- What is Interoperability in Healthcare?
- Understanding the Levels of Healthcare Interoperability
- 1. Foundational Interoperability
- 2. Structural Interoperability
- 3. Semantic Interoperability
- 4. Organizational Interoperability
- Importance of Interoperability in Healthcare
- ROI That Leadership Can Measure
- Why Decision Makers Act
- How to Achieve an Interoperable Healthcare IT Infrastructure
- Implementation Considerations Leadership Should Understand
- Budget Planning and Resource Alignment
- Engagement Models That Work for Most Hospitals
- A Future Ready Interoperability Foundation
- Examples of Interoperability in Healthcare
- 1. EHR to EHR Data Exchange: Epic Care Everywhere
- 2. FHIR Based Patient Access: Apple Health Records
- 3. Telehealth to EHR Integration: Teladoc Health
- 4. Clinical Decision Support Integration: UpToDate
- 5. Wearable to Provider Data Exchange: Fitbit Health Solutions
- Benefits of Healthcare Interoperability
- Enhanced Patient Care
- Continuity of Care
- Improved Efficiency
- Cost Savings
- Patient Empowerment
- Public Health Initiatives
- Streamlined Administrative Processes
- Better Data Analytics
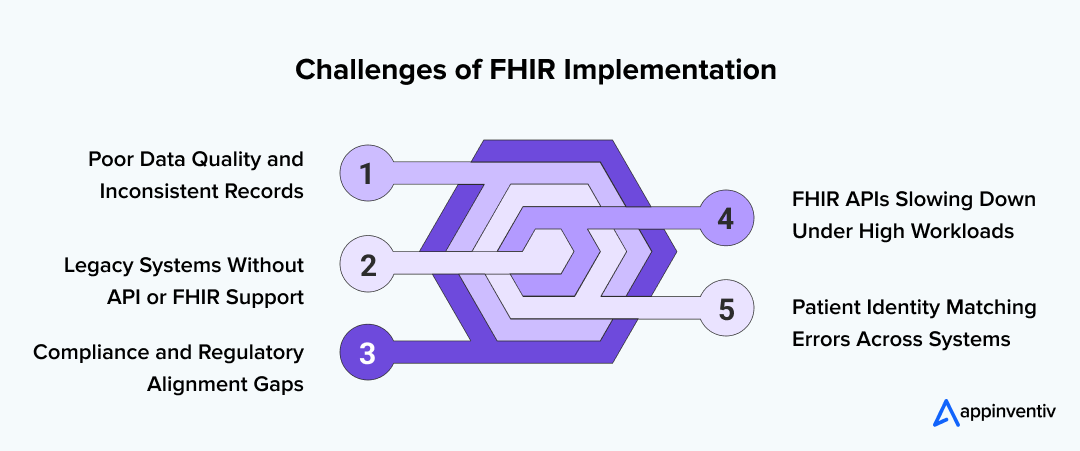
- Top 5 FHIR Implementation Challenges and Solutions
- 1. Getting Data Clean Enough for FHIR to Make Sense
- 2. Older Systems That Were Never Built for APIs
- 3. Keeping Up With Compliance While Everything Is Moving
- 4. FHIR APIs That Slow Down Under Heavy Workloads
- 5. Matching the Right Patient Across Multiple Systems
- A Practical Framework for Healthcare Interoperability Implementation (2025–2026)
- 1. Start With Clear, Practical Objectives
- 2. Assess Existing Systems and Identify What Can Be Reused
- 3. Adopt Standards That Allow Systems to Speak the Same Language
- 4. Make Privacy and Security a Core Part of the Design
- 5. Build an End-to-End Patient Journey, Not Just System Links
- 6. Prepare for Cloud, APIs, and AI as the Next Phase of Interoperability
- Cost of Implementing Interoperability for Hospitals
- Timeline and Roadmap: Interoperability Implementation Blueprint
- Months 0–3: Assessment and Interoperability Readiness
- Months 3–6: Standards Mapping and Architecture Planning
- Months 6–12: Building and Integrating Core Interoperability Capabilities
- Months 12–18: Testing, Validation, and Workflow Alignment
- Months 18–24: Optimization, Scaling, and Advanced Use Cases
- Future of Interoperability in Healthcare
- Attain Interoperability in Healthcare with Appinventiv
- FAQs
Key takeaways:
- Interoperability turns scattered health data into a single, actionable view.
- Hospitals see clear ROI through fewer repeats, faster decisions, and lower admin load.
- Interoperability maturity rises from basic data exchange to full organizational alignment.
- A phased 12–24 month roadmap makes adoption realistic and scalable.
- Appinventiv delivers proven interoperability solutions using FHIR, cloud, and modern APIs.
Healthcare is one of the most innovative sectors in terms of data development. The sector currently accounts for 30% of the entire global database stream and is expected to rise to 36% by 2025.
It is important to note that healthcare has been growing at a faster rate than other major sectors, including 6% faster than manufacturing, 10% faster than finance, and 11% faster than the media & entertainment industry. With the rising volume of this data, the importance of medical information in improving the quality of healthcare becomes obvious.
Nevertheless, it clearly presents the paradox of progress because, on average, doctors spend 18.5 million hours every year doing the most basic data collection administration stuff. This significant investment of time and energy prompts a crucial concern – the necessity of attaining interoperability in healthcare.
This article will discuss why we need to make health IT interoperability a priority, looking at the complex world of medical data and how it can simplify tasks for healthcare workers while addressing the challenges that hamper the way of attaining interoperability in healthcare.
Get a Cost Estimate for FHIR/HL7 Integration and close your interoperability gap.
What is Interoperability in Healthcare?
The ability of an electronic healthcare system to communicate seamlessly with other computers or software systems from various healthcare providers or hospitals is referred to as interoperability in healthcare. It goes beyond interconnectedness and allows the sharing and opening of health information across pharmacies, labs, clinics, hospitals, and hospices.
Healthcare providers are required to use strict data standards to protect Patient Health Information (PHI) as it is extremely sensitive. Adhering to such regulations provides a guarantee of safe data transfers across the healthcare environment.
Some key aspects of health IT interoperability include:
- Fast Healthcare Interoperability Resources (FHIR): FHIR provides a structured plan for sharing digital health data. It’s made to be changeable and used in many situations with various health information.
- Interoperability Standards: These rules explain the technical terminology and references needed for sharing healthcare information. It makes sure that systems can communicate with each other properly.
- Information Exchange Workflow: With safety and privacy in mind, interoperability solutions help to share health information. This exchange happens between different parties, like doctors, patients, and external web developers.
- Uses of Information Exchange: IT healthcare solutions that work together can assist doctors in getting the most recent science-backed medical advice. They can improve active health upkeep for their patients. Plus, these systems can make it easier to work together with other health care providers.
- Privacy and Security: Privacy and safety of health details are key to effective sharing. Interoperability needs safe sharing as it uses sensitive information. This info needs to have the utmost privacy and security.
Understanding the Levels of Healthcare Interoperability
The levels of interoperability in healthcare form a structured path that hospitals follow as they move from basic system connectivity to full scale information exchange. HIMSS groups these types of interoperability in healthcare into four stages: foundational, structural, semantic, and organizational. Each level comes with its own cost, complexity, and level of vendor support, which determines when professional consulting becomes necessary.

1. Foundational Interoperability
Foundational interoperability focuses on simple, secure data transport between systems. At this stage, systems can send and receive information, but they do not interpret the content they exchange.
What to expect:
- Lowest cost and lowest complexity
- Minimal vendor dependency
- Basic API or messaging setup
When you need external help:
Most hospitals handle the foundational level internally, especially when working with modern EHRs that already support basic exchange capabilities. External consulting is rarely required unless the organization relies heavily on outdated systems.
2. Structural Interoperability
Structural interoperability defines the format, structure, and syntax of shared data. Standards such as HL7 v2 or FHIR ensure that systems can interpret basic information consistently.
What to expect:
- Moderate complexity
- Higher reliance on EHR vendors for interface configuration
- Important for reliable data interoperability in healthcare
- Requires structured mappings for smooth workflows
Cost and vendor dependency:
Costs rise here because integration depends on how flexible the hospital’s systems are. Many EHR vendors limit how much internal teams can modify without additional licensing or support.
When you need external help:
A consulting partner becomes valuable when connecting multiple systems from different vendors or when upgrading from older HL7 messaging to FHIR based workflows.
3. Semantic Interoperability
Semantic interoperability in healthcare focuses on meaning. Systems must understand the clinical context of the data being exchanged. This ensures accurate interpretation across platforms and is essential for analytics, AI, and clinical data interoperability.
What to expect
- High complexity, especially when standardizing terminology
- Requires mapping medical vocabularies such as SNOMED CT, LOINC, and ICD 10
- Critical for safety, decision support, and precision care
Cost and vendor dependency:
This is where costs increase significantly. Semantic alignment often depends on vendor controlled structures inside the EHR, limiting in-house customization. Organizations also need strong data governance and clinical involvement.
When you need external help:
At the semantic level, a consulting partner becomes almost essential. Hospitals rely on external experts to manage terminology mapping, data quality, workflow redesign, and downstream compatibility for analytics and AI.
4. Organizational Interoperability
Organizational interoperability is the highest level, where clinical, operational, legal, and governance frameworks all work together to support seamless data exchange across institutions.
What to expect:
- The most complex and strategic stage
- Requires policy alignment, shared workflows, cross-entity trust frameworks
- Necessary for participation in TEFCA and national exchanges
- Directly influences patient access, referrals, and coordinated care
Cost and vendor dependency:
This level demands investment in governance, security, compliance, and change management. Vendor dependencies are strong here because data must flow reliably across multiple systems, networks, and partners.
When you need external help:
Professional implementation is usually mandatory. Consulting partners help design governance models, structure privacy controls, support large scale integration, and build operational workflows aligned with national and regional standards.
Importance of Interoperability in Healthcare
The importance of interoperability in healthcare is highlighted by potent numbers, indicating its significance in today’s time. An impressive 64% of all doctor visits, 70% of hospital stays, and a whopping 83% of all drug prescriptions are deeply tied to the smooth sharing and access to health information. Also, a notable 71% of total healthcare costs and a big 93% of Medicare costs are crucial parts of the healthcare use scenario.
Most clinical decisions rely on data that does not originate in the same department. When information flows smoothly, the operational and financial impact is significant. Hospitals that achieve strong healthcare data interoperability report measurable improvements such as:
- Shorter clinical decision times
- Fewer repeated tests
- Faster medication reconciliation
- Better referral turnaround
- Reduction in administrative overhead
Industry analyses show that a large share of care activity, including doctor visits, hospital stays, and prescription handling, depends on timely access to accurate patient information. Decision makers view this as not only a clinical benefit but a core performance driver.

ROI That Leadership Can Measure
Healthcare organizations that invest in interoperability often see returns through:
- Lower operational duplication
- Reduced claim denials due to complete records
- Waste reduction from repeated imaging or lab work
- Increased staffing efficiency from automated data exchange
For a hospital leadership team, these outcomes translate into improved margins, predictable workflows, and more capacity for value based care programs. These benefits of interoperability in healthcare make it a strategic investment rather than an IT upgrade.
Why Decision Makers Act
Executives commit to interoperability when they see proof points such as:
- Clear improvements in throughput and care coordination
- Reduced variability in clinical workflows
- Reliable data to support reporting and population health models
- Higher patient satisfaction linked to fewer delays
This is where the advantages of interoperability in healthcare become operational, not theoretical.
How to Achieve an Interoperable Healthcare IT Infrastructure
Moving to an interoperable IT environment requires planning, but the payoff extends across clinical, operational, and financial domains. A connected system supports better decision making, reduces manual work, and strengthens the overall digital foundation of the hospital.
Implementation Considerations Leadership Should Understand
Before committing, hospitals typically evaluate:
- How much technical debt exists inside the current system
- The age and flexibility of the EHR and departmental tools
- Which workflows depend heavily on manual processes
- Where data inconsistencies create risk or compliance issues
Leaders also consider how interoperability healthcare aligns with future digital initiatives such as AI, telehealth, and remote monitoring.
Budget Planning and Resource Alignment
Interoperability is not a one time purchase. Budget planning usually includes:
- Core integration and modernization efforts
- Middleware or API gateway setup
- Security and compliance enhancements
- Cloud hosting, if the organization moves in that direction
- Training and change management programs
This staged budgeting helps avoid cost shocks and keeps the organization aligned with long term transformation goals.
Engagement Models That Work for Most Hospitals
Most organizations adopt one of these models:
- A phased internal build supported by external consulting
- A hybrid model combining vendor tools with custom integration
- A fully managed interoperability program led by a consulting partner
The model selected often depends on internal team bandwidth, existing technical debt, and how fast leadership wants to see measurable results.
A Future Ready Interoperability Foundation
As wearables, telehealth, and remote monitoring become more common, the need for a learning health system increases. Interoperability creates the foundation for:
- Continuously improving clinical models
- Faster patient support
- Reduced care variation
- Scalable analytics and AI driven decisions
In this environment, interoperability becomes an enabler for both immediate efficiency and future innovation.
Also Read: Top Healthcare Trends that will Redefine the Industry
Examples of Interoperability in Healthcare
Interoperability comes to life when you see how real systems exchange information in ways that make care easier for both clinicians and patients. The following interoperability in healthcare examples show how hospitals, mobile platforms, and virtual care tools use shared standards and APIs to keep clinical data connected and usable across settings. Each one reflects how clinical data interoperability and data interoperability in healthcare work in practice, not just theory.
1. EHR to EHR Data Exchange: Epic Care Everywhere
Hospitals often treat patients who have been seen somewhere else, so having a complete picture matters. Epic’s Care Everywhere network helps clinicians pull allergies, medications, imaging reports, and discharge summaries from outside facilities right when they need them.
How it works in reality:
Epic relies on well established standards like C CDA for summaries and FHIR for individual data elements. Identity checks happen through national query frameworks, and terminology from other systems (SNOMED, LOINC, RxNorm) is normalized before it appears in the local record. The result is less time reconciling charts and more confidence during clinical decisions.
2. FHIR Based Patient Access: Apple Health Records
Apple Health Records gives patients something they rarely had before: a single place to view their health information from different providers. Lab results, vitals, medications, and visit summaries all appear in one timeline, making it easier for patients to stay informed and involved.
How the technology supports it:
Hospitals expose SMART on FHIR endpoints that Apple can securely connect to using OAuth. When a patient opts in, the app retrieves standardized FHIR resources such as Observation, Condition, and Encounter. Everything stays encrypted on the device, and the coding used by the hospital is preserved. Patients end up with a complete, accurate copy of their history without any extra steps from clinicians.
3. Telehealth to EHR Integration: Teladoc Health
Virtual care works best when it does not sit outside the clinical workflow. Teladoc helps solve this by sending visit notes, care summaries, and remote monitoring data directly into the hospital’s EHR. It keeps telehealth from becoming a silo and makes the experience feel connected for both sides.
What happens behind the scenes:
Visit summaries and clinical notes move through HL7 v2 messages, while biometric readings from devices are shared as FHIR Observations. Because the integration supports updates in both directions, providers can adjust care plans inside their EHR and have those changes reflected in the virtual care environment. That reduces documentation gaps and strengthens continuity of care.
4. Clinical Decision Support Integration: UpToDate
UpToDate shows how interoperability improves decisions at the point of care. When physicians review a chart, they can open guidance that’s tailored to the patient’s diagnosis, lab values, or symptoms without leaving the EHR.
How the link is created:
The EHR uses HL7 Infobutton APIs to send coded clinical terms (ICD, SNOMED, LOINC) to UpToDate. The system then returns the most relevant evidence or recommendations for that specific context. Instead of searching manually, clinicians get information that fits the moment and reduces mental load.
5. Wearable to Provider Data Exchange: Fitbit Health Solutions
Wearables help clinicians see what happens between appointments. Fitbit Health Solutions gives providers access to metrics like daily steps, heart rate, sleep patterns, and other trends, which can support chronic care and lifestyle coaching.
How the data moves:
Fitbit offers REST APIs that allow healthcare systems to pull biometric data. Providers translate these readings into FHIR Observation resources with proper timestamps and device metadata. Once in the EHR or care management platform, the data can be trended, flagged, or used to guide conversations during follow ups.
You may like reading: The Ultimate Business Guide to Healthcare Application Development
Benefits of Healthcare Interoperability
Healthcare interoperability helps everyone involved in the healthcare system. Let’s learn about some important benefits of healthcare interoperability for patients, healthcare workers, doctors, and the overall healthcare sector.
Enhanced Patient Care
Interoperability is the backbone for healthcare providers, granting them a holistic and current understanding of a patient’s medical background. This key capability empowers well-informed choices, diminishes potential medical mistakes, and enriches the overall quality of patient care.
Continuity of Care
Many patients require treatment from different healthcare professionals across other locations. Interoperability plays a crucial role in facilitating the smooth flow of health information, thus guaranteeing consistent care delivery and averting any disruptions in treatment.
Improved Efficiency
Making data sharing smoother between various health systems reduces typing work, paperwork, and repeat tests. This effective approach not only saves time but also lessens the chance of mistakes linked to manual tasks.
Cost Savings
The cost benefits of healthcare interoperability include eliminating repetitive and rule-based tasks, lessening mistakes, and boosting the smooth run of things. It makes the best use of resources and aids in managing healthcare spending.
Patient Empowerment
Empowering patients through interoperability grants them expanded access to their health information, fostering transparency and active engagement in healthcare choices. This approach further promotes adherence to treatment plans and empowers individuals to assume control over their well-being.
Public Health Initiatives
Interoperability plays a crucial role in advancing public health initiatives. It facilitates the prompt exchange of data concerning disease outbreaks, health trend monitoring, and the implementation of preventive measures – all working towards enhancing population health management.
Streamlined Administrative Processes
Automating administrative tasks in health contributes to a reduction in the workload for medical professionals. This involves streamlining billing processes, managing insurance claims, and executing other administrative functions, ultimately enhancing the efficiency of workflow.
Better Data Analytics
Health data interoperability enables in-depth data analytics, offering valuable perspectives into public health, treatment efficacy, and patterns within the healthcare landscape. This method, rooted in data, facilitates informed decision-making and long-term strategizing.
Top 5 FHIR Implementation Challenges and Solutions
FHIR has become the common language everyone in healthcare wants to speak, but getting there is rarely simple. Hospitals and health systems usually discover the gaps only when they begin connecting their EHRs, labs, imaging systems, and patient apps. Below are five real challenges teams face during FHIR adoption and some grounded ways to work through them.
1. Getting Data Clean Enough for FHIR to Make Sense
Most hospitals work with old records, missing fields, different naming conventions, and notes that were never meant to move across systems. When this information enters a FHIR pipeline, it becomes difficult for any system to read or trust it. Ensuring the effective governance and quality assurance of healthcare data is essential for achieving seamless interoperability.
How teams fix it in practice
- Run basic data profiling to see what is actually usable
- Standardize medical terms through SNOMED CT, LOINC, and ICD 10
- Add validation checks before data enters the exchange layer
- Create a shared dictionary so every department uses the same structure
Once the foundation is clean, FHIR implementation becomes far more predictable.
2. Older Systems That Were Never Built for APIs
Many providers still rely on systems that were designed long before APIs and FHIR existed. These platforms struggle with modern formats and cannot exchange information without extra help. This is one of the most visible interoperability challenges in healthcare because it shows up early and affects the entire workflow.
What usually works
- Put a lightweight FHIR gateway in front of legacy systems
- Use middleware that can translate HL7 v2 messages into FHIR resources
- Move critical components to cloud services gradually
- Revisit vendor contracts during upgrades and push for FHIR support
These steps allow organizations to adopt FHIR without replacing every system at once.
3. Keeping Up With Compliance While Everything Is Moving
Every FHIR project must stay aligned with HIPAA, GDPR, TEFCA, and local data sharing rules. Even small design choices, such as how a resource is stored or who can view it, can affect compliance. This adds pressure on IT teams and slows down implementation unless the guardrails are defined early.
A practical approach
- Use a privacy-first design so sensitive data never moves without protection
- Set clear access rules and track every interaction
- Implement consent management for patient controlled data
- Review all workflows against healthcare interoperability standards such as TEFCA
When compliance is built in from the start, the project moves faster and avoids rework.
4. FHIR APIs That Slow Down Under Heavy Workloads
Once a hospital begins exchanging large volumes of clinical records, images, and real time feeds, FHIR services can slow down. This is less about the standard and more about how the system is architected. Performance issues often surface only when the first large-scale integration goes live.
How teams keep systems steady
- Cache frequently accessed resources
- Use asynchronous patterns for heavy data transfers
- Shift complex tasks to cloud environments that can scale
- Track response times, failures, and throughput through monitoring tools
These adjustments allow FHIR based workflows to stay reliable even during peak load.
5. Matching the Right Patient Across Multiple Systems
One of the toughest barriers to interoperability in healthcare is patient identity. Records from different places often contain spelling variations, incomplete fields, or mismatched dates. When systems cannot confirm who the patient is, the rest of the interoperability effort falls apart.
How organizations solve this
- Deploy an EMPI to keep one source of truth
- Use probabilistic and AI assisted matching models
- Standardize demographic fields across all touchpoints
- Document clear identity rules for every department
Accurate identity matching is what makes shared records trustworthy and safe.
A Practical Framework for Healthcare Interoperability Implementation (2025–2026)
Healthcare organizations are moving fast toward connected systems, yet the path to interoperability in healthcare technology is rarely straightforward. The steps below reflect how hospitals and care networks are approaching interoperability in 2025–2026, blending strategy, modern tools, and patient centric workflows.
1. Start With Clear, Practical Objectives
Teams begin by deciding what they want connected and why. Without this clarity, even the most advanced systems fail to deliver meaningful outcomes. Setting a direction helps avoid unnecessary complexity and keeps the project aligned with long term goals.
Organizations usually define:
- Which systems or departments need first level integration
- The desired maturity level for interoperability in healthcare information systems
- Workforce capacity and vendor dependencies
- Expected clinical and operational improvements
- Compliance needs tied to HIPAA, TEFCA, and local data policies
Emphasizing compliance with healthcare regulations, particularly those related to safeguarding patient data such as HIPAA, is essential in goal-setting to uphold the confidentiality of exchanged information.
2. Assess Existing Systems and Identify What Can Be Reused
Many hospitals already have partial integrations in place. The challenge is understanding where interoperability healthcare already exists and where gaps remain.
A typical assessment includes:
- Reviewing EHR API capabilities
- Studying current HIE participation
- Mapping data movement across departments
- Identifying manual processes that need digitization
- Listing legacy tools that require upgrades or middleware
This review becomes a roadmap for extending healthcare data interoperability without replacing entire systems.
3. Adopt Standards That Allow Systems to Speak the Same Language
Interoperability depends on consistent data structures. In 2025–2026, most organizations deepen their use of standards that allow information to move smoothly across platforms.
Common standards include:
- FHIR for flexible API based exchange
- HL7 for structured messages
- ICD 10, SNOMED CT, and LOINC for terminology
- Resource mapping frameworks for analytics and AI
These standards strengthen data interoperability in healthcare, allowing systems to interpret and act on shared information reliably.
4. Make Privacy and Security a Core Part of the Design
As more systems connect, security becomes central to every design decision. Healthcare organizations no longer treat compliance as an afterthought. Instead, they integrate privacy early in the architecture.
Teams focus on:
- Encrypted exchange across all APIs
- Role based access controls
- Consent and authorization workflows
- Staff training for safe handling of PHI
- Continuous audit trails for every data interaction
A security first design ensures that interoperability scales safely.
5. Build an End-to-End Patient Journey, Not Just System Links
Interoperability is not only a technical requirement. It directly impacts how patients experience care. When systems work together, clinicians and patients both benefit from smoother, faster, and more informed workflows.
Healthcare organizations map the patient journey and focus on:
- Integrating CRM, EHR, telehealth, and scheduling
- Reducing handoff delays between departments
- Automating referrals and care transitions
- Keeping patient portals updated in real time
When information flows effortlessly, patients spend less time repeating their history and more time receiving care.
6. Prepare for Cloud, APIs, and AI as the Next Phase of Interoperability
The future of interoperability sits in cloud environments and API driven data exchange. Cloud platforms support scalable FHIR servers, real time analytics, and IoT integrations that older systems cannot handle.
Organizations preparing for the next phase focus on:
- Migrating systems to cloud hosted environments
- Setting up modern API gateways
- Adding observability tools to track API health
- Integrating remote monitoring and wearable device data
- Cleaning and structuring data for AI assisted clinical workflows
These capabilities will define how ready healthcare organizations are for the next generation of interoperability in healthcare technology.
Cost of Implementing Interoperability for Hospitals
The cost of bringing true interoperability healthcare capabilities into a hospital can vary a lot. Most organizations end up somewhere between $40,000 to $400,000, depending on how many systems need to talk to each other and how old those systems are. Some start small with a few clinical connections. Others take on a full modernization effort. Below mentioned are some of the cost drivers:
- Connecting the Core Systems: Linking the EHR with labs, radiology, billing, and care teams makes up the first big part of the spend. Older systems often need extra work before they can share data reliably, especially when building toward stable data interoperability in healthcare.
- Middleware and API Setup: Most hospitals introduce a middleware or FHIR layer to help older platforms communicate with new ones. This becomes the engine that moves data and keeps everything in sync.
- Security and Compliance Work: Every connection needs to meet HIPAA, TEFCA, and internal privacy requirements. Encryption, access rules, audits, and testing all add to the total investment but are essential for patient safety.
- Cloud and Infrastructure: More hospitals now choose cloud based setups to support interoperability. Cloud services make it easier to scale APIs and handle peak workloads, which is why cloud interoperability in healthcare has become a common part of the cost.
- Training and Workflow Adjustments: Clinicians and staff need time to learn the new flow of information. Updating processes, documentation, and tools adds a smaller but important portion of the budget.
Timeline and Roadmap: Interoperability Implementation Blueprint
Interoperability is not a single project. It is a phased transformation that touches workflows, infrastructure, compliance, and patient experience. Most healthcare organizations succeed when they adopt a structured roadmap instead of trying to modernize everything at once. The blueprint below reflects a realistic 12–24 month timeline many hospitals follow when improving interoperability in healthcare information systems.
Months 0–3: Assessment and Interoperability Readiness
The first phase focuses on understanding where the organization stands today and what will be required to move forward.
Key activities include:
- Mapping existing systems, interfaces, and vendor dependencies
- Reviewing how interoperability healthcare capabilities currently function
- Identifying gaps in data interoperability in healthcare workflows
- Evaluating compliance needs tied to HIPAA, TEFCA, and regional mandates
- Documenting architectural limitations in legacy EHR components
This stage creates the visibility necessary to design a grounded plan.
Months 3–6: Standards Mapping and Architecture Planning
Once the baseline is clear, teams decide how data will flow and how different systems should communicate.
This involves:
- Finalizing the healthcare interoperability standards to be used across departments
- Designing the target architecture, including FHIR servers and API gateways
- Creating a terminology alignment plan using ICD 10, SNOMED CT, and LOINC
- Planning integrations required for clinical data interoperability
- Identifying workflows that can be automated once data exchange stabilizes
By the end of this phase, the organization has a clear technical blueprint for moving ahead.
Months 6–12: Building and Integrating Core Interoperability Capabilities
With planning complete, implementation begins. This period is typically the most resource intensive as teams connect systems, introduce new APIs, and modernize old interfaces.
Key milestones include:
- Deploying or upgrading the EHR’s FHIR capabilities
- Introducing middleware to link legacy systems with modern interfaces
- Implementing role based access and encryption policies
- Digitizing manual workflows that block interoperability
- Setting up observability dashboards for message failures and exchange volume
This is when the first major data flows become visible across departments.
Months 12–18: Testing, Validation, and Workflow Alignment
Interoperability becomes valuable only when data is accurate, complete, and usable in real clinical settings. This stage focuses on reliability and consistency.
Organizations typically:
- Validate FHIR resource mapping and cross system data accuracy
- Test real world care scenarios such as referrals, discharges, and lab updates
- Refine workflows that depend on clinical data interoperability
- Confirm compliance readiness for audits and TEFCA participation
- Train clinical and operational teams to use integrated tools
By the end of this period, data movement stabilizes, and clinicians begin to experience meaningful workflow improvements.
Months 18–24: Optimization, Scaling, and Advanced Use Cases
Once core interoperability is functioning, organizations shift to enhancing performance and exploring advanced use cases.
Common initiatives include:
- Expanding interoperability across more departments or partner networks
- Integrating telehealth, wearables, and IoT data streams
- Automating transitions of care and population health reporting
- Enabling analytics and AI tools that rely on structured, high quality data
- Preparing the infrastructure for future scalability and national exchange frameworks
This phase positions the organization for long term growth and innovation.
Future of Interoperability in Healthcare
The future of interoperability in healthcare looks promising with the implementation of emerging technologies and enhanced interoperability standards like FHIR, promoting seamless data exchange.
For instance, blockchain is designed to address security concerns, ensuring trustworthy data sharing. APIs in healthcare will play a crucial role in enabling secure and efficient communication between disparate systems, thereby facilitating real-time data access and supporting a patient-centered approach to personalized care. Improved APIs will foster efficient communication, enabling a patient-centered approach to personalized care. The integration of AI and ML in healthcare promises informed decision-making and personalized treatment plans. The growth of the IoT in healthcare expands data interoperability, incorporating wearables and remote monitoring.
Government regulations emphasize standardized data exchange and global health information sharing. Currently, healthcare initiatives are focused on integrating telehealth and virtual care, prioritizing interoperability between digital platforms and conventional systems. Cybersecurity is essential in safeguarding patient information during exchanges.
The future of healthcare interoperability envisions a more connected, intelligent, and secure landscape, prioritizing improved patient experiences and outcomes.
Attain Interoperability in Healthcare with Appinventiv
Interoperability in healthcare IT is essential since it improves patients’ outcomes, service delivery, and financial health. Consequently, healthcare institutions should consider the challenges that may arise and take other regulatory endeavors to establish a more interoperable health information system that effectively delivers improved care outcomes.
When looking for the best healthcare IT consulting services to attain interoperability, you can consider partnering with Appinventiv. We have a proven track of building advanced healthcare applications for businesses worldwide.
Our portfolio demonstrates effective solutions for medical businesses, including YouCOMM, which increased the nurses’ response time by up to 60% over 5+ hospital chains in the US and helped us become a trusted custom healthcare software development company around the world.
Furthermore, millions of people have embraced Soniphi, an e-health app that records user’s voices for complete health analysis, demonstrating the significance of our innovative approaches in software development.
Interested in building similar solutions and advancing your health IT interoperability journey? Connect with our experts now and see your business reach greater heights.
FAQs
Q. What is interoperability in healthcare?
A. Interoperability in healthcare refers to the ability of different systems, applications, and devices to exchange and use patient information without manual intervention. When data moves smoothly across clinical, operational, and administrative systems, providers can coordinate care more effectively. Modern interoperability in healthcare technology relies on standards like FHIR, HL7, and C CDA to keep information consistent and usable across platforms.
Q. How do you define interoperability in healthcare?
A. Interoperability in healthcare refers to the ability of digital health systems to exchange data and interpret it consistently across platforms.
It goes beyond basic data sharing and focuses on:
- Ensuring clinical meaning is preserved when information moves between systems
- Allowing EHRs, labs, pharmacies, and care platforms to understand data in the same context
- Supporting accurate clinical decision making using shared patient records
When interoperability works correctly, healthcare organizations operate from a unified, trustworthy source of information rather than fragmented systems.
Q. What are the problems with interoperability in healthcare?
A. Interoperability in healthcare faces several structural and technical challenges that slow down data exchange and limit clinical efficiency.
The most common issues include:
- Incompatible EHR systems that cannot communicate reliably
- Inconsistent data formats across departments and vendors
- Technical debt within legacy healthcare IT environments
- Lack of shared clinical terminology and coding standards
- Limited or poorly implemented API support
When there is a lack of interoperability in healthcare, patient records become fragmented, tests are repeated unnecessarily, and administrative workloads increase. Healthcare organizations are addressing these gaps through interoperability solutions in healthcare, including FHIR based data models, cloud integration, and standardized terminology mapping to improve data consistency and system alignment.
Q. How does interoperability impact healthcare delivery?
A. Interoperability directly affects the quality and speed of patient care. When systems align, clinicians gain instant access to reliable information, which improves diagnosis, reduces avoidable errors, and speeds up care transitions. Strong cloud for interoperability in healthcare models allow real time sharing of labs, imaging results, and care summaries, which leads to fewer delays and more coordinated treatment. Ultimately, interoperability supports better patient outcomes and smoother workflows across the entire care team.
Q. How can healthcare organizations improve interoperability?
A. Improving interoperability requires both technology upgrades and workflow alignment. Hospitals generally focus on adopting standards like FHIR, modernizing APIs, cleansing legacy data, and integrating cloud environments. Many organizations partner with teams specializing in healthcare interoperability software development to build secure interfaces and automate data exchange. Cloud platforms also simplify integration efforts and support scalable interoperability solutions in healthcare. Success often depends on creating a roadmap that aligns technology, compliance, and clinical needs.
Q. What are some use cases of interoperability in the healthcare industry?
A. Real world use cases of interoperability in healthcare industry settings include:
- EHR to EHR record exchange during referrals
- Telehealth platforms sending visit summaries to hospital systems
- Wearables streaming vitals into remote monitoring dashboards
- Pharmacy systems checking medication histories through shared networks
- Care teams coordinating transitions after discharge
These examples highlight how integrated data flows help reduce duplication, support preventive care, and create a more connected patient journey.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…

How To Build A Custom Behavioral Health Software? Costs, Features & Compliances
Key Takeaways Custom behavioral health software development supports the unique needs of therapy work that many general EHR tools do not cover well. Start with the foundational modules. Clinical notes, scheduling, billing, and security should be the first modules you build. Treatment plans and consent controls are important for safe and organized care, so they…

How Custom Healthcare App Development is Powering Digital-First NHS Care
Key Highlights: NHS teams are moving fast toward digital-first care, and custom apps are filling gaps that the standard NHS App cannot cover. Custom healthcare apps help reduce workload, cut waiting times, and improve how patients access care across Trusts and ICS regions. UK rules such as DTAC, NHS DSP Toolkit, NHS Login, and UK…