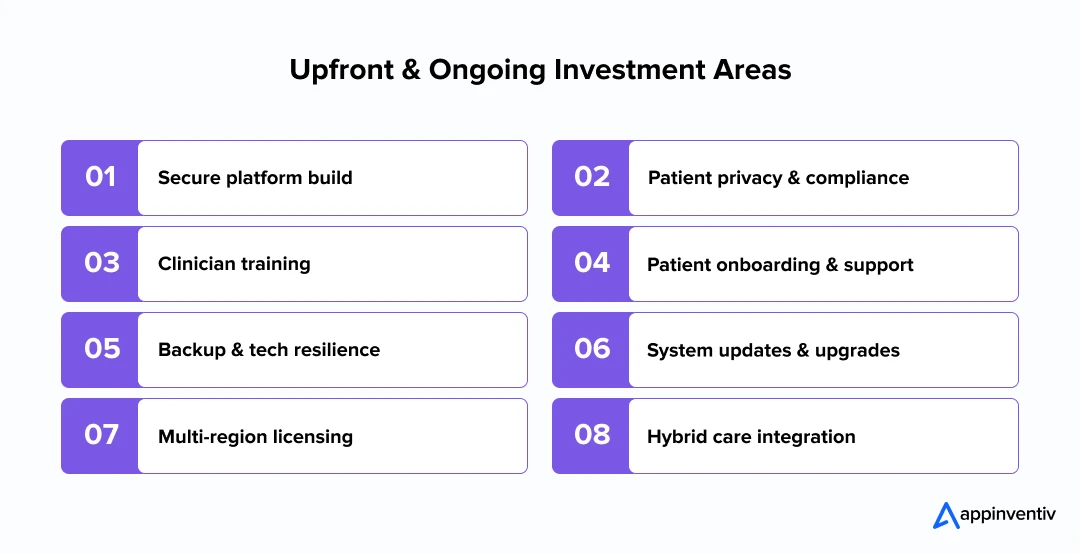
- Implementation Costs and Investment Considerations
- 1. Building the Right Platform
- 2. Protecting Patient Privacy
- 3. Helping Clinicians Adjust
- 4. Making It Easy for Patients to Start
- 5. Having a Backup Plan
- 6. Keeping the System Fresh
- 7. Navigating Rules and Licensing
- 8. Blending Digital and In-Person Care
- Investment Outlook
- Barriers, Risks and Mitigation Strategies
- Why This Matters
- Hybrid & In-Person Approaches
- Future Trends and Emerging Cost Levers
- 1. AI, Automation and Digital Triage Agents
- 2. Group Teletherapy and Peer Networks
- 3. Wearables and Passive Monitoring
- 4. VR and AR for Therapy
- 5. Cross-Border and Global Care
- 6. Value-Based Care and Outcomes Tracking
- 7. Smarter Connections to the Health Ecosystem
- 8. Supportive Policy and Subsidy Changes
- Why It Matters for Providers and Builders
- How Appinventiv Helps You Build Smarter Telemental Health Solutions
- FAQ’s
Key Takeaways
- Telemental health is cutting the heavy costs of running clinics and making it easier for people to get therapy when and where they need it.
- Seeing a therapist online saves time and travel money while helping clinics keep schedules full and care affordable.
- Secure digital platforms let therapists reach new patients without opening more offices, and people can join sessions from the comfort of home.
- Less rent to pay, fewer hours spent on paperwork, and fewer no-shows are changing how mental health care works behind the scenes.
- Quick check-ins and easier access help catch problems early so patients stay out of the ER and avoid expensive crises.
- Moving mental health care online is proving practical and cost-friendly for both providers trying to grow and patients trying to keep up with care.
Mental health care has always been expensive and hard to reach. Finding the right therapist, waiting weeks for an appointment, and managing the cost can feel overwhelming. Now, telemental health for healthcare providers is rewriting that story. With secure video sessions and smart digital platforms, healthcare providers can cut the expense of running physical clinics and reach people wherever they are.
This rapid adoption is also driving new models of telehealth for mental health providers, helping them reach more people without the heavy cost of physical expansion.
For patients, it’s just as life-changing. Telemental health for healthcare patients means no more long commutes, no lost work hours, and fewer reasons to skip therapy. This shift in telemental health for patients is helping more people stay consistent with therapy and avoid long-term complications. The help you need fits into your day, not the other way around. That convenience often leads to better follow-through and fewer costly crises later on.
What started as a quick fix during the pandemic has turned into something far bigger — a cost-effective way to get and give care. This article unpacks how telemental health is helping both providers and patients save money while keeping mental health support within reach.
What Is Telemental Health?
Think of telemental health as care that meets you where you are. No commuting, no waiting rooms, no racing the clock to make an appointment. Now therapy can happen over secure video, phone, or chat, right from the space where you feel most at ease.
For providers, it’s a way to break free from the limitations of a single clinic. This shift helps telemental health for healthcare providers cut location limits and deliver care to new communities.
Therapists can see patients who live hours away, fill schedule gaps more easily, and lower the cost of keeping a physical office running. Patients, in turn, get options that fit real life.
Telemental health isn’t a single set routine. For one person, it’s sitting down for a live video chat with a therapist. For another, it’s sending a message when things feel heavy and getting a reply later.
- Teletherapy or telepsychology: real-time video sessions that feel close to an in-person visit.
- Telepsychiatry: medication check-ins or follow-ups without the long trip to an office.
- Asynchronous counseling: voice notes or secure texts when you need to talk but can’t schedule a full session.
- Digital CBT and guided programs: self-paced tools with a professional quietly keeping watch.
- Quick check-ins: a few minutes to touch base and stop problems from snowballing. These short moments are a big reason virtual mental health consultations help people keep up with care without losing time to travel or waiting rooms.
Still, therapy online isn’t just another app. These conversations are private and often vulnerable. That’s why platforms have to meet tough standards like HIPAA and GDPR and be ready if someone suddenly needs help. Getting that right is what protects telemental health patient privacy and makes it safe to open up.
Traditional vs. Telemental Health Care Comparison
| Feature | Traditional In-Person | Telemental Health |
|---|---|---|
| Geographic reach | Limited to local patients | Accessible anywhere with reliable internet |
| Overhead (office, utilities) | High | Minimal; digital-first infrastructure |
| Patient travel & time | Significant | Reduced or none |
| Scheduling constraints | Fixed slots, gaps | More flexible, easier to fill |
| Continuity / no-shows | Higher drop-off rates | Often lower; easier to attend |
| Marginal cost to scale | Proportional | Lower as digital platforms scale more efficiently |
Use has grown sharply since the pandemic. Mental health now represents one of the biggest slices of virtual care. Many clinicians blend in-person and digital sessions so they can see more people and keep costs under control.
Telemental health isn’t a perfect substitute — crisis care or complex assessments still need a physical presence — but for most ongoing mental health needs, it’s proving reliable, safe, and much easier to scale.
Cost Challenges in Traditional Mental Health Care
To really understand why telemental health can be more cost-effective, it helps to look closely at where the expenses pile up in the traditional mental health system. Many of these costs are so ingrained that they’re easy to miss until you compare them with a digital-first model.
1. Physical Infrastructure & Facilities
Running a mental health clinic is expensive before a single patient walks in. Rent, utilities, maintenance, furnishing waiting rooms, and equipping therapy spaces all add up. According to TheraPlatform, maintaining multiple locations also increases IT and security needs because each office must be compliant and private. These are fixed costs that do not go away even if appointment slots remain empty.
Solution: Moving some or most sessions online reduces the need for large, costly spaces. Providers can operate with one smaller clinic or even fully virtual setups while still offering secure and professional care.
2. Operational Staff & Administrative Burden
Behind every therapy session is a long list of non-clinical work: scheduling, verifying insurance, billing, collecting payments, credentialing, and keeping patient records in line with privacy laws. Many clinics also have to invest in staff training for compliance and digital systems just to keep paperwork secure and audits clean. Every admin hour adds to the cost per patient.
Solution: Telemental health platforms can automate scheduling, billing, reminders, and documentation. Smart EHR/EMR integration means fewer manual updates, fewer errors, and less time spent on repetitive tasks.
3. Therapist Time Waste and Idle Gaps
Therapists often lose billable time because of no-shows, late cancellations, or travel between locations. HealthTech Magazine notes that mental health providers have historically struggled with keeping schedules full because of these unpredictabilities. That unused capacity is pure cost: the clinician is paid or scheduled, but revenue is lost.
Solution: Virtual appointments allow therapists to fill their schedule more consistently. If a patient cancels, another can be slotted in from a different location. Online platforms can also send automated reminders to reduce no-shows.
4. Patient Travel and Time Costs
From the patient’s side, each in-person visit is more than just the session fee. There is the cost of getting there — fuel or public transport fares — plus parking, time away from work, and sometimes arranging childcare. For people with limited resources, these costs quickly add up and become a barrier to continuing care. Missed appointments or early dropouts often happen because of these burdens.
Solution: Virtual mental health consultations remove travel entirely. Patients can join from home or work, saving money and time and making it easier to stick with care long term.
5. Geographic and Access Barriers
Rural and underserved communities face an additional layer of cost. Long distances to the nearest provider can make regular therapy unsustainable. McKinsey highlights that location remains one of the biggest drivers of access inequality. When people delay treatment because it is too far or too costly to reach, conditions often worsen and become more expensive to treat later.
Solution: Telemental health breaks the location barrier. Providers can see patients across cities or states, and patients can finally access care without expensive travel or relocation.
6. Drop-off and Continuity Problems
High no-show rates and early therapy dropout are chronic issues. Missed sessions waste appointment slots, break therapeutic progress, and lead to relapses that require more intensive and costly interventions later.
Solution: Digital platforms make it easier for patients to stay engaged through quick check-ins, asynchronous messaging, and reminder tools. More frequent, lower-friction contact keeps therapy consistent and outcomes stronger.
7. Crisis and Emergency Overuse
When people cannot access affordable, ongoing support, they often end up needing acute or emergency care during mental health crises. Those episodes are significantly more expensive than preventive therapy and can overwhelm providers’ resources.
Solution: Telemental health creates a safety net by offering early interventions and flexible follow-ups. Patients can reach help before a crisis escalates, reducing ER visits and emergency admissions.
8. Scaling Limitations
Expanding an in-person mental health practice is not as simple as hiring more therapists. New branches require leases, build-outs, local licensing, and additional support staff. Digital-first models scale much faster and cheaper, but traditional setups are locked into a high-capital approach.
Solution: Digital infrastructure grows without heavy physical investment. Providers can add clinicians, expand into new geographies, and meet demand spikes through scalable virtual platforms instead of opening new offices.
Together, these factors make the brick-and-mortar model financially fragile. The move to virtual care is a key part of digital transformation in healthcare, reducing overhead and improving scalability. And when done right, scaling telemental health for healthcare providers becomes less capital-intensive and far more flexible.
Cost Benefits of Telemental Health for Healthcare Providers
Telemental health is not just about convenience. When built with the right infrastructure, it can directly reduce the financial weight on mental health practices, hospitals, and large health systems. Here’s how it breaks down:
1. Reduced Facility and Real Estate Costs
Running a physical clinic is expensive. Rent, utilities, waiting areas, signage, and on-site security add up fast, especially if you are trying to serve multiple locations. By shifting sessions online, providers can scale back physical space or avoid opening new offices altogether.
TheraPlatform points out that digital-first models eliminate many location-based expenses while still letting clinicians maintain a professional and private care setting virtually. For many, this shift to telehealth for mental health providers has become a proven way to serve growing patient demand while keeping operations lean.
2. Higher Therapist Utilization and Efficiency
A big advantage of digital care is the ability to fill gaps in a clinician’s day. In traditional practice, time is lost to travel between offices, patient late arrivals, or cancellations. Virtual sessions reduce these dead spots.
Therapists can see patients back-to-back from one secure platform, helping them increase the number of billable hours per week without adding staff or rooms. Many practices now rely on mobile telemental health apps for providers to manage schedules more efficiently, keep patient data organized, and avoid the wasted time common in traditional setups.
3. Reduced No-Show and Cancellation Rates
Missed appointments drain resources. A single no-show means wasted time and no reimbursement. Virtual visits make it easier for patients to keep appointments, especially if travel, childcare, or work are barriers.
Studies cited by HealthTech Magazine show that convenience alone significantly cuts cancellation rates and directly improves revenue predictability.
4. Scalable Reach Without Proportional Cost Increase
Expanding an in-person practice means leasing new space, hiring staff, and managing new compliance obligations. Digital platforms work differently. Once the system is built, adding patients in new cities or states has minimal incremental cost, just bandwidth and platform fees.
McKinsey notes that many in-person visits could shift to virtual care without sacrificing outcomes and unlock significant cost efficiencies.
5. Lower Clinical and Administrative Overheads
Much of what makes healthcare expensive is not clinical, it is the paperwork. Virtual-first setups can automate intake forms, appointment reminders, billing, and EHR (Electronic Health Records) updates.
The result is less manual admin and fewer full-time staff hours per patient served.
6. Improved Access and Demand Management
One of the biggest economic advantages is being able to reach new patient populations without adding brick-and-mortar capacity. Virtual appointments help smooth out demand surges by giving providers more flexibility in scheduling and distribution of cases.
According to McKinsey, about $250 billion in outpatient spending may move to virtual settings as care delivery models evolve. Meanwhile, systems adopting AI, digital tools, and remote care pathways are projected to tap into hundreds of billions in net savings over time
7. Digital Transformation Synergies
When telehealth is paired with analytics and automation, savings go deeper. AI can help triage patients, flag those at risk of dropout, and streamline documentation.
McKinsey’s research shows that digital transformation in health systems could unlock 200 to 360 billion dollars in net global savings by 2030, largely by reducing inefficiencies and repetitive manual tasks.
8. Mitigating System Overload
Virtual mental health support helps keep more serious cases from spilling into emergency rooms or inpatient care.
By providing early, frequent, and affordable check-ins, health systems reduce the likelihood of acute episodes that require costly crisis response and hospital beds.
In short: The cost per additional patient served through telehealth tends to drop as volume grows. Margins improve because fixed expenses shrink and scheduling becomes more efficient. For providers and health systems, that translates into a business model that can expand reach without expanding overhead.
Cost Benefits of Telemental Health for Patients & Caregivers
When therapy moves online, patients and their caregivers often feel relief not just emotionally but financially. These savings are measurable and go beyond the price of a session. Virtual therapy platforms built with telemental health for healthcare patients in mind reduce costs beyond the session fee and make ongoing care easier to maintain.
- Less Travel, More Savings: A study published in The Journal of Urology / Urology Practice found patients saved an average of $152.78 per visit through telehealth by cutting out travel entirely. One appointment alone can produce meaningful savings, and these add up quickly over weeks or months.
- Time Saved and Work Preserved: In the same study, patients avoided hours of commuting time and in-clinic waiting. That extra time often means fewer hours lost at work, less stress, and more flexibility to attend to life’s other demands.
- Fewer Barriers for Remote or Mobility Limited Individuals: A review from the Rural Telehealth Research Center showed that cost savings were especially strong for patients living far away or in underserved areas. Most of the savings came from avoiding travel costs. For many in rural or mobility-restricted settings, telehealth is not a luxury but a lifeline.
- Cutting Caregiver and Childcare Costs: When therapy is virtual, patients do not have to arrange travel or backup help for family members. Caregivers often save on babysitters, transport, or coordination efforts, and these costs can become significant over time.
- Potential for Lower Session Prices: Because virtual-first providers typically run leaner operations, some pass those savings to patients in the form of more competitive rates. Lower overhead also means fewer additional “hidden costs” that often appear in the total price of care. As telemental health for patients grows, these savings become more visible and easier to measure over time.
- Better Continuity and Fewer Missed Sessions: One of the most important economic benefits is sticking to the plan. When attending therapy is easier, dropout rates fall. Better adherence means fewer missed sessions, fewer relapses, and less need for expensive crisis care in the future. By making it easier to stay consistent with therapy, virtual mental health consultations also help reduce long-term treatment costs for patients.
- Preventing Escalation to Emergency Care: Early and easy access can stop worsening conditions before they require hospitalization. Telehealth reduces the chance of patients needing costly emergency interventions or inpatient stays by letting them reach help sooner.
Real Life Examples of Telemental Health Services
Numbers alone are convincing, but real-world stories make the impact clear. Many healthcare organizations and companies that embraced telemental health have publicly shared how it reduced costs and improved access.
Kaiser Permanente – Making Mental Health Care Easier to Reach
Kaiser Permanente has spent years breaking down the old barriers between patients and therapy. Today, people can schedule sessions, join secure video calls, and use digital self-help tools all within one connected system. It’s not a separate “online service” — it’s simply part of how care works. That shift has made life easier for both sides. Clinicians don’t need to juggle physical offices, and patients don’t have to choose between therapy and a busy day. The setup feels more natural, more flexible, and a lot more affordable than the traditional clinic model.
Cleveland Clinic – Bringing Therapy to Every Zip Code
Cleveland Clinic’s virtual arm, simply called The Clinic, shows how digital care can stretch across an entire country without losing quality. Working with Amwell, it now serves patients in all 50 states — connecting them to psychiatrists, psychologists, and behavioral health specialists without the long waitlists that used to define the system. For patients in smaller towns, this isn’t just convenient — it’s access they’ve never had before. For Cleveland Clinic, it’s a way to manage demand more efficiently without opening new buildings or adding layers of cost.
Cleveland Clinic and Ayble Health – Treating Body and Mind Together
Cleveland Clinic’s collaboration with Ayble Health takes a thoughtful turn: it blends mental health care into chronic disease management. People dealing with digestive disorders can now access guided CBT sessions, mindfulness audio tracks, and therapist-backed emotional support — all inside the same virtual platform they use for medical treatment. It’s a simple idea with a big impact: healing the mind and body together instead of treating them as separate issues. The result is better treatment adherence, fewer flare-ups, and patients who feel seen beyond their symptoms.
FTI Consulting – When Digital Care Makes Financial Sense
FTI Consulting’s analysis on digital behavioral health paints a clear picture: investing in teletherapy and virtual platforms actually pays off. Health systems that went digital saw fewer last-minute cancellations, fewer hospitalizations, and better staff retention. AI-assisted check-ins and automated scheduling freed clinicians from repetitive admin work, letting them focus on patients instead of paperwork. What started as a crisis workaround during the pandemic has quietly evolved into a cost-efficient, patient-friendly system that keeps care continuous instead of reactive.
Kaiser Permanente – Using AI to Support Clinicians, Not Replace Them
Kaiser Permanente is also experimenting with artificial intelligence — not to replace human therapists but to make their jobs easier. Its AI-driven telehealth tools help flag patient needs, organize medical notes, and handle scheduling behind the scenes. The goal isn’t to make therapy faster, but to make it less stressful for providers and smoother for patients. In a system where clinician burnout is real, that kind of digital backup is priceless. It’s a small glimpse into what the next decade of mental health care could look like — humane, efficient, and deeply connected.
Implementation Costs and Investment Considerations
Telemental health can pay for itself, but it is not instant. The shift from an office-based setup to a digital one comes with real work. It is not just about choosing a video app. It is about building a service people trust and feel comfortable using and giving clinicians tools that let them work well online.
In fact, when estimating investments, our telemedicine app development cost guide offers benchmarks you can use.
1. Building the Right Platform
Think of the platform as your clinic’s new front door. It has to be private, stable, and easy to use. Many organizations now look for online therapy platforms for providers that combine compliance, patient engagement, and administrative automation from the start. Patients should log in without frustration. Clinicians should be able to pull up notes, schedule, and send prescriptions in the same place.
Using secure video and cloud hosting keeps costs predictable and avoids the risk of systems breaking when schedules get busy. Many organizations now invest in tele-behavioral health platforms development to create systems built for growth and long-term sustainability.
2. Protecting Patient Privacy
Mental health sessions often involve deeply personal conversations. People will only open up if they feel safe. Strong logins, clear consent steps, and encrypted storage are essential. Some clinics bring in outside experts to test their security.
Building HIPAA compliant teletherapy systems helps providers maintain patient trust while avoiding costly compliance issues later. These steps are crucial when you build a secure telemental health platforms that patients can trust from day one.
3. Helping Clinicians Adjust
For therapists, switching to a screen can feel strange at first. They may worry about losing connection or missing nonverbal signals. Short, practical training helps.
Things like reading micro expressions on video, keeping sessions warm and personal, and knowing what to do if someone is in crisis but not physically there make a difference.
4. Making It Easy for Patients to Start
Many patients are anxious before their first online session. Simple instructions and quick tech support can make the difference between showing up or canceling.
Some clinics run a short practice call so patients know how to log in and feel comfortable before real therapy begins.
5. Having a Backup Plan
Technology can fail. The best-run platforms still have moments when video freezes or a call drops. Having a plan, switching to audio, resending a link, or having support available keeps the session and revenue from being lost.
6. Keeping the System Fresh
After launch, the work does not stop. Platforms need updates, new security layers, and small usability improvements. Budgeting for this avoids breakdowns later and shows patients the service is reliable.
7. Navigating Rules and Licensing
Telehealth rules change by location. Some clinics need extra licenses to serve patients in other states or countries. Sorting this out upfront saves time and legal trouble.
Many teams work with compliance specialists early to avoid expensive delays later.
8. Blending Digital and In-Person Care
Online care should feel like part of the same clinic, not a separate branch. Clear workflows for emergencies, referrals, and in-person follow-ups help patients feel safe.
When something cannot be handled online, they should know exactly what happens next.
Investment Outlook
Most of these costs show up early, but they do not last forever. A well-designed platform helps telemental health for healthcare providers stay compliant and efficient as they scale operations. Once a digital service is running smoothly, missed appointments usually drop, schedules stay fuller, and you need less space and staff on-site. Many clinics report recovering their setup costs within about 12 to 24 months.
Barriers, Risks and Mitigation Strategies
The economic case for telemental health is strong, but success depends on solving practical challenges. Many of these are predictable and manageable with the right planning. Understanding the key challenges of Telehealth for mental health early allows providers to plan better and avoid costly mistakes.
| Barrier / Risk | Mitigation / Strategy |
|---|---|
| Regulatory and Licensing Fragmentation | Telehealth rules vary by region, which can slow expansion. Build early relationships with legal and compliance experts. Use multi-state or regional licensure, partner networks, or centralized credentialing services to reduce administrative burden. |
| Reimbursement and Payer Policies | Payment parity is not universal. Advocate for telehealth coverage with payers, negotiate contracts that support virtual care, and consider mixed billing models while reimbursement policies evolve. |
| Digital Divide and Access Gaps | Not every patient has reliable internet or modern devices. Offer audio-only options when video is not possible. Design mobile-first platforms that work on low bandwidth. Consider programs that help patients with connectivity costs. McKinsey emphasizes bridging this digital gap to truly scale access. |
| Security and Privacy Concerns | Mental health records are highly sensitive. Use HIPAA-grade encryption, clear consent flows, and strict vendor vetting. Schedule regular audits and risk assessments to stay ahead of compliance issues and reassure patients. |
| Clinical Limitations | Not every case is suitable for virtual therapy. Define clear escalation protocols for emergencies and integrate hybrid care models so clinicians can bring patients in when needed. |
| Resistance and Adoption Hesitancy | Some clinicians and patients are unsure about digital therapy. Run pilot programs, share success stories, and offer training to build confidence. Identify “clinician champions” who can model success and encourage adoption. |
| Quality and Trust | Patients need to know care quality is equal to in-person therapy. Use validated clinical measures, track outcomes, and collect anonymized patient feedback to continuously improve and show results. |
| Saturation and Competition | The virtual mental health space is growing quickly. Differentiate by specializing in a niche (e.g., pediatrics, trauma therapy), ensuring seamless integration with other health services, and demonstrating measurable outcomes. |
Why This Matters
Addressing these barriers early leads to faster adoption and stronger financial results. Providers who invest in compliance planning, patient-friendly design, and clinician training usually see smoother launches and achieve ROI sooner. Many of these early investments set the foundation for scalable digital tele behavioral for healthcare providers solutions that are both compliant and cost-efficient. It also builds long-term trust, which keeps both patients and payers engaged.
Hybrid & In-Person Approaches
In reality, many mental health providers adopt hybrid models: mixing virtual sessions with occasional in-person visits (e.g. intake, assessments, hands-on therapy).
When hybrid makes sense:
- Complex cases, assessments needing physical presence
- Groups or workshops
- Patients preferring occasional in-person rapport
Cost trade-offs:
- Hybrid retains some overhead, but allows flexible scaling
- Use virtual mode for routine follow-ups, check-ins, scaling staff
Providers can stratify patient types (simple vs complex) and allocate care modes accordingly, optimizing cost-efficiency without compromising quality.
Comparisons across models often show that virtual-first + hybrid fallback yields the best balance of cost, access, and clinical quality.
Future Trends and Emerging Cost Levers
Telemental health is growing fast, but it is far from finished. New ideas and technologies are making care easier to deliver and cheaper to run, while giving patients better ways to stay engaged. For anyone building or expanding digital mental health services, understanding where the field is heading can shape smart, future-ready investments. Staying on top of emerging trends for telemental health for healthcare helps providers invest in the right technology and remain competitive as the field evolves.
1. AI, Automation and Digital Triage Agents
AI is shifting from simple chatbots to tools that can actually support clinicians. Digital triage agents can collect details about symptoms, pick up on risk signals, and help route a patient to the right level of care. This means fewer wasted clinical hours and faster help for the patient.
From a development point of view, it calls for secure natural language tools, solid data privacy, and smart links to the EHR so clinicians get the right context without extra clicks.
For deeper insights, explore our detailed blog on AI in healthcare.
2. Group Teletherapy and Peer Networks
Therapy has long been one-to-one, but online spaces are making group support easier. A single therapist can guide several people with shared needs, cutting the cost for each participant.
Well-designed platforms can also let people form safe, moderated peer groups that keep them motivated between sessions — a low-cost way to support mental wellness at scale.
3. Wearables and Passive Monitoring
More patients now have smartwatches, sleep trackers, or mood apps. That data from these wearable apps/devices can help spot stress or relapse risk early. Developers who can bring that information into the therapy platform — in a way that is private and not overwhelming — make it possible for clinicians to act before a crisis happens.
Catching problems sooner avoids expensive emergency care later. And with these connected tools telemental health for healthcare patients becomes more personalized and proactive over time.
4. VR and AR for Therapy
Virtual reality therapy, once a niche idea, is becoming practical and affordable. It can help with phobias, PTSD, and stress in a controlled setting without needing long, specialized sessions.
If developers can integrate VR safely and simply into telehealth platforms, clinics can add high-impact treatment options without building new spaces or investing in extra staff.
5. Cross-Border and Global Care
Licensing and technology are opening doors for mental health professionals to serve patients beyond local boundaries. A therapist in one region could reach people in underserved areas somewhere else, provided compliance is handled well.
Building flexible tools that handle local regulations, multiple languages, and secure payments is becoming a competitive edge.
6. Value-Based Care and Outcomes Tracking
Paying only for sessions is slowly giving way to paying for results. Some insurers now reimburse based on measurable progress, not just time spent. Platforms that can track symptom improvement, medication follow-through, or engagement over time will help providers prove value and negotiate better reimbursement.
This is pushing demand for next-generation online therapy platforms for providers that can measure outcomes and support pay-for-performance models.
7. Smarter Connections to the Health Ecosystem
Mental health works best when it is not isolated. Platforms that link easily to primary care, pharmacies, or other digital health services help avoid duplicate work and improve outcomes. Interoperability also saves money for clinics and health systems by cutting down on inefficiencies.
Expanding telemonitoring mental health for patients providers will make these integrations even more powerful, allowing real-time data sharing while reducing unnecessary visits. As these integrations deepen, the demand for custom Tele-behavioral health platforms development will increase, allowing providers to create highly tailored and cost-efficient care networks.
8. Supportive Policy and Subsidy Changes
Governments are starting to back virtual mental health as a core part of care. New coverage rules, tax breaks, and direct funding could make digital therapy cheaper to offer and easier for patients to access. Tools that can adapt quickly to new regulations will stay ahead.
Why It Matters for Providers and Builders
The next wave of telemental health is about smarter, more connected systems, not just video calls. Providers who invest early in automation, wearable data, and outcome-based care will reduce costs and stand out in a crowded space.
For developers, the challenge is to build platforms that are secure, scalable, and simple for both clinicians and patients. Get that balance right and it becomes easier for clinics to grow while keeping mental health affordable.
How Appinventiv Helps You Build Smarter Telemental Health Solutions
Bringing telemental health for healthcare providers to life is not just about adding video calls. It is about making care simple to reach and safe to deliver, while keeping the costs manageable. Patients need to feel supported; clinicians need tools that do not slow them down.
At Appinventiv, we build technology to make that possible. Our telehealth app development services combine healthcare understanding with product thinking. We do not stop at the code, we look at the real work your team does and design around it.
- Safe and compliant: We build platforms that meet HIPAA and GDPR standards so both patients and providers know their information stays private. This approach also supports organizations building reliable digital tele behavioral for healthcare providers tools that can grow with demand and stay secure over time.
- Fits into your existing systems: We ensure seamless EHR and EMR integration for virtual mental health platforms, so your notes, schedules, and patient records stay connected and organized instead of scattered.
- Smart features that save time:Tools like digital intake, triage support, and gentle reminders help keep sessions on track and reduce no-shows.
- Easy for patients to use: Simple mobile-first design means telemental health for healthcare patients works anywhere — even with slower internet — and feels comfortable from the first login.
- Light on admin work: Automated scheduling and billing cut the repetitive tasks that eat up hours and drive costs up.
- Ready to grow with you: As your services expand, the platform can scale without a rebuild, more clinicians, more features, new regions.
We work closely with practices, hospitals, and new digital-first clinics to create solutions that feel reliable and easy to use. The goal is to help you serve more people while keeping costs predictable and operations smooth. Our teams help healthcare organizations build a secure telemental health platforms tailored to their workflows and compliance needs.
If you are exploring or expanding telemental health, reach out to our team to see how we can help you build a platform that fits your patients and your business.
FAQ’s
Q. What is telemental health and how does it save costs?
A. Telemental health is just mental health care delivered at a distance via through video calls, phone check-ins, secure chats, and therapy apps. Instead of both sides spending time and money to meet in person, care happens where the patient already is.
For clinics, that shift chips away at fixed costs. Fewer rooms to rent and maintain, less furniture and waiting area space, fewer front-desk hours to manage schedules and paperwork. Therapists can stay booked without losing time on travel or long gaps between appointments. For patients, the savings feel personal: no bus rides or parking fees, no unpaid half-days off work, no juggling childcare for a short visit. Those small wins add up quietly until you notice the whole system costs less to run.
Q. How does telemental health reduce hospital readmissions and emergency visits?
A. A big reason people land in the ER during a mental health crisis is because they could not see someone soon enough. One missed appointment turns into weeks without support. Symptoms grow, things spiral, and by the time help is available, the situation is urgent.
Telemental health gives people a safety net. They can book a quick check-in or send a secure message when things feel shaky. Therapists can step in earlier, adjust care plans, or schedule extra sessions before a small slip becomes a full crisis. That early touchpoint is what keeps many from needing expensive, high-stress emergency care later.
Q. How do providers integrate telemental health into existing EMR/EHR systems?
A. It is not as tricky as it sounds, but it does require a plan. Most new platforms already speak the same “language” as EMRs and EHRs, so notes, schedules, and patient updates can flow straight into the record.
Many clinics bring in developers to fine-tune this connection, to make sure data is encrypted, HIPAA and GDPR boxes are checked, and everything feels seamless for the staff. The idea is simple: therapists keep using the system they know, but now their virtual visits show up alongside the in-person ones without extra work or risk.
Q. Can AI-driven telemental health solutions further reduce provider costs?
A. Absolutely, and not in a flashy way but in small, practical ones. AI can gather patient updates before a session, spot red flags, or help sort out who needs to be seen sooner. It can handle scheduling reminders and routine documentation that usually pulls therapists away from care.
For clinics, that means fewer admin hours, fewer no-shows, and more consistent use of therapist time. For patients, it’s easier to stick with care because reminders keep them on track and support feels more responsive. Over time, that efficiency means lower cost per visit and more stable revenue without cutting the quality of therapy.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…