- Why RCM Software is Essential for Healthcare Providers
- Market Insights: Healthcare RCM Software Landscape
- AI and Machine Learning Integration:
- Cloud-Based Solutions:
- Customization Over Off-the-Shelf Solutions:
- Increased Adoption of Automation:
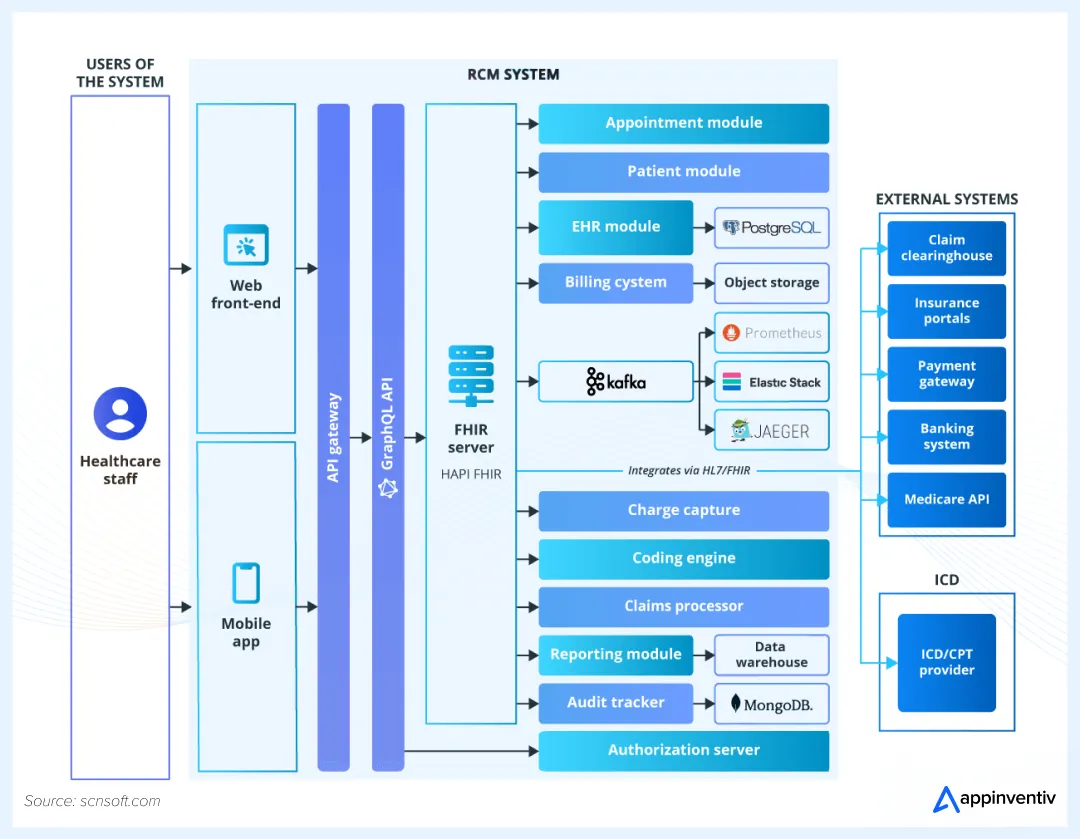
- Sample of Enterprise RCM Software Architecture for Healthcare
- Key Steps in Revenue Cycle Management Software Development
- Step 1: Business Analysis and Requirements Gathering
- Step 2: Technical Design
- Step 3: UX/UI Design
- Step 4: Development and Testing
- Step 5: Deployment & Post-Launch Support
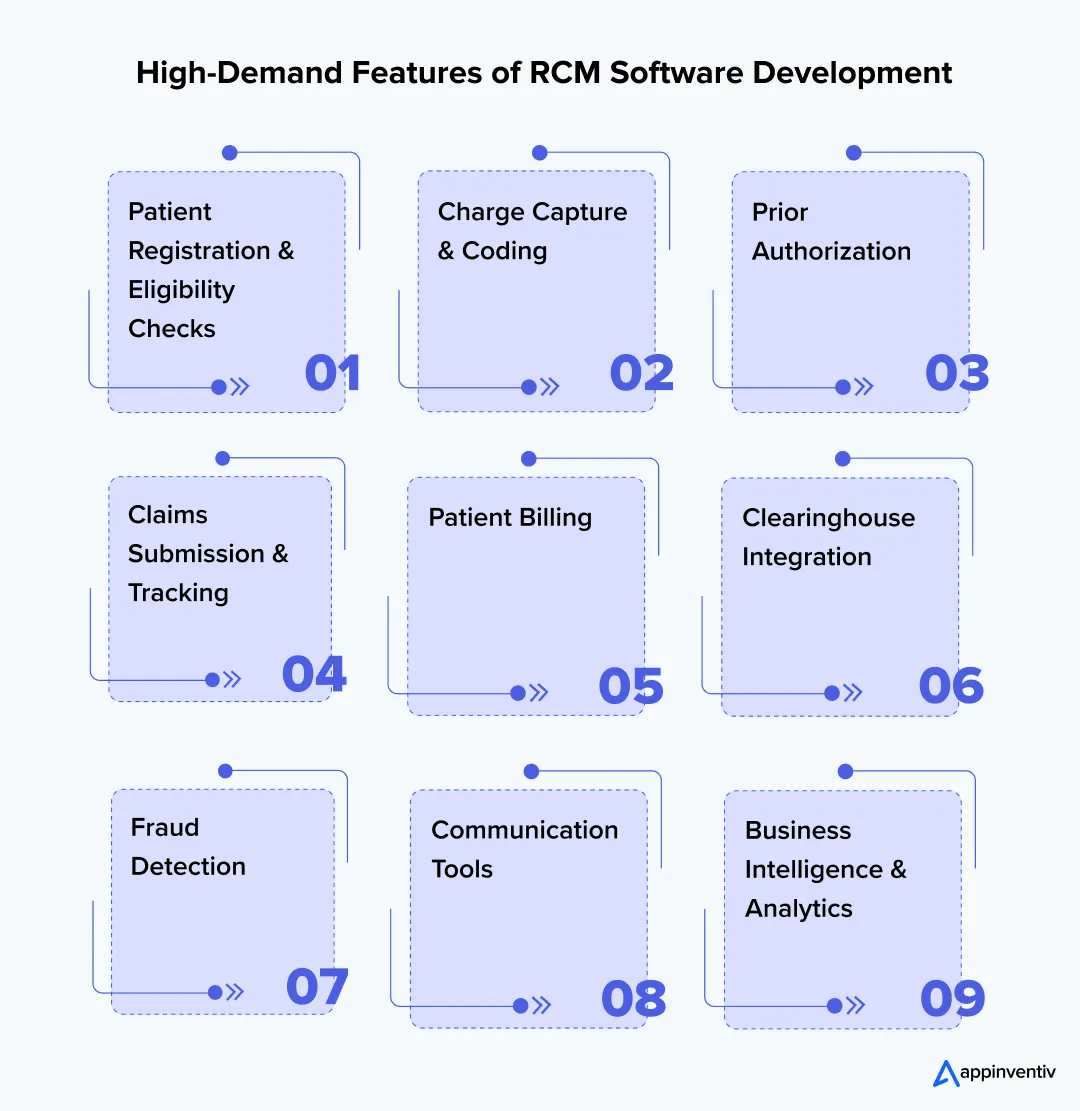
- Key Features of Revenue Cycle Management Software in Healthcare
- Patient Registration & Eligibility Checks
- Charge Capture & Coding
- Prior Authorization
- Claims Submission & Tracking
- Patient Billing
- Clearinghouse Integration
- Fraud Detection
- Business Intelligence & Analytics
- Communication Tools
- Tech Stack for Revenue Cycle Management Software Development
- Cost to Develop Custom Revenue Cycle Management Software
- Cost Breakdown
- The Future of RCM Software Development
- 1. AI and Predictive Analytics
- 2. Blockchain Technology
- 3. Telemedicine Integration
- Why Choose Appinventiv for Building Your RCM Software?
- 1. Expertise in Healthcare Solutions
- 2. Cutting-Edge AI-Driven Solutions
- 3. Tailored to Your Needs
- 4. End-to-End Support
- 5. Cost-Efficient Custom Solutions
- Final Thoughts
- FAQ'S
Key takeaways:
- Healthcare revenue cycle management software includes key components like claim submission, patient insurance verification, and automated patient billing.
- The development cost typically ranges from $40,000 to $600,000+, depending on feature complexity, automation level, and integration requirements.
- AI, machine learning, and blockchain are transforming RCM software and will continue driving innovation in healthcare financial systems.
- Appinventiv provides customized RCM solutions that ensure scalability, security, and compliance for healthcare organizations.
Managing the financial side of healthcare can feel like a constant uphill battle. There’s always paperwork to handle, claim denials to deal with, and the need to stay compliant with changing regulations. The challenges are real.
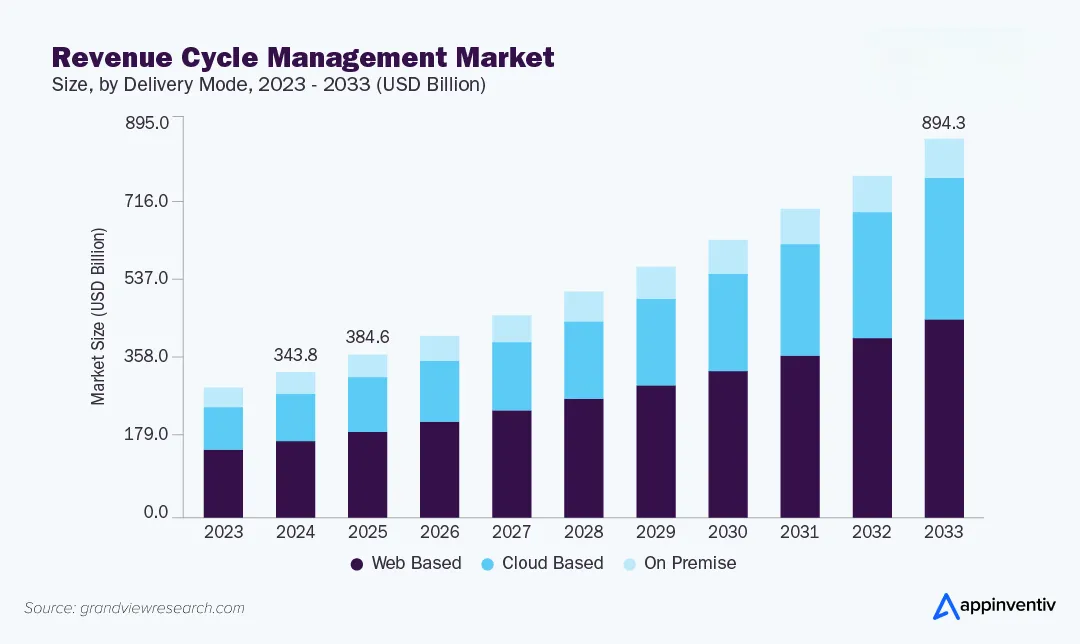
Slow reimbursement cycles and billing errors can seriously affect your cash flow. In fact, Grand View Research predicts the global RCM market will grow from $343.78 billion in 2024 to $894.25 billion by 2033. This shows just how important effective revenue cycle management is for healthcare providers.
It’s not just about any RCM software development—it’s about custom-built solutions that fit your needs, automate tasks, and cut down on costly mistakes. The healthcare industry is changing quickly. Sticking with outdated systems won’t keep your business competitive.
In this blog, we’ll guide you through everything you need to know about healthcare revenue cycle management software development that works for your practice or business.
Improve your healthcare facility by building an AI-powered RCM software.
Why RCM Software is Essential for Healthcare Providers
Healthcare providers need to improve how they handle money. But many still rely on manual work or old systems that make things harder. Poor billing and payment processes lead to lost revenue and extra paperwork.
Claim denials are one of the biggest problems healthcare providers deal with, and implementing denial management automation can significantly reduce these losses while improving cash flow. Such claims lead to wasted time, lost revenue, and additional work for staff.
Revenue cycle management software simplifies this whole process. It automates everything – from patient registration to payment collection. This automates tasks, improves accuracy, and reduces manual efforts.
RCM software connects all financial processes with systems like EHRs and practice management tools. This cuts down on errors and delays.
The benefits of revenue cycle management software adoption are clear:
- Faster Reimbursement: Automated claim submissions and real-time tracking can speed up payment processing.
- Fewer Billing Errors: Coding and claim scrubbing automation reduce human errors that cause denials and rework.
- Better Compliance: Helps stay updated with changing regulations like HIPAA and ICD-10, without manually tracking each update.
| In short, the right revenue cycle management system implementation can improve your healthcare businesses’ bottom line. It can boost cash flow, and cut down on administrative work. This lets your team focus more on what matters most: patient care. |
Market Insights: Healthcare RCM Software Landscape
As the demand for efficient billing and revenue management solutions grows, the healthcare revenue cycle management software development market is also expanding.
We have already seen the growing need for automated and efficient billing and payment solutions in healthcare. As providers face higher costs and more complex billing, RCM software is becoming crucial to maximize revenue, speed up payments, and maintain compliance.
Here’s how the RCM landscape is evolving:
AI and Machine Learning Integration:
AI is transforming healthcare revenue cycle management software development by:
- Predicting claim denials before they are submitted. It is done using past data.
- Spotting fraudulent claims and errors in real-time.
- Improving coding accuracy by automating charge capture and suggesting correct codes.
- Using predictive analytics to forecast payment cycles and improve cash flow management.
Cloud-Based Solutions:
More healthcare businesses are now moving to cloud-based RCM platforms. The reason being the benefits it offers, like:
- Remote access: Healthcare providers and billing teams can access RCM systems from anywhere, offering more flexibility.
- Data security: Cloud-based systems provide strong encryption and comply with data security rules.
- Scalability: Cloud solutions can easily grow with practices, without the need for expensive on-site infrastructure.
Customization Over Off-the-Shelf Solutions:
Healthcare providers are increasingly opting for custom revenue cycle management software development over generic, off-the-shelf solutions. A tailored solution offers many benefits:
- Seamless integration: Custom RCM systems can be designed to work smoothly with existing healthcare systems. These can include EHRs, practice management software, and insurance portals.
- Adaptability: These solutions can be tailored to fit the unique needs of different practices. This makes workflows more efficient and reduces manual work.
- Improved compliance: Customized solutions help ensure that the system stays up-to-date with changing regulations. This lowers the risk of legal penalties.
Increased Adoption of Automation:
Healthcare providers are using automated RCM systems to improve efficiency. This automation helps them with:
- Faster claims processing: It speeds up claim submissions and tracking.
- Reduced human error: These automated systems remove manual data entry mistakes which reduce claim denials and rework.
- Improved patient experience: Automation makes billing communication easier. This allows patients to view and manage their bills more easily.
| The RCM landscape is changing quickly. Healthcare providers who adopt these trends will be better equipped to simplify their financial operations, reduce administrative work, and improve revenue management. |
Sample of Enterprise RCM Software Architecture for Healthcare
An effective RCM software architecture integrates different modules. These components work together to ensure a smooth, automated flow of information across the revenue cycle.
Key Steps in Revenue Cycle Management Software Development
Building custom RCM software isn’t something you rush through. Each step matters. Miss one, and you’ll pay for it later. Let’s have a look at the healthcare revenue cycle management software development process.
Step 1: Business Analysis and Requirements Gathering
First, figure out what you really need. Not what sounds good in a sales pitch—what actually solves your problems.
- Identify Stakeholders: Sit down with the people who’ll use this system daily. CFOs, revenue cycle managers, billing specialists. They know where the system breaks down. Their input shapes everything that comes next.
- Understand Pain Points: Dig deeper into your current workflows. Where do claims get stuck? Which processes cause the most errors? What slows your team down? Find the bottlenecks that need attention.
- Compliance Needs: HIPAA and GDPR aren’t suggestions. They build compliance into the foundation. It ensures that patient data stays protected from day one.
Step 2: Technical Design
Next, map out how the software will actually work behind the scenes.
- System Architecture: Plan a structure that grows with your practice. The system needs to handle more users, more data, more transactions as you expand. It also needs to play nice with your EHRs and insurance portals. The right EHR-CRM integration makes or breaks modern healthcare operations.
- Tech Stack: Technology choices matter. Pick tools that offer real flexibility. ReactJS for responsive interfaces. NodeJS for solid backend performance. Cloud services like AWS for reliability and scale. These aren’t buzzwords—they’re practical choices.
Step 3: UX/UI Design
Your team shouldn’t need a computer science degree to use this software.
- User-Friendliness: The design interfaces should make sense the first time someone opens them. Clean layouts. Clear buttons. Logical workflows. Your team gets up to speed fast with minimal training.
- Mobile Compatibility: Healthcare doesn’t stop when people leave their desks. The software works just as well on phones and tablets. Your staff can check claims, verify coverage, or review reports from anywhere.
Step 4: Development and Testing
This is where the healthcare revenue cycle management software development really happens. Code gets written. Features come to life.
- Agile Development: The software is built in stages, not all at once. You see progress quickly. Changes happen faster. Problems get caught early.
- Security Testing: The QA team puts the software through serious stress tests. Does encryption work properly? Are RCM data privacy and compliance standards actually private? Does multi-factor authentication stop unauthorized access? Verify HIPAA compliance at every level. Security isn’t an afterthought.
Step 5: Deployment & Post-Launch Support
The final step is launching the system. But that’s not the end; make sure it continues to work well over time.
- Deployment on Cloud: Launch your ECM software on AWS or Azure for maximum uptime and security. Cloud platforms give you the scalability you’ll need as you grow.
- Continuous Monitoring: Watch the system after it goes live. Bugs get fixed fast. Performance issues get addressed immediately. Regular updates keep the software current and efficient.
This process ensures your RCM software development delivers what you actually need. It stays compliant with changing regulations. And it’s built to grow alongside your practice.
Key Features of Revenue Cycle Management Software in Healthcare
In revenue cycle management, certain features are highly important for healthcare providers that aim to simplify billing and payment processes. These features can improve efficiency, accuracy, and compliance. Here’s a breakdown of the most crucial features driving the success of RCM software.
Patient Registration & Eligibility Checks
What It Does: Automatically checks patient information. Including insurance details, by connecting with EHR and payor systems.
Real-World Example: Northwell Health, a major healthcare provider in New York, used automated eligibility verification across their facilities. This cut claim rejections by 25%. It makes sure that only insured patients were scheduled for services covered by their insurance, preventing unpaid claims.
Also Read: How to Build Patient Management Software?
Charge Capture & Coding
What It Does: The system pulls charges directly from your EHR. No manual data entry needed. It applies the correct medical codes automatically—ICD-10, CPT, whatever’s required. Built-in compliance checks catch mistakes before they become problems.
Real-World Example: Sutter Health in Northern California put this to the test. They’re a massive health system, so their numbers matter. The software started applying ICD-10 codes automatically to every patient visit.
The results? Coding errors dropped by 30%. That’s huge. Fewer errors meant fewer claim denials. Fewer denials meant faster payments. Their entire reimbursement cycle sped up because the codes were right the first time.
Prior Authorization
What It Does: It automates the process of getting advance authorization from insurance companies. This helps in reducing delays in treatment.
Real-World Example: Memorial Hermann Health System in Texas used an automated prior authorization system. This helped them in cutting the time spent on phone calls and paperwork by 50%. This helped staff focus on other tasks, speeding up treatment approvals and improving efficiency.
Claims Submission & Tracking
What It Does: This connects with clearinghouses and tracks claims in real time. It uses AI-driven claim scrubbing to automatically find and fix errors before submission. This ultimately reduces claim denials.
Real-World Example: Mayo Clinic, a well-known medical center, added AI-driven claims tracking to its RCM system. This flagged potential errors before submission, leading to a 20% drop in claim denials, faster reimbursements, and better revenue flow.
Patient Billing
What It Does: It automates the entire billing process. Starting from creating invoices to sending reminders and processing payments. It also gives patients clear financial information. These medical revenue cycle management software development can be beneficial for the medicine suppliers to easily keep track of entire billing cycles.
Real-World Example: Cleveland Clinic, a nonprofit medical center, used an automated billing system. This sent patients monthly reminders and simple statements. This helped them boost patient payment rates by 40% and reduced the workload of manual billing.
Clearinghouse Integration
What It Does: It automates claim submissions to clearinghouses and provides real-time eligibility checks. This ensures claims are accurate and complete before submission.
Real-World Example: Ascension Health, one of the largest private healthcare systems in the US, connected their RCM software with clearinghouses. This led to a 15% increase in claims accepted on the first submission. The integration also streamlined eligibility verification, reducing repetitive tasks for front-office staff.
Fraud Detection
What It Does: This is an AI-powered fraud detection system that checks claims for issues like duplicate billing or upcoding and flags any suspicious activity.
Real-World Example: Aetna, a major health insurance company, used AI-driven fraud detection in their RCM system. They used it to spot suspicious billing patterns. This helped Aetna detect and prevent millions of dollars in fraudulent claims in the first year. It helped them protect both the insurer and healthcare providers.
Business Intelligence & Analytics
What It Does: It offers real-time dashboards, financial forecasting, and predictive analytics. This helps healthcare providers make data-driven decisions.
Real-World Example: HCA Healthcare is one of the largest hospital operators in the US. They added a business intelligence module to their RCM software. This helped them forecast revenue more accurately and optimize staff allocation. The company could identify underperforming locations and improved overall collections by 18%.
Communication Tools
What It Does: The communication tools provide secure, direct communication between healthcare providers and payors. This helps in speeding up claims resolution.
Real-World Example: Intermountain Healthcare in Utah adopted direct messaging tools within their RCM software. This streamlined communication with insurance companies, reducing the average time for claim resolution by 30%. The improved collaboration also made the patient experience better by providing clearer billing information.
These features are what make healthcare revenue cycle management software development valuable. It automates essential parts of the revenue cycle, from patient registration to claims submission and fraud detection. RCM software helps organizations reduce mistakes, simplify operations, and improve cash flow.
| Whether you have a small practice or looking to build revenue cycle management software for hospitals networks, these features can help. They can assist you to stay competitive, compliant, and profitable in the growing complexity of healthcare. |
Appinventiv builds secure, scalable healthcare software tailored to your workflow.
Tech Stack for Revenue Cycle Management Software Development
Choosing the right tech stack is essential for scalable, secure, and efficient custom RCM software development. Below is a simple breakdown of the key technologies often used in RCM software development.
| Layer | Technology | Purpose |
|---|---|---|
| Frontend | ReactJS, AngularJS, HTML5, CSS3 | Building user interfaces for web and mobile accessibility. |
| Backend | NodeJS, Python, Java | Handling server-side logic, processing, and API management. |
| Database | PostgreSQL, Microsoft SQL Server | Storing and managing large amounts of structured data securely. |
| Cloud | AWS, Microsoft Azure, Google Cloud | Hosting, scalability, and ensuring high availability. |
| Security | SSL/TLS, AES encryption, OAuth | Ensuring data security and regulatory compliance (HIPAA). |
| APIs | FHIR, HL7, REST APIs | Integrating with EHR, insurance providers, and other systems. |
| Testing | Jest, Mocha, Selenium | Ensuring quality, functionality, and security during development. |
This tech stack ensures the system is secure, scalable, and able to work with other healthcare systems. It also helps manage sensitive data efficiently.
Cost to Develop Custom Revenue Cycle Management Software
The cost of custom revenue cycle management software development can vary based on several factors. This includes the size and type of businesses that need healthcare software. You may also want to read how to build a medical practice management software.
Below is a detailed breakdown of the costs, including ongoing maintenance.
Cost Breakdown
The cost to develop custom RCM software typically ranges from $40,000 – $600,000+. The final cost depends on factors like the complexity of features, automation level, and integration needs. Here’s a closer look at these cost factors:
Basic RCM Software:
- Cost Range: $40,000 – $100,000+
- Includes: Basic functions like patient registration, claims processing, billing automation, and integration with EHR systems.
- Features:
- Claims submission
- Charge capture
- Basic reporting and analytics
- Integration with EHR and insurance portals
- Manual coding (non-AI-driven)
Mid-Range RCM Software:
- Cost Range: $100,000 – $400,000+
- Includes: Advanced features like automated claim scrubbing, fraud detection, and business intelligence (BI) tools.
- Features:
- AI-assisted coding
- Denial management
- Advanced reporting and analytics
- Integration with clearinghouses
- Patient billing automation
High-End RCM Software:
- Cost Range: $200,000+ to $600,000+
- Includes: Full-scale custom RCM systems with advanced AI, machine learning, and predictive analytics. These systems manage large operations and can be customized for complex revenue models.
- Features:
- AI-powered fraud detection
- Predictive billing and forecasting
- Real-time reporting dashboards
- Integration with complex systems like multi-entity healthcare networks
- High scalability for large organizations
Example of Cost Breakdown
| Feature/Service | Basic | Mid-Range | High-End |
|---|---|---|---|
| Core RCM Functionalities | ✔️Patient Registration | ✔️Patient Registration | ✔️Patient Registration |
| Claims Processing | ✔️Manual | ✔️Automated | ✔️Automated & AI-driven |
| Billing Automation | ✔️Basic | ✔️Advanced | ✔️Fully Automated |
| Business Intelligence | ✔️Reporting & Analytics | ✔️Predictive Analytics | |
| Fraud Detection | ✔️AI-powered Fraud Detection | ||
| Integration with EHRs | ✔️ | ✔️ | ✔️ |
| Customization | Limited | Moderate | Fully Customizable |
Additional Costs
Ongoing maintenance
Building the software is just the start. You’ll need to keep it running smoothly after launch. The cost of software maintenance adds up with the basic development.
Expect to pay 15% to 20% of your initial development cost each year. Yes, every year. This might sound steep, but here’s what you’re getting:
What’s Included:
- Security updates that protect your system from new threats
- Bug fixes when something breaks or doesn’t work right
- Patches that close security holes before hackers find them
- System upgrades to stay compatible with new regulations
- Technology updates so your software doesn’t become outdated
- Feature improvements based on what your team actually needs
- Enhancements that make daily tasks easier and faster
Example:
Let’s say your custom RCM software costs $1,000,000 to build. Plan on spending around $150,000 per year for maintenance. That’s not money disappearing into a black hole. It’s what keeps your system functional, secure, and compliant.
Healthcare regulations change constantly. New security threats pop up monthly. Your software needs regular attention to keep up. Skip maintenance, and you’re asking for trouble down the road.
Integration costs
Your RCM system doesn’t exist in a vacuum. It needs to talk to your other software.
Maybe you’re using an EHR system already. You’ve got patient portals running. Your team works with multiple insurance payor systems. All of these need to connect smoothly with your new RCM platform.
These connections cost extra. How much? It depends on what you’re connecting to and how complicated it gets.
Cost Range: $50,000 to $250,000.
The price varies based on several factors. How many systems are you linking together? Are they modern platforms with easy APIs? Or older legacy systems that need custom workarounds? Each integration has its own challenges.
Healthcare revenue cycle management software development requires real money upfront. The additional costs don’t stop after launch either. Maintenance, integrations, updates—they all add up.
But here’s the thing: the long-term benefits outweigh these costs. A well-built RCM system pays for itself.
Think carefully about what you actually need. Don’t buy features you won’t use. Focus on capabilities that solve your specific problems. Match the solution to your budget and business goals.
The right RCM software development investment makes financial sense. The wrong one just drains resources without delivering results. Choose wisely.
For healthcare organizations planning custom RCM solutions, refer to our comprehensive guide to software development cost to budget effectively for your digital transformation.
The Future of RCM Software Development
The future of healthcare revenue cycle management software development is exciting, with technology evolving and creating new possibilities. Here’s a look at what’s coming next.
1. AI and Predictive Analytics
AI isn’t just coming to RCM—it’s already changing the game. But what we’re seeing now is just the beginning.
Imagine knowing which claims will get denied before you even submit them. That’s where we’re headed. AI can look at your historical data and spot patterns. It flags potential problems early. Your team fixes issues upfront instead of dealing with rejections later.
Fraud detection is getting smarter too. AI systems now catch suspicious billing patterns as they happen. Not days later. Not weeks later. Right now. Bad actors get stopped before fraudulent claims go through.
Denial management is becoming almost automatic. AI doesn’t just identify denials—it tells you why they happened. More importantly, it shows you how to prevent the next one. Reimbursement cycles speed up because you’re not constantly resubmitting claims.
2. Blockchain Technology
Blockchain sounds complicated, but the benefits are straightforward. Think of it as a digital ledger that nobody can tamper with.
Every transaction gets recorded permanently. No one can go back and change the numbers. This cuts fraud risk dramatically. Everyone—providers, payers, patients—sees the same information. No more disputes about what was billed or when.
Data privacy gets a major upgrade with blockchain. Sensitive healthcare information stays locked down tight. Only people with proper authorization can access it. HIPAA compliance becomes easier to maintain, not harder.
3. Telemedicine Integration
Telemedicine has exploded in recent years. It’s not going away. RCM software needs to keep up.
Virtual consultations require different billing approaches. Remote payment collection works differently than front-desk transactions. Modern RCM software development must handle both seamlessly.
The good news? The technology is catching up fast. New systems track telemedicine payments just like in-person visits. Claims processing works the same way. Billing management doesn’t skip a beat, whether your patient is in the office or at home.
Telemedicine is also creating entirely new payment models. Subscription-based care. Remote monitoring fees. Virtual follow-ups. RCM software needs to handle all these variations automatically.
Also Read: How Much Does Telemedicine App Development Cost?
What This All Means
These advances aren’t just cool tech features. They solve real problems healthcare providers face every day.
AI makes your team faster and more accurate. Blockchain makes your transactions more secure. Telemedicine integration keeps you flexible as care delivery changes.
The healthcare revenue cycle management software development of tomorrow will be more powerful than what we have today. Fewer mistakes. Better security. Faster processing. Your staff will spend less time fighting with software and more time focusing on patient care.
The healthcare world moves fast. RCM systems that embrace AI, blockchain, and telemedicine will keep pace. The ones that don’t? They’ll get left behind.
Why Choose Appinventiv for Building Your RCM Software?
Looking for a partner to build custom RCM software? Appinventiv brings real expertise, fresh ideas, and reliable support to the table. Here’s what makes us different for your healthcare software development services:
1. Expertise in Healthcare Solutions
We’ve been doing this for over 10 years. That’s a decade of working directly with healthcare providers. We’ve seen the problems you deal with every day.
Our experts handle healthcare data security challenges carefully and implement best practices. Regulatory compliance? We handle it. Data security? It’s built into everything we create. Your system will meet HIPAA compliance and follow GDPR standards right out of the gate. Patient information stays protected. Your practice stays compliant. No shortcuts.
2. Cutting-Edge AI-Driven Solutions
We’ve deployed more than 150 AI models across different projects. We know how to make AI actually useful.
Our RCM solutions use artificial intelligence and machine learning in practical ways. Predictive billing that catches issues before they happen. Fraud detection that spots suspicious patterns instantly. Denial management that learns from past mistakes.
What does this mean for you? Fewer billing errors. Faster payments from insurance companies. Fraudulent claims get stopped before they cost you money. The technology works in the background while your team focuses on patient care.
3. Tailored to Your Needs
With 3000+ solutions designed and delivered, our software developers know every healthcare provider has unique needs. That’s why we customize our RCM software to fit your specific workflows, whether you run a small practice or a large hospital network.
Our solutions are flexible and designed to scale, ensuring they grow with your practice as it expands.
4. End-to-End Support
We have modernized over 500 legacy processes, so we understand the full scope. You could be wondering: What kind of support do we provide after RCM software implementation? Our experts provide complete support at every stage of your RCM software journey.
From initial consulting and development to post-launch maintenance, we’re here to help every step of the way. We make sure your system performs at its best with regular updates and troubleshooting support.
5. Cost-Efficient Custom Solutions
We don’t believe in throwing money at problems. Our approach focuses on smart spending that pays off over time.
Custom doesn’t have to mean expensive. We build solutions tailored to your needs without the bloated price tag. Every feature serves a real purpose for your practice.
Here’s what happens when we automate your revenue cycle: Cash starts flowing faster. Administrative costs drop. Your team spends less time on paperwork and more time on what matters.
The math is simple. Better efficiency means lower operating costs. Fewer errors mean fewer claim denials. Faster processing means quicker payments.
You’re not just buying software. You’re investing in a system that improves your bottom line month after month. Our healthcare revenue cycle management software development creates real financial impact.
The result? A cost-effective solution that strengthens your entire revenue cycle management process. You spend less, earn more, and run smoother operations.
We combine our 35+ industry expertise with advanced technology to create RCM software that supports your practice’s financial health. If you need a partner who understands your needs and delivers results, we’re here to help.
Appinventiv automates billing and enhances accuracy, improving cash flow and efficiency.
Final Thoughts
The numbers tell a clear story. The RCM software market will reach $65.7 billion by 2031. That’s massive growth. It shows how badly healthcare organizations need better, customized RCM solutions.
Yes, there are challenges in revenue cycle management automation. You’ll face hurdles during implementation. But here’s the thing: investing in RCM software now puts you ahead of the curve.
Why does this matter? Healthcare is getting more competitive every day. Regulations keep changing. Profit margins are tighter than ever. The right RCM software helps you handle all three.
Organizations that invest today will be ready for tomorrow. They’ll stay compliant with new rules. They’ll run more efficiently. And they’ll remain profitable as the market expands.
At Appinventiv, we’ve spent years building healthcare software that actually works. Our experts understand what makes healthcare different. Our custom solutions address the real problems providers face every day.
Ready to improve your revenue cycle? Let’s talk about what RCM software development can do for your organization.
FAQ’S
Q. What is revenue cycle management in healthcare?
A. Healthcare revenue cycle management software development handles the money side of healthcare. It manages payments between doctors, patients, and insurance companies.
The process starts when a patient books an appointment. It includes checking their insurance, creating bills, sending claims, and collecting payments. The main goal? Make sure doctors and hospitals get paid correctly and on time. It also cuts down on mistakes and paperwork.
Q. How to ensure HIPAA or GDPR compliance in an RCM platform?
A. Keeping patient data safe is the top priority. Your RCM platform needs strong security measures in place.
This means encrypting all sensitive information. Set up proper access controls so only authorized people can view data. Keep the system updated to meet new rules and regulations.
You’ll also need audit logs to track who accessed what. User permissions help control what each team member can see. Secure data transmission protects information as it moves through the system.
Q. What are the main types of healthcare revenue cycle management software?
A. There are five main types of RCM software used by healthcare providers:
- Claims Processing Software – Automates claim submission, validation, and tracking to reduce denials and speed up payments.
- Billing and Invoicing Software – Handles end-to-end billing, invoicing, and payment collection to improve cash flow.
- Medical Coding Software – Ensures accurate use of ICD-10 and CPT codes to reduce claim errors and maintain compliance.
- Analytics and Reporting Software – Provides real-time insights into revenue performance, payer behavior, and claim trends.
- Patient Eligibility Verification Software – Checks insurance coverage instantly to prevent denied claims and billing delays.
Each type plays a vital role in streamlining operations, improving accuracy, and ensuring faster reimbursements across the revenue cycle.
Q. How long does it take to develop revenue cycle management software?
A. RCM software development time varies based on what you need. A basic system might take 3-4 months. More complex platforms can take up to 12 months.
What affects the timeline? The number of features you want. Whether you need AI and advanced analytics, how many other systems does it need to connect with? The size of your healthcare organization also plays a role.
Q. Which is the most commonly used revenue model?
A. Fee-for-service is still the most popular revenue model in healthcare. Here’s how it works: providers get paid for each service they perform. Each test, procedure, or appointment generates a separate charge.
You’ll find this model everywhere. Hospitals use it. So do clinics and private practices.
But things are changing. More organizations are moving toward value-based care. This newer model focuses on patient outcomes instead of the number of services. It rewards quality over quantity.
Q. What are the seven steps in the revenue cycle in healthcare?
A. The revenue cycle has seven main steps:
- Pre-Registration: Gather patient details before their appointment.
- Registration: Double-check and enter all patient information correctly.
- Eligibility Verification: Confirm the patient’s insurance will cover the services.
- Charge Capture: Document all services provided during the visit.
- Coding: Assign the correct medical codes for diagnoses and treatments.
- Claim Submission: Send the claim to the insurance company.
- Payment Collection: Receive payment and chase down any unpaid claims.
Each step matters. Skip one, and you risk delayed payments or claim denials. Get them all right, and providers receive accurate payment on time.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…