- Understanding Healthcare Payer Analytics
- Types of Analytics Used in Healthcare Payer Systems
- Claims Analytics
- Risk Adjustment Analytics
- Risk Modeling Analytics
- Financial Analytics
- Quality and Outcomes Analytics
- Utilization Analytics
- Health Equity Analytics
- Steps to Establish a Successful Healthcare Payer Analytics Strategy
- Figure Out Your Objectives
- Build One Single Data Foundation
- Pick the Right Tools and Technologies
- Track the Important Things (KPIs)
- Develop Smart Prediction Models
- Focus on Compliance and Security
- Get Teams Talking
- Make Improvement a Habit
- Key Applications and Use Cases of Healthcare Payer Analytics
- Identifying Fraud, Waste, and Abuse
- Managing Claims and Costs
- Keeping Members Engaged
- Population Health and Risk
- Supporting Value-Based Care
- Compliance and Reporting
- Provider Network Optimization
- Revenue and Payment Integrity
- Predictive Utilization Management
- Challenges of Adopting Healthcare Data Analytics for Payers And How to Overcome Those
- Data Silos and Fragmentation
- Quality and Standardization of Data
- Privacy and Compliance Risks
- Intrinsic Infrastructure and Scalability Problems
- Poor Analytical Ability and Cultural Obstacles
- Interpretation of Insights into Action
- Future of Healthcare Payer Analytics: What Does It Beholds?
- Generative AI
- Cloud-Based Analytics Platforms
- Real-Time Data Streaming
- Visualization and Self-Service Analytics
- How Appinventiv Can Help Build a Custom Healthcare Payer Analytics Solution
- FAQs
Key Takeaways
- Healthcare payer analytics converts raw claims data into actionable insights that support smarter financial decisions and interventions.
- High-level analytics enable the payers to lower expenses, enhance the outcomes of their members, and increase operational efficiencies by uncovering trends, threats, and opportunities.
- The key to breaking the data silos, compliance, and maximization of ROI is in the implementation of a single database and the appropriate analytics tool.
- Proactive analytics use will enable payers to anticipate high-cost cases and avoid fraud, and value-based care initiatives to be successful in the long term
Healthcare payers hold mountains of data, including claims, clinical notes, lab results, and pharmacy records. Yet, a large portion of this remains untapped and underutilized. Within these vast stores of data lie powerful insights. These could genuinely transform the quality of care, member engagement, and financial performance.
The potential is substantial: McKinsey notes that for every $10 billion in payer revenue, AI solutions alone might save between $150 million and $300 million in administrative costs. They could also reduce medical expenses by nearly $1 billion ($970 million) and boost revenues by as much as $1.24 billion.
Turning claims data into actionable intelligence is no longer merely a technical objective; it is a clear competitive necessity. As healthcare costs rise and financial margins tighten, payers must learn to translate raw data into meaningful, real-time intelligence.
This intelligence must drive better outcomes for both the organizations themselves and their members. This is precisely where healthcare payer analytics becomes essential. It transforms fragmented information into insights that power smarter financial decisions, targeted interventions, and more efficient operations. When applied correctly, healthcare payer analytics clearly expose inefficiencies, accurately predict risk, and strengthen necessary provider partnerships.
This blog explores how healthcare payer analytics functions, its primary applications, major components, effective implementation strategies, common challenges, and the measurable return on investment that comes from finally unlocking the true value hidden within claims data.
Let’s delve deeper.
Turn this advantage into growth with automation that simplifies claims, payments, and provider operations
Understanding Healthcare Payer Analytics
Healthcare analytics for payers refers to the application of more sophisticated data-driven techniques to assist the insurance companies and other related organizations in making smarter, evidence-based decisions. Simply put, healthcare payer analytics focuses on analyzing claims, costs, and member behavioral patterns.
Compared with general healthcare data analytics, which focuses on clinical outcomes and patient care, payer analytics focuses on financial efficiency, risk management, and operational improvement.
The primary objective is to assist payers in improving cost-efficiency, increasing member satisfaction, and preventing fraud or billing errors. Through healthcare data analytics for payers analyze utilization rates, claims history, and population health data, enabling them to optimize plan design, negotiate provider contracts, and identify anomalies before they occur.
This model also contributes to the overall movement towards value-based care by measuring the performance outcomes and rewarding quality rather than quantity, and matching reimbursement systems with the actual health-related outcomes. Furthermore, it will enhance regulatory compliance through establishing data transparency, proper claim processing, and compliance with the emerging reporting standards.
Types of Analytics Used in Healthcare Payer Systems
There are several data analytics approaches used by payers to inform their strategic and operational decisions. They are commonly included in health plan data analytics, where these methods aim to transform vast claims and member data into valuable insights that improve care quality and reduce expenditures.
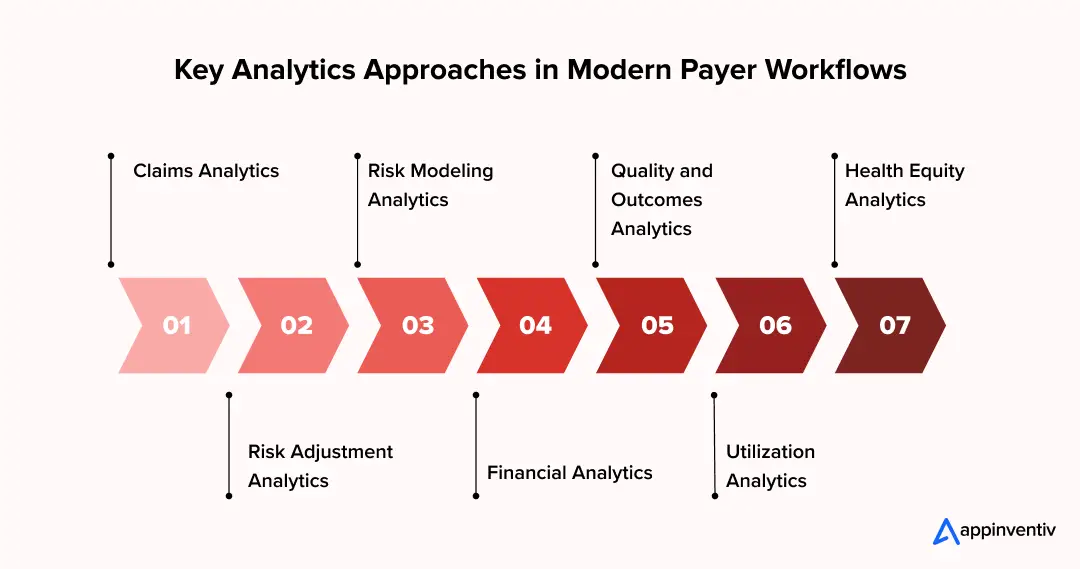
Claims Analytics
This is what healthcare payer analytics is based on. It is about an examination of the entire claims lifecycle, including submission and adjudication to settlement and reporting. Descriptive models are used to detect recurring patterns or anomalies in claims, whereas predictive models are used to predict claim volumes and potential denials, enabling faster interventions.
Risk Adjustment Analytics
Risk adjustment analytics are tools applied by payers to assess the health risks of members’ populations and provide fair reimbursements. Diagnostic analytics is used to explain differences in risk scores, while predictive tools forecast future risk levels based on demographics and prior clinical history.
Risk Modeling Analytics
Predictive analytics helps identify high-cost patients, chronic conditions, and potential care gaps early. Prescriptive models take an even further step and make specific recommendations on the specific intervention or disease management programs to avoid excessive increase in costs.
Financial Analytics
This type is aimed at monitoring the revenue leakage, cost trends, and payment accuracy. Historical spending is summarized by descriptive analytics, whereas diagnostic and prescriptive analytical tools can be used to identify and address inefficiencies in the payer operations.
Quality and Outcomes Analytics
These analytics evaluate the level of performance of providers, the quality of care, and patient outcomes. Healthcare predictive analytics identify members who are likely to have poor outcomes, and prescriptive analytics help to organize care and plan incentives to achieve better results.
Utilization Analytics
Utilization analytics is the study of the utilization of healthcare services among populations. Diagnostic analytics describes how it is over/underutilized, and predictive techniques predict demand in order to manage networks and resources optimally.
Health Equity Analytics
This increasing region measures access disparities, outcome disparities, and resource allocation disparities. The descriptive and diagnostic analytics can be used to see the trends of inequity, and the prescriptive tools can be used to design specific outreach or benefit strategies to bridge those gaps.
Collectively, these analytics can help the payers switch to proactive plans to enhance efficiency, compliance, and satisfaction among members by making the evaluation retrospective.
Appinventiv’s Insights
The strength of healthcare payer analytics lies in how these types work together rather than in isolation. Claims, risk, financial, and quality analytics, when combined, form a feedback loop, with each insight improving the next. This interrelated system transforms stagnant data into a living system of intelligence that enables smarter, faster payer decisions.
Steps to Establish a Successful Healthcare Payer Analytics Strategy
Creating a working analytics strategy that scales is what the modern healthcare payers need. Modern healthcare payer analytics software solutions play a key role here as the payers actually put huge amounts of healthcare data together, understand it, and then do something with it. Let’s check out the steps to establish a clear strategy plan:
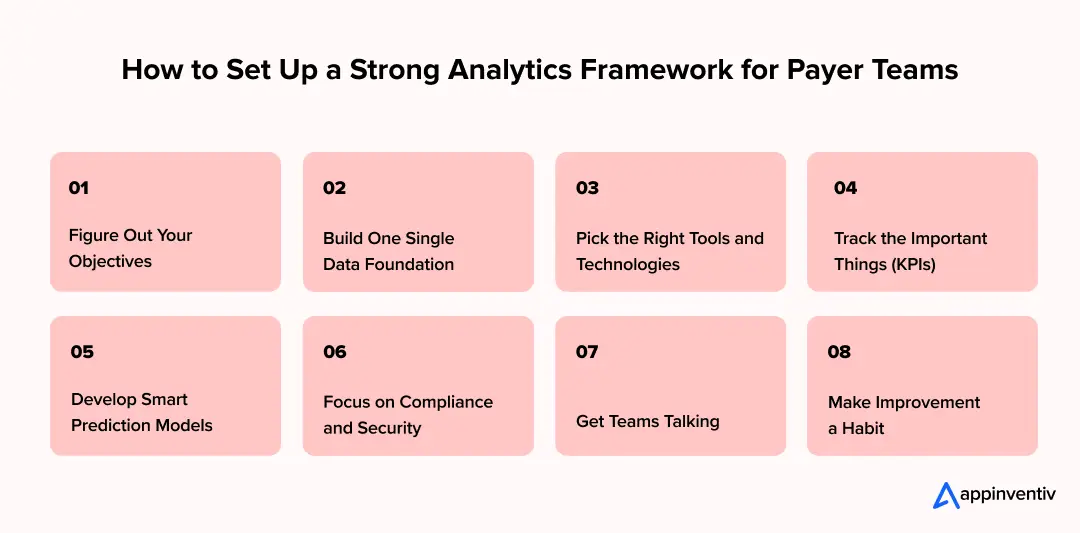
Figure Out Your Objectives
Start by asking: What is the business trying to fix? Analytics should help those core goals. Maybe you need to cut how much it costs to run the back office, catch fraud faster, process claims more accurately, or get members more involved.
You might just want to focus on value-based care, too. If you set clear priorities now, your analytical work will naturally line up with the measurable results your organization needs.
Build One Single Data Foundation
You have to pull information from everything that includes claims, provider rosters, member details, and clinical notes, putting all into a centralized repository. A unified data model is the only way to support real health plan data analytics and get insights that cut across different teams.
You also need to standardize the data, check its quality often, and set up proper governance. That’s essential for keeping everything consistent and accurate.
Pick the Right Tools and Technologies
Invest in platforms that can truly handle big data, strong visualization software, and machine learning frameworks. Make sure they can manage huge data volumes safely.
When you bring AI in healthcare payer analytics, it’s a huge boost. It helps spot patterns, catches fraud automatically, and makes predictive analysis much more reliable.
Also Read: AI Agents in Fraud Detection
Track the Important Things (KPIs)
Define metrics that matter. These should cover both how the operations are running and how members are doing. Typical examples include how quickly claims are paid, the medical cost ratio, how well providers perform, and member satisfaction scores.
Tracking these metrics allows payers to evaluate progress and pinpoint inefficiencies using insights from healthcare payer analytics.
Develop Smart Prediction Models
Use predictive analytics to anticipate high-cost patient cases, disease risk, and potential fraud, and then connect this to prescriptive analytics. That means the system tells you exactly what to do: recommend specific interventions, organize resources in the most efficient way, and design personalized care plans that fit the company’s goals.
Focus on Compliance and Security
You must follow all regulatory frameworks like HIPAA and other data protection laws in your region. Secure data storage, limited and controlled access, and constant monitoring aren’t just good practice, they’re necessary to protect sensitive member and provider information.
Get Teams Talking
Data scientists need to work with IT people, clinicians, and the business stakeholders. This collaboration is vital. It’s what ensures the data insights actually turn into practical, real-world action. It improves outcomes everywhere and helps build a truly data-driven workplace.
Make Improvement a Habit
Check your analytical models regularly. When new data comes in, update them. Encourage the teams to keep refining their dashboards, test out new data sources, and adopt the best practices they find. This is how you sustain long-term value and keep operations strong.
Key Applications and Use Cases of Healthcare Payer Analytics
Healthcare payer analytics is a must-have tool for insurers and payers today. It’s how they keep their finances healthy, get better results for their members, and make sure they’re following all the rules. Here are some of the top healthcare payer analytics use cases with real-life applications:
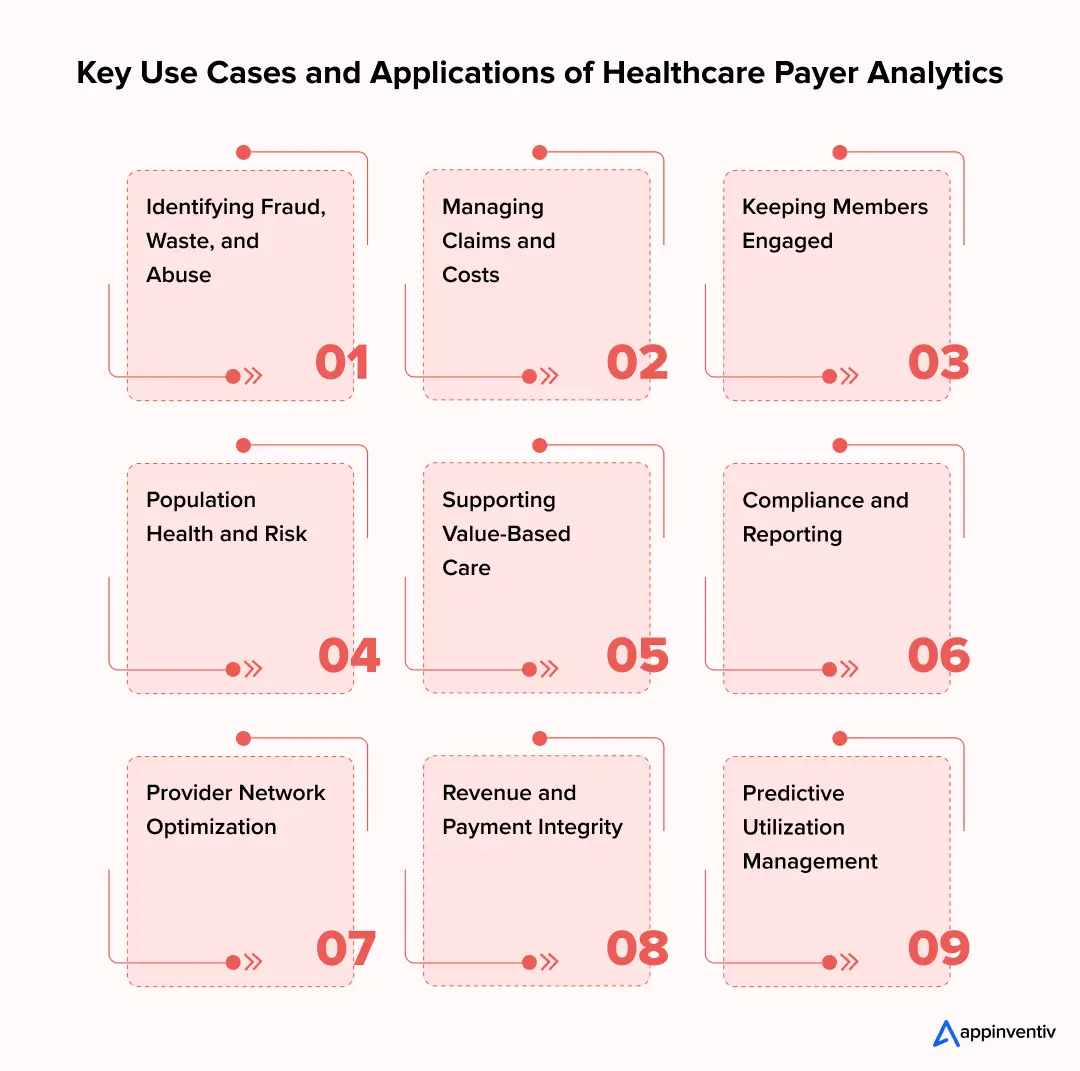
Identifying Fraud, Waste, and Abuse
Analysts rely on advanced analytical models. These models find issues right away: weird billing issues, claims submitted twice, or other suspicious provider activity. Predictive algorithms and anomaly detection tools are key. They make internal checks much stronger, reducing the money lost to fraudulent activity.
To illustrate, AI-based analytics are used by Anthem (now Elevance Health) to track claims in real time, eliminating hundreds of millions of potential overpayments each year.
Managing Claims and Costs
Payers use analytics to smooth out the entire claims adjudication process. The system helps cut down on human errors and clearly shows where the costs are coming from. Through healthcare payer analytics, teams can track healthcare claims trends in real-time. This is powerful intelligence, letting insurers negotiate better contracts with providers and manage their finances more efficiently.
Cigna applies predictive analytics to maximize each reimbursement and target reimbursement cost outliers to enhance total claims efficiency and turnaround speed.
Keeping Members Engaged
Healthcare analytics data for payers helps segment members into groups. Segmentation is done by looking at health behavior, demographics, and risk levels. This is vital. It means the payer can create customized outreach programs, manage care proactively, and raise overall member satisfaction scores.
Humana’s data-driven engagement programs use behavioral and demographic segmentation and preventive care reminders to increase member engagement rates by more than 25 times.
Population Health and Risk
By combining predictive models with AI in healthcare payer analytics, payers can spot high-risk populations much earlier. This matters because it ensures resources are disbursed at the right place where they will benefit the most. Finding these risk levels helps tremendously with preventive care initiatives; fewer people end up in the hospital needlessly.
Blue Cross Blue Shield of Massachusetts uses risk stratification tools to detect members with chronic conditions at an early stage and enhance the outcomes of preventive care.
Supporting Value-Based Care
Analytics gives payers the information they need to gauge provider performance. It tracks quality metrics, ensuring payments align with actual, measurable health outcomes. Using health plan data analytics, organizations can build stronger partnerships with their providers. The goal is simple: hold everyone in the care network accountable.
UnitedHealthcare applies state-of-the-art analytics to consider provider efficiency and match reimbursement models to outcome-based measurements.
Compliance and Reporting
Automated dashboards simplify those incredibly complicated reporting requirements. They ensure everything submitted for compliance is accurate and keep financial and operational data streams transparent for everyone who needs to see them.
Aetna uses analytics to automate CMS and NCQA reporting to enhance accuracy and minimize time spent on audit preparation.
Provider Network Optimization
Analytics assists payers in assessing network performance and identifying service gaps. It reveals which providers are delivering better results and need new collaboration. Payers can ensure more effective contracting by monitoring network leakage and patient referral patterns.
Blue Shield of California applies network analytics in tracking the performance of providers and redesigning networks to improve the balance between costs and quality.
Revenue and Payment Integrity
Analytical tools are used to track the reimbursement trends, identify underpayment, and limit leakages in financial operations. Live analytics ensure that claims are paid correctly and that revenue remains consistent across regions or programs.
The Centene Corporation applies payment integrity analytics to its claims system and recovers millions of dollars annually through proactive audits.
Predictive Utilization Management
Payers will be able to predict high-cost events such as ER visits or hospital readmissions in advance. With the help of predictive analytics, earlier intervention can be offered via care management programs or telehealth outreach.
Highmark Health’s predictive models identify utilization spikes and direct members to less expensive care alternatives.
Use the power of data to cut costs, elevate care quality, and drive the future of payer innovation
Challenges of Adopting Healthcare Data Analytics for Payers And How to Overcome Those
Although the information obtained through healthcare data analytics is valuable, the journey towards complete analytical maturity and adoption is complex and laden with challenges. Here are some of the major adoption challenges of healthcare data analytics for payers and solutions to handle those:
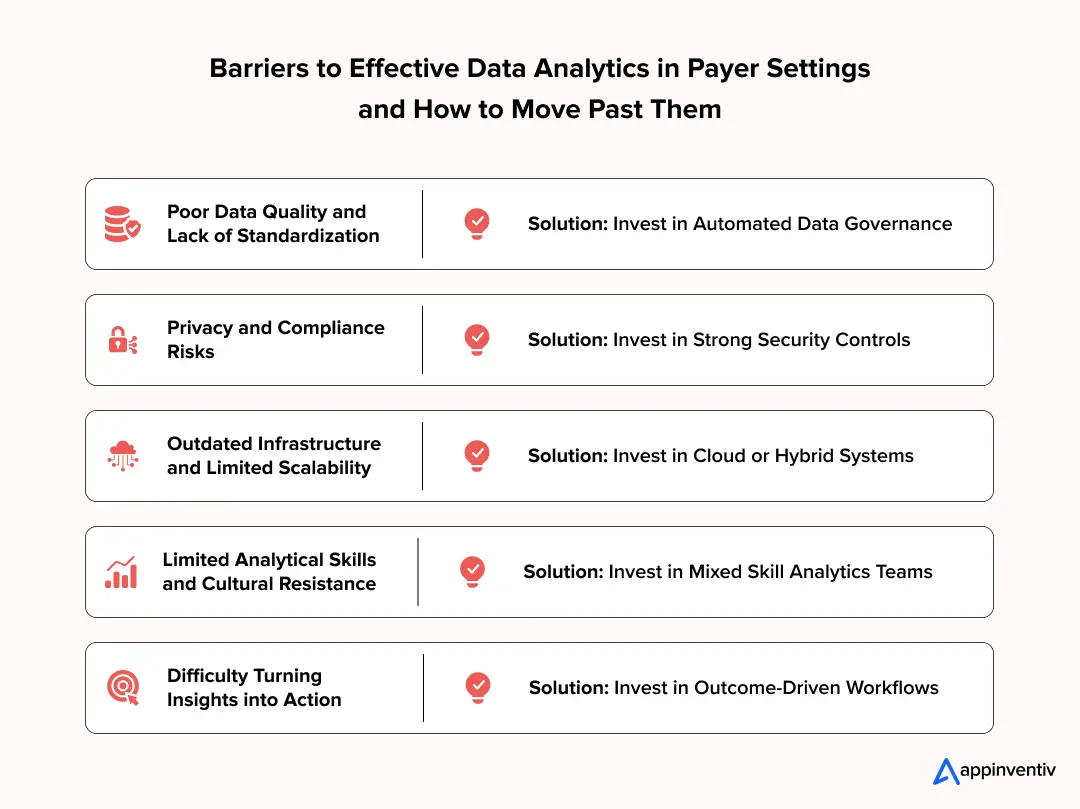
Data Silos and Fragmentation
Healthcare data is typically stored in various systems, including claims databases, EHRs, pharmacy portals, and third-party vendors. This resistance to integration compromises the accuracy of analytics and slows down the generation of insights.
Solution: Invest in unified data platforms or modern data lakes that consolidate claims, clinical, as well as demographic data. Standards of interoperability, such as HL7 integration, ensure that information exchange is clean and more uniform.
Quality and Standardization of Data
Unfinished, duplicate, or inconsistent information results in poor reporting and untrustworthy risk models. Even the slightest discrepancy in the records of the provider and payer may influence reimbursement.
Solution: Have a centralized data governance model that automates data cleaning and validation to have standardized inputs in all analytics processes.
Privacy and Compliance Risks
The necessity of working with the protected health information (PHI) subjects, payers, to the HIPAA and other requirements. Violations or failure to comply may lead to the imposition of fines and loss of confidence.
Solution: Ensure strong encryption, role-based access, and constant monitoring. Frequent adherence to compliance checks and employee education helps in compliance with privacy legislation.
Intrinsic Infrastructure and Scalability Problems
Many payers continue to rely on outdated systems that cannot handle heavy analytical loads. Such old platforms limit real-time processing and predictive modeling.
Solution: Migrate to cloud or hybrid systems at a slow pace. Platforms designed for Healthcare Analytics for Payers, such as Azure for Healthcare or AWS HealthLake, support scaling and easy data integration.
Poor Analytical Ability and Cultural Obstacles
The new analytics would demand not only technology but individuals capable of analysing multifaceted data. A significant number of payer teams are unwilling to use predictive algorithms or machine learning outputs.
Solution: Develop multidisciplinary analytics groups that include actuarial, clinical, and technical specialists. Encourage data literacy in different departments to allow employees to interpret and use findings appropriately.
Interpretation of Insights into Action
Analytics tend to end at reporting rather than at guiding actual change. Insights cannot work without clear execution plans because they do not enhance results or efficiency.
Solution: Align the analytics results with quantifiable business outcomes, such as improved member engagement or reduced costs. Incorporating insights into decision workflows ensures the uniform implementation of healthcare payer analytics strategies across the organization.
Future of Healthcare Payer Analytics: What Does It Beholds?
The analytics landscape for healthcare payers is changing quickly. This shift is driven by advances in AI, cloud computing, and real-time data handling. These aren’t just technical upgrades; they are fundamentally transforming how payers make decisions, manage their costs, and get better results for their members. Here are the future trends that are expected to revolutionize the future of healthcare payer analytics:
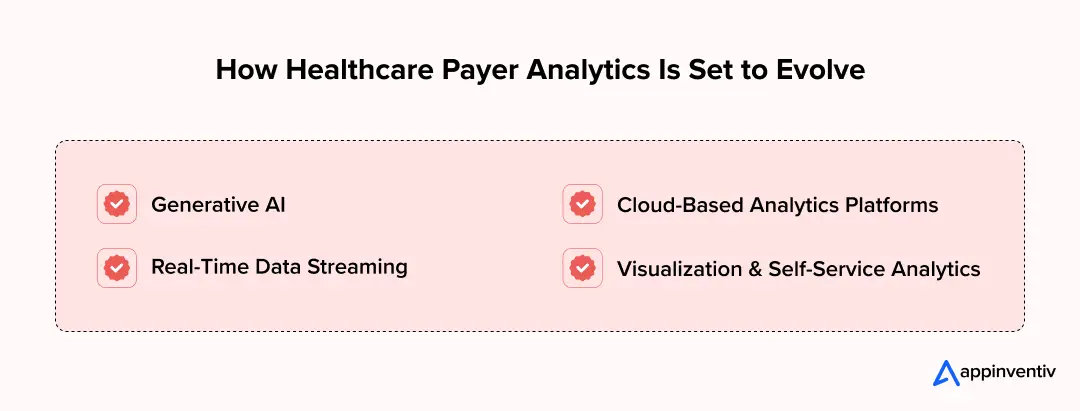
Generative AI
Generative AI in healthcare is not only improving in terms of prediction, but it can also generate something new out of more complicated data. It is able to integrate clinical, claims, and operational data to derive unambiguous summaries, personalized reports, and scenario models.
This helps the payer teams by experimenting on the possible impacts of new care management steps on cost, utilisation, or member outcomes before implementing them. The outcome is more stable planning and quicker and more assertive decisions.
Cloud-Based Analytics Platforms
Cloud infrastructure helps payers put fragmented data together. It also allows analytics workloads to scale up exactly when needed, reducing reliance on expensive old systems. Modern cloud platforms in healthcare support secure, compliant storage while giving near-instant access to insights across claims, member, and provider data.
Real-Time Data Streaming
Historically, healthcare payer data analytics used to rely on batch processing of old claims. Now, emerging real-time streaming technologies let payers track claims, utilization, and member activity as the event actually occurs. This change allows for immediate action, like preventing an unnecessary ER visit or flagging anomalous billing patterns instantly.
Visualization and Self-Service Analytics
Interactive dashboards and self-service tools give business teams the power to explore insights without needing IT help every time. Visual analytics makes trends and anomalies easy to spot, improving both the speed and the confidence behind decision-making.
Appinventiv’s Insights
Payer analytics will move towards active orchestration of results rather than mere analysis of historical data in the near future. Not only will the systems identify patient risks or anomalies in claims, but they will also automatically trigger the appropriate interventions. This predictive orchestration will reshape payers’ processes for cost and care management.
How Appinventiv Can Help Build a Custom Healthcare Payer Analytics Solution
Healthcare payer analytics is changing how insurers and payers operate. It affects how they make decisions, manage costs, and get better results for their members. By converting claims and member data into useful intelligence, payers gain the ability to optimize operations, detect fraud, predict high-risk cases, and deliver more personalized care.
Building a custom healthcare payer analytics solution becomes achievable when partnering with a skilled technology provider like Appinventiv. Through our healthcare software development services, you can seamlessly manage complex data, refine operational workflows, and create reliable analytical models. With steady engineering support and domain experience, we help teams design platforms that improve insight quality, strengthen compliance, and support long-term digital growth.
Appinventiv has extensive experience in healthcare projects like Soniphi, Health-e-People, and DiabeticU, demonstrating their ability to integrate various data sources, deploy advanced analytics, and deliver platforms that are secure, scalable, and compliant.
Whether the need involves predictive risk modeling, real-time monitoring, or interactive dashboards, these proven capabilities ensure payers can pull the maximum value from their data. Appinventiv’s data analytics services further empower organizations. They transform complex claims and member information into actionable insights that improve the quality of care, operational efficiency, and financial performance.
With the right technology partner and a sound approach, healthcare payer analytics is more than just a tool. It functions as a strategic advantage. It drives smarter decisions, better outcomes, and a measurable return on investment (ROI) across the healthcare ecosystem.
To learn more about our expertise and projects, we have worked on, take a quick glance at our portfolios and client testimonials, which reflect our dedication to every project we take on.
Connect with our experts today to discuss your project idea.
FAQs
Q. How do payers use data analytics?
A. Data analytics help payers to analyze provider performance, the behavior of members, and claims. It assists in pinpointing high-risk groups, detecting fraud, containing costs, optimizing provider networks, and tailoring care plans.
Using raw data to transform it into actionable information, payers will be able to make evidence-based decisions to enhance operational efficiency, improve member outcomes, and support value-based care efforts.
Q. How does healthcare payer analytics software help improve payer operations?
A. Healthcare payer analytics software enhances claims processing, identifies cost drivers, identifies anomalies, and tracks provider performance. It automates reporting, facilitates risk stratification, and provides predictive and prescriptive insights.
This increases the efficiency of operations, lowers errors, improves compliance, and gives payers the capability to take charge in managing costs, member engagement, and network performance.
Q. What are the types of analytics in healthcare?
A. Some of the common types of healthcare analytics for payers:
Claims Analytics: Analyzes healthcare insurance claims data to determine trends, abnormalities, and cost optimization opportunities.
Risk Adjustment Analytics: Evaluates the risk profile of members in order to recompense them appropriately and to manage the population.
Predictive and Risk Modeling Analytics: Anticipated high-risk patients, disease development, and future usage.
Financial Analytics: Monitors spending, revenue, and accuracy of payments to enhance financial performance.
Quality and Outcomes Analytics: Evaluates provider outcomes and patient outcomes to facilitate value-based care.
Utilization Analytics: This is an analysis of the utilization of healthcare services to achieve an access-cost balance.
Health Equity Analytics: Determines the differences in care access, quality, and outcomes among populations.
Descriptive, Diagnostic, Predictive and Prescriptive Methods: These are the various methods of analysis applied in all payer data functions.
Q. What are some of the recent trends in healthcare plan analytics?
A. The top trends in healthcare plan analytics include:
Generative AI for insights and reporting: Generates self-updating reports and models scenarios to do more effective planning.
Scalability through cloud-based analytics: Data aggregation to mitigate risk and reliance on old systems.
Real-time data streaming for immediate interventions: Provides immediate tracking of claims, costs, and utilization.
Intelligent visualization and self-service dashboards: give users the ability to access insights independently.
Integration of behavioral and social determinants of health data: Offers a comprehensive picture of health among the members to implement specific interventions.
Q. What are some of the key benefits of healthcare payer analytics?
A. Some of the common benefits of healthcare payer analytics include:
Enhanced Cost Effectiveness: Determines spending patterns and eliminates waste in claims and care delivery.
Improved Risk Management: Early prediction of high-cost cases can be done, and proactive interventions done.
Better Member Experience: Utilizes insights to make plans personal and enhance engagement.
Fraud Detection: Notifies suspicious billing and claim abnormalities prior to the processing of payment.
Compliance with Regulations: Makes it easy to comply with payers with transparent, auditable data.
Data-Driven Decisions: Interactive, real-time, and accurate perspective of financial, clinical, and operational performance.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How Custom Healthcare App Development is Powering Digital-First NHS Care
Key Highlights: NHS teams are moving fast toward digital-first care, and custom apps are filling gaps that the standard NHS App cannot cover. Custom healthcare apps help reduce workload, cut waiting times, and improve how patients access care across Trusts and ICS regions. UK rules such as DTAC, NHS DSP Toolkit, NHS Login, and UK…

How to Implement Denial Management Automation in Healthcare
Key Takeaways Denial management works best when prevention is prioritized before recovery, starting at registration, eligibility, and authorization. Automation delivers the most value when introduced in phases, aligned with existing revenue cycle maturity. Clean data, clear ownership, and consistent denial categorization matter more than tools alone. Analytics and AI help teams focus on high-impact denials,…

SMART on FHIR App Development – Benefits, Process, Features, Costs
Key takeaways: SMART on FHIR brings FHIR's data exchange standard together with SMART's authorization for secure access, providing complete interoperability between EHR systems. The proportion of hospitals that provide app-based access increased to over 82% in 2025. SMART on FHIR applications enable secure access, real-time data sharing, and role-based workflow for patients, clinicians, and administrators.…