- Rethinking Access: Strategic Gaps in Mental Health Delivery
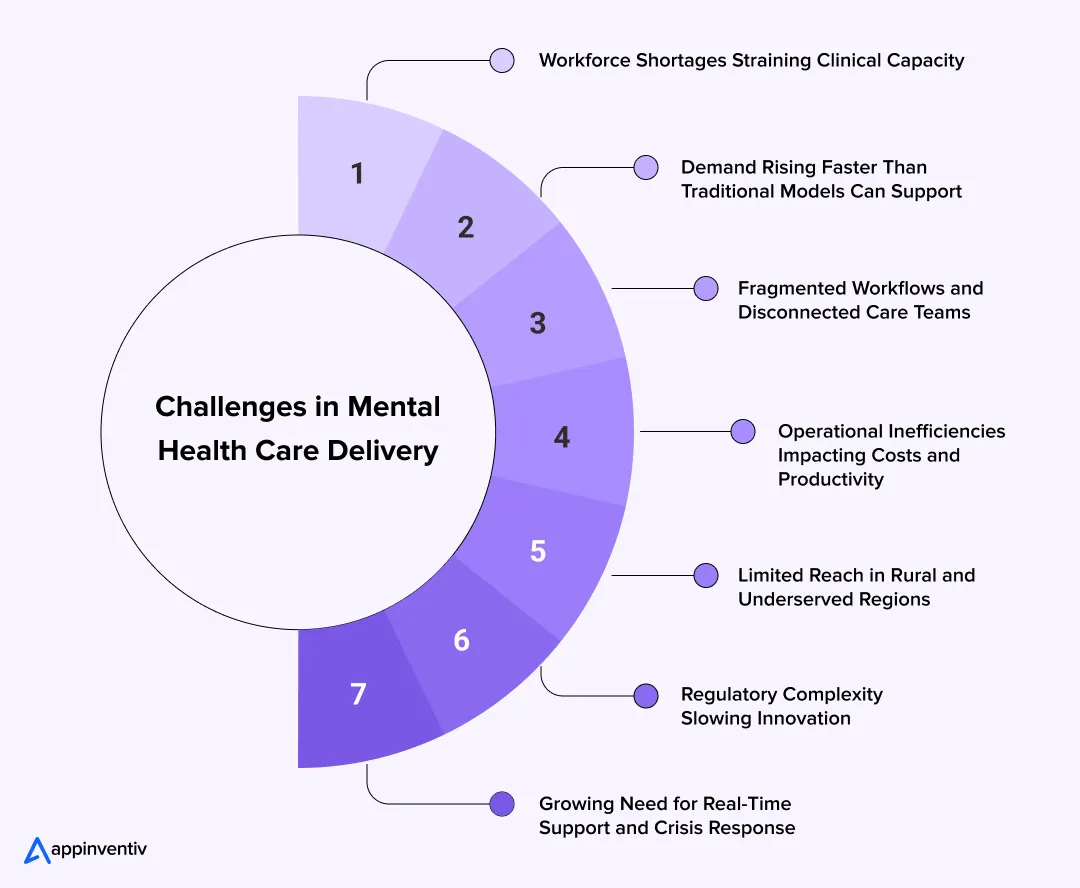
- Workforce Shortages Straining Clinical Capacity
- Demand Rising Faster Than Traditional Models Can Support
- Fragmented Workflows and Disconnected Care Teams
- Operational Inefficiencies Impacting Costs and Productivity
- Limited Reach in Rural and Underserved Regions
- Regulatory Complexity Slowing Innovation
- Growing Need for Real-Time Support and Crisis Response
- How Telemedicine Breaks Down The Barriers of Smooth Mental Health Care Delivery
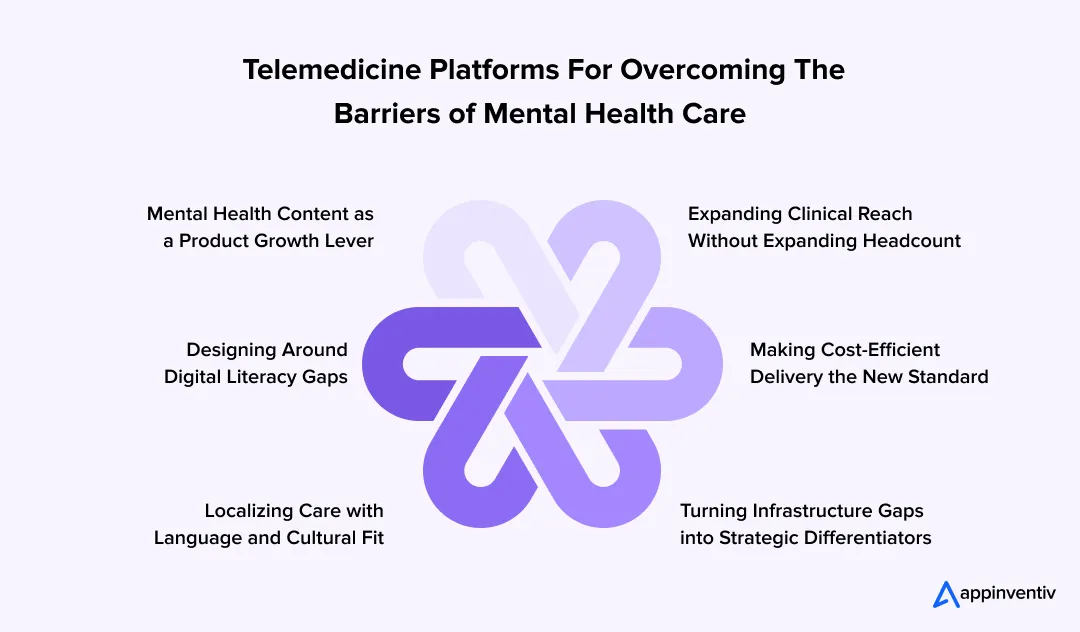
- Expanding Clinical Reach Without Expanding Headcount
- Making Cost-Efficient Delivery the New Standard
- Turning Infrastructure Gaps into Strategic Differentiators
- Localizing Care with Language and Cultural Fit
- Designing Around Digital Literacy Gaps
- Mental Health Content as a Product Growth Lever
- Benefits of Telemedicine for Mental Health Care
- The Other Side of the Screen: Unpacking Telemedicine's Unique Challenges in Mental Health Delivery
- Persistent Digital Divide
- Technical Glitches and Connectivity Issues
- Interstate Licensing and Regulatory Complexities
- Limitations in Crisis Intervention and Acute Care
- Building Therapeutic Rapport and Non-Verbal Cues
- The Future of Telemedicine in Mental Health: A Vision for Integrated Care
- Continuous Support Instead of Weekly Check-ins
- AI-Powered Early Intervention
- Data-Led Early Intervention
- Collaborative Care Across Locations
- Blended Community Support
- A More Human Form of Digital Care
- Wearables and Remote Monitoring for Proactive Care
- Hybrid Care Models (In-person + Virtual)
- Leverage Appinventiv's Expertise for Mental Health Telemedicine Development
- FAQs
Key Takeaways
- Telemedicine is helping healthcare systems close gaps caused by clinician shortages, long wait times, and limited physical infrastructure.
- Virtual mental health care boosts access beyond geographical barriers while reducing no-shows, travel barriers, and scheduling conflicts.
- Hybrid models, remote monitoring, and AI-supported assessments make care more continuous, proactive, and scalable.
- Partner with Appinventiv to build a secure and scalable telemedicine platform for mental health care
A health system expands its behavioral health services, only to discover that demand still outpaces capacity. Clinics have open hours, but not enough licensed professionals. Patients drop out because scheduling doesn’t align with work shifts. High-acuity cases slip through the cracks during long gaps between appointments. The cost isn’t just clinical; it shows up in missed revenue, workforce strain, and declining engagement.
This is the operational pressure point many enterprises are dealing with today. And it’s the exact gap where telemedicine for mental health is proving its value. Virtual therapy rooms, AI-supported assessments, remote monitoring, and hybrid care models are aiding healthcare providers in reaching patients who were previously shut out by distance, scheduling barriers, infrastructure costs or even social stigma.
Evidently, virtual mental health care is no longer a side offering. It has become a core component of how organizations stabilize access, retain clinicians, and expand reach without expanding infrastructure. Telemedicine platforms help systems move away from episodic, location-bound interactions and toward continuous, flexible, data-supported care delivery. The results? Fewer no-shows, faster triage, broader coverage, and a measurable lift in patient satisfaction.
It’s not just a technology upgrade, it’s a strategic lever. Let’s dive into learn how telemedicine is helping healthcare organizations remove long-standing barriers in mental health access and delivery, and why leaders are now treating it as critical infrastructure rather than an optional add-on.
Rethinking Access: Strategic Gaps in Mental Health Delivery
When we talk about scaling telemedicine in mental health, it’s no longer just about enabling access, it’s about closing the operational gaps that hold back efficiency, cost control, and growth. For businesses building digital mental health technology platforms, identifying and addressing these weak spots early can mean the difference between real traction and stalled adoption.
Here are some of the most pressing issues:
Workforce Shortages Straining Clinical Capacity
Many healthcare organizations are trying to grow their mental health programs but simply don’t have enough clinicians to cover the demand. Teams are split across several sites, schedules rarely line up, and burnout keeps pulling experienced professionals out of the system. It leaves organizations with gaps in coverage that are hard to fill, even when budgets are available.
Demand Rising Faster Than Traditional Models Can Support
In 2026, people are more concerned about their mental health than ever before, but they face many challenges to get the right care at the right time. Clinics have fixed hours, limited rooms, and long queues that keep stretching. By the time an appointment opens up, a patient’s condition may have already improved or they have switched to another provider. This creates pressure not only on clinical staff but also on administrative teams trying to manage the backlog.
Fragmented Workflows and Disconnected Care Teams
Behavioral health often touches several departments, but the tools these teams use don’t always talk to each other. A psychiatrist may adjust a treatment plan without the therapist seeing the update. A primary care doctor may not know a patient who missed two counseling sessions. These gaps slow down decision-making and weaken continuity of care.
Operational Inefficiencies Impacting Costs and Productivity
The cost of delivering in-person mental health care adds up quickly. Rooms sit unused when patients cancel at the last minute. Providers lose valuable hours waiting for no-shows. Schedules are tight, and even small delays throw off the entire day. Providers can serve more patients and in less time if the care delivery model is not tied so closely to physical space.
Limited Reach in Rural and Underserved Regions
For systems that serve wide geographic areas, expanding mental health services is even harder. Recruiting specialists for remote locations takes months, sometimes years. Building new clinics isn’t always financially feasible. Many communities end up driving long distances for support or skipping care altogether.
Regulatory Complexity Slowing Innovation
The rules around behavioral health vary from state to state. Licensing, billing, and privacy expectations change frequently, and every update adds administrative work. Ensuring compliance across distributed teams becomes a full-time task. This makes it intimidating for organizations to modernize their care models.
Growing Need for Real-Time Support and Crisis Response
As cases become more complex, organizations are expected to respond faster. But without continuous visibility into how patients are doing between visits, problems often surface late. Teams are left reacting to crises instead of preventing them, which increases risk and strain on the system.
How Telemedicine Breaks Down The Barriers of Smooth Mental Health Care Delivery
The impact of telemedicine and mental health isn’t just seen in patient convenience. It’s showing up in how health systems operate, how quickly they respond, and how reliably they maintain care across locations. Below, we break down the specific ways telemedicine is helping organizations remove long-standing barriers and build stronger, more scalable mental health programs.
Expanding Clinical Reach Without Expanding Headcount
One of the biggest wins with telemedicine in mental health is how it breaks down those location barriers that have always held healthcare back. Think about traditional care – everyone has to show up in person. That puts a serious limit on who you can reach, burns out your providers with packed schedules, and leaves entire regions without adequate coverage.
Virtual platforms flip that script completely.
What This Means for Your Business:
When you remove geography from the equation, businesses can suddenly reach patients in rural areas or other underserved regions. No need to build physical clinics or hire local staff – that’s the beauty of it. This works whether you’re building a direct-to-consumer mental health app or adding wellness services to your existing enterprise offerings. You can make better use of the providers you already have, cut down on overhead costs, and tap into markets that would normally require significant upfront investment.
What you end up with is pretty compelling: better margins and wider reach, but your costs don’t just keep climbing as you grow. That’s not something you see with traditional healthcare models, where expanding usually means spending more on everything – staff, facilities, equipment. Here, the economics actually work in your favor.
Example: Horizon Healthcare in the U.S. uses virtual care to connect underserved rural patients with behavioral health specialists across facilities, reducing waitlists without hiring more clinicians. Their platform enables psychiatrists in urban centers to serve patients across multiple counties virtually, eliminating the need for patients to travel long distances for care and for providers to expand physical infrastructure.
Making Cost-Efficient Delivery the New Standard
Telemedicine cuts through a lot of the inefficiencies that bog down traditional healthcare. No more dealing with patient travel times, expensive infrastructure, or those admin bottlenecks that slow everything down.
The cost savings are obvious, but there’s more to it than that. You can experiment with dynamic pricing models via AI in telemedicine, offer scheduling that actually works around people’s lives, and give patients different ways to connect – video, phone, messaging, whatever works best for them.
What This Means for Your Business:
Moving away from those rigid, fixed-cost models opens up space to actually innovate. You can build tiered subscriptions that make sense for different budgets, create therapy bundles that people can actually afford, or even run AI-enhanced group sessions – all tailored to what your users can realistically pay.
Here’s what’s interesting: being cost-efficient doesn’t mean sacrificing the user experience anymore. It actually becomes part of what makes your platform attractive. When people can find options that work for their situation, they stick around longer.
This approach does a few things for your business. It keeps users engaged with your platform, creates new ways to generate revenue, and helps you actually meet the growing demand for affordable digital mental health services. And you can do it at scale, which is something the traditional model just can’t match.
Example: Talkspace offers lower-cost therapy subscriptions via messaging and asynchronous communication, reducing delivery costs while maintaining accessibility. Their subscription plans range from $276-$436 per month, compared to traditional in-person therapy costs of $175-$500 per session. The asynchronous messaging model allows therapists to serve more clients efficiently while patients get 24/7 access to communicate with their providers.
Turning Infrastructure Gaps into Strategic Differentiators
One of the biggest challenges in telemedicine for mental health is that digital access just isn’t equal across the board. Some users are dealing with spotty internet, outdated devices, or they simply don’t have the digital skills to navigate care tools effectively.
Most platforms look at this and think “problem.” The businesses that are actually winning? They see opportunity.
Think about it – if you can build something that works well for people with limited connectivity or older devices, you’re suddenly competing in a space where most others have essentially given up. That’s not a small market either. The companies that figure this out first are going to have a serious advantage.
What This Means for Your Business:
Platforms that prioritize low-bandwidth optimization and device compatibility from the ground up can reach markets that others simply miss. Make sure your app’s UI is intuitive – not just what looks good in demos – and you’re already ahead of most competitors.
Throw in some embedded tutorials or adaptive onboarding that adjusts to how people actually use your product, and you’ll see those drop-off rates improve. More people will stick around long enough to see the value.
Addressing digital inequity creates competitive advantages through expanded market access rather than purely altruistic outcomes. Optimizing products for older devices, limited connectivity, and suboptimal technical environments builds customer loyalty in underserved markets with fewer competitive alternatives. This loyalty translates into sustainable business growth.
Example: Alaska’s AFHCAN developed specialized telemedicine systems designed for satellite connectivity limitations, connecting 248 sites including 158 village health centers across an extensive rural network. Designing solutions specifically for challenging connectivity environments creates scalable healthcare delivery systems that competitors struggle to replicate effectively.
Localizing Care with Language and Cultural Fit
Scaling globally or even just across different regions in your own country takes more work than just running everything through Google Translate. The platforms that are actually succeeding in telemedicine and mental health get this. They’re putting real effort into cultural intelligence.
What does that look like? It means matching patients with therapists who actually understand where they’re coming from not just linguistically, but culturally. Someone who gets their background, speaks their language naturally, and understands the context that shapes how they think about mental health in the first place.
What This Means for Your Business:
When platforms get the cultural piece right, they see something interesting happen: people don’t bail quickly, and they engage more deeply with the service. That makes sense when you think about it – if users feel like the platform actually gets them, they’re more likely to stick around.
Building a multilingual support platform that doesn’t feel clunky, matching people with therapists who share similar backgrounds, and creating content that resonates with different communities are no longer optional. In crowded markets, this level of personalization can be the difference between someone trying your service once and becoming a paying subscriber for months or even years.
The competitive advantage here is pretty clear. When people feel understood, they stay. And when they stay, your revenue grows.
Example: Ginger.io expanded its teletherapy network with bilingual clinicians to better support Latinx communities in the U.S. The result was simple but telling: engagement rose because people finally felt understood, not just treated.
Designing Around Digital Literacy Gaps
You can build the most sophisticated platform in the world, but it won’t matter if people can’t figure out how to use it. There’s this barrier that doesn’t get talked about enough when it comes to using telemedicine for mental health – digital literacy.
A lot of users, particularly older adults or people who’ve never tried therapy before, hit a wall during onboarding. The interface that seemed intuitive to your development team suddenly feels overwhelming to someone who’s already nervous about seeking help. They might try once, get frustrated, and just give up entirely.
That’s a problem you can’t afford to ignore, especially when you’re trying to reach patients who could really benefit from the service but need a smoother path to get there.
What This Means for Your Business:
Building in guided tutorials, smart onboarding flows, and support features that actually work can make a huge difference in whether people stick around and feel good about using your service. It’s basically like having a customer success team built right into the product itself.
Here’s what’s interesting: the more intuitive you make your platform, the less hand-holding people need afterward. Users start feeling confident about navigating things on their own, which is exactly what you want.
When you help people actually use your platform well, you’re not just being nice – you’re protecting your business. Happy, confident users are the ones who keep paying and tell their friends about your service. That’s the kind of UX investment that pays for itself.
Example: Digital navigator programs in U.S. community clinics offer one-on-one tech support to help patients navigate virtual mental health platforms.
Mental Health Content as a Product Growth Lever
Telemedicine platforms have evolved way beyond just being appointment schedulers. The real impact of telemedicine in mental health happens when these platforms turn into full ecosystems.
For organizations aiming to provide long-term, structured care for mental health conditions, investing in behavioral health software solutions becomes essential alongside telehealth capabilities.
We’re talking about therapy sessions, sure, but also content libraries, self-guided programs, daily wellness tools – basically everything that keeps users connected to their mental health journey between appointments. It’s about creating touchpoints that matter, not just filling calendar slots.
This shift makes sense when you think about it. Mental health isn’t something that only matters during your weekly 50-minute session. People need support, resources, and engagement throughout their week. The platforms that get this right are the ones building lasting relationships with their users.
What This Means for Your Business:
Mental health education and digital tools are what actually drive people to keep coming back. When you integrate guided CBT modules, mindfulness exercises, or even short explainer videos, you’re building those habit loops that get people using your platform more often.
Content becomes this engine that pulls users back in regularly. And every time they engage, you get another chance to introduce them to additional services, gather feedback, or actually help them see better outcomes.
That’s the shift that matters – education stops being just some nice-to-have marketing feature and becomes the thing that actually powers your business. It’s not just about having more content; it’s about creating content that makes people want to come back tomorrow, and the day after that.
Example: Calm’s 2024 campaign aired mindfulness ads during election night TV coverage, driving brand recall and positioning mental health as part of daily life.
Interested in implementing telehealth mental health capabilities into your own health care system? Our Telemedicine App Development – The Ultimate Guide 2026 is for you. This blog breaks down the technology, architecture, compliance layers, and cost models behind building scalable virtual care platforms. It’s a helpful next step if you’re planning to modernize or expand your digital mental health offerings.
Benefits of Telemedicine for Mental Health Care
Beyond breaking down barriers, telemedicine and mental health together deliver tangible benefits that translate into improved care quality and operational efficiency for healthcare systems and, ultimately, better outcomes for patients. Here is how:
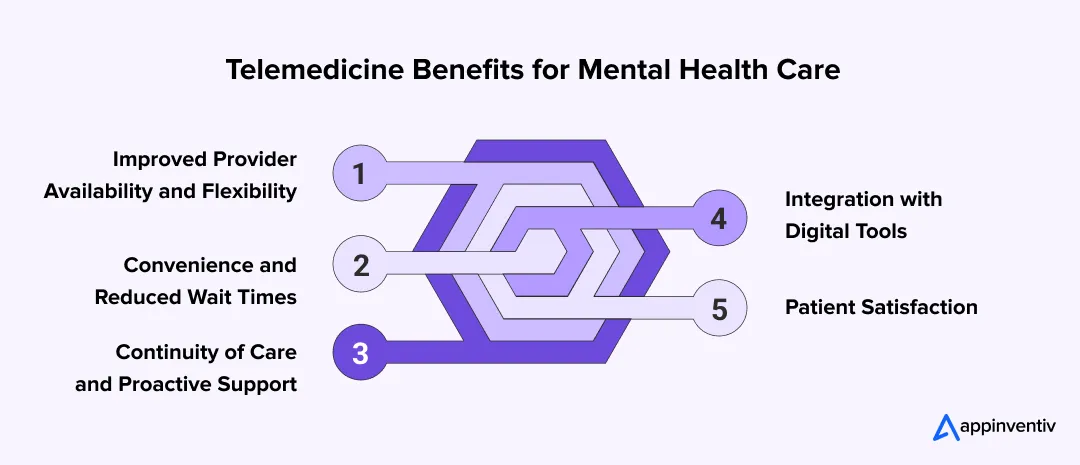
Improved Provider Availability and Flexibility
Telemedicine is an opportunity to handle more cases and provide a more flexible schedule, which may optimize provider capacity in an environment where there are shortages of mental health providers.
Convenience and Reduced Wait Times
With telemedicine, patients gain the incomparable ease of not having to travel to receive care, avoid missed appointments due to transportation issues, and experience greatly minimized waiting times. The results? Enhanced revenue, improved care, fewer cancelled appointments.
Continuity of Care and Proactive Support
One of the key benefits of telehealth for mental health is ensuring consistent care, especially for those with chronic conditions or need emergency care. The technology facilitates proactive check-ins and timely interventions, enhancing patients’ easy access to treatment plans.
Integration with Digital Tools
The seamless integration of telehealth tools with digital tools like mental health apps, IoT driven remote monitoring systems, and AI-powered analytics offers a holistic approach to continued care.
Patient Satisfaction
With telemental health, patients often show high levels of satisfaction, which in turn drives engagement and better adherence to treatment. This also validates the effectiveness of telehealth and mental health combined.
Bonus Read: Guide to Mental Health App Development for Businesses in 2026
Discover how your organization can expand mental health services with flexible, scalable telehealth platforms designed for today’s digital-first needs.
The Other Side of the Screen: Unpacking Telemedicine’s Unique Challenges in Mental Health Delivery
Though telemedicine in mental health offers immense advantages, its implementation is not so easy. There are many challenges in telemedicine for mental health implementation that require strategic attention to overcome. Understanding these complexities is vital for optimizing virtual care delivery:
Persistent Digital Divide
Telemedicine may seem to eliminate the distance between healthcare providers and patients, but it may unintentionally establish new disparities. The major issue is providing a fair opportunity to people who do not have a stable internet connection, appropriate digital devices, or sufficient digital skills. Even though care is available virtually, certain vulnerable populations can become unable to receive essential services due to this digital exclusion.
Solution
Telemedicine solutions should be prioritized to use low-bandwidth conditions, as well as work with lower-end devices, and, where possible, be allowed to work offline. The UX based on lightweight, mobile-first, and adaptive streaming features will provide care delivery access under suboptimal technology conditions. When a platform is bolstered in terms of resilience, it can simply be monetized as expanded market outreach and inclusivity in nature–spared of cost-budgeting exercises.
Technical Glitches and Connectivity Issues
Stable technology is key to the successful implementation of telemental health. The technical issues like lost video or audio/video impairments, platform crashes may violate the flow of the therapeutic process, create frustration among patients and providers, and may adversely affect the efficacy and continuity of care.
Solution
Optimization of the whole tech stack before the issue happens is paramount. Consider pre-call diagnostics, adaptive bitrate streaming, or AI-based quality checks. Create a backend that predicts and mitigates performance glitches, guarantees a better success rate of sessions, and minimizes abandonments. This stability is beneficial not only to the businesses, but it is also a way of safeguarding user loyalty and reducing support expenses.
Interstate Licensing and Regulatory Complexities
One of the major obstacles to the application of telemedicine in mental health is the difficulty in managing state-to-state licensing legislation. Most providers will have to be licensed within the state where the patient is physically present. This limits their possibilities to provide the services interstate and also limits the expandability of specialized care, even though this platform is virtual.
Solution
Companies should integrate built-in provider credentialing modules and compliance-aware routing systems to match users with legally eligible professionals. Where applicable, building strategic partnerships with multi-state licensed networks or national registries can drastically accelerate coverage expansion. Compliance isn’t a bottleneck; it’s a competitive edge when architected into the platform from day one.
Limitations in Crisis Intervention and Acute Care
Although applicable to long-term treatment and mild-to-moderate disorders, there are certain limitations of telemental health as a method of acute psychiatric crisis management or contexts where immediate physical assistance is a necessity. It may be much harder to assess high risk, guarantee safety to the patient in the emergence of an unfamiliar ailment, and organize a quick emergency response when a virtual setting is used rather than the real one.
Solution
Design platforms using hybrid care frameworks that integrate telehealth with on-ground emergency networks and local mental health resources. Real-time escalation protocols, geolocation-assisted alerts, and behavioral analytics can help identify high-risk situations before they escalate. Embedding these safeguards strengthens platform credibility, aligns with duty-of-care standards, and reassures both users and partners that the system is prepared and reliable.
Building Therapeutic Rapport and Non-Verbal Cues
Not to mention that deep therapeutic rapport may prove harder to build via a screen in some cases and with some patients and therapists. The lack of expressive non-verbal messages (body language, presence) and factors of geographical location when contacting can potentially harm the opportunity of a therapist to evaluate the entire emotional state of a patient or can create discomfort in a patient who wants to be vulnerable and feel a full connection with the therapist.
Solution
Supplementing virtual sessions with AI for sentiment analysis, mood monitoring, and optional video-recorded reflections can give the providers more hints about the well-being of the patient. At the frontend, such functions as eye contact synchronization, natural lighting, and environment calibration are used to simulate the in-person environment. When the interface is engineered with rapport, there is improved engagement and value of sessions.
Bonus Read: Best Mental Health App Features for 2026
The Future of Telemedicine in Mental Health: A Vision for Integrated Care
Telemedicine in mental health is entering a new phase. It’s no longer just a backup for in-person visits. It’s gradually turning into a system that follows patients through their everyday lives, offering support exactly when they need it rather than only when a slot is available. Understanding these shifts is not merely about adopting new tools, but about strategically positioning your organizations to deliver scalable, efficient, and deeply personalized care.
Continuous Support Instead of Weekly Check-ins
Virtual care is shifting from scheduled appointments to ongoing touchpoints where:
- Patients can reach out between sessions.
- Clinicians get a clearer picture of day-to-day emotional patterns.
- Support becomes more responsive, especially for individuals with fluctuating symptoms.
AI-Powered Early Intervention
The next generation of telemedicine will heavily rely on AI to detect subtle signals like changes in sleep, social withdrawal, or irregular routines to prevent a crisis before it turns severe or unmanageable. AI-driven analytics can surface these patterns instantly, enabling clinicians to intervene early and prevent escalation rather than reacting to breakdowns.
Also Read: The Impact of AI in Healthcare Industry
Data-Led Early Intervention
The next wave will rely heavily on subtle signals that often go unnoticed such as disturbed sleep, sudden withdrawal, or irregular routines often appear before a crisis. Telemedicine platforms will surface these patterns so clinicians can intervene early. The goal? Prevent escalation rather than manage breakdowns.
Collaborative Care Across Locations
Mental health care is becoming more team-based, and telemedicine makes that easier. Here is how:
- Therapists, psychiatrists, and coaches can work from the same digital record.
- Patients avoid repeating their story at every touchpoint.
- Rural and underserved areas gain regular access to specialists.
Blended Community Support
Future models of telemedicine in mental health will also weave in human networks around the patient.
- Moderated peer groups
- Family education sessions
- Local crisis support paired with virtual follow-ups
This mix brings structure, belonging, and continuity to the recovery journey.
A More Human Form of Digital Care
The real shift isn’t the technology itself. It’s how care becomes:
- More consistent
- More adaptive
- More accessible
Mental health telemedicine isn’t replacing human connection; it’s giving people more ways to keep that connection alive, even when life gets complicated.
Wearables and Remote Monitoring for Proactive Care
The proliferation of smart wearables in healthcare and connected health devices will enable a shift from reactive treatment to proactive intervention. These devices can passively collect real-time physiological and behavioral data, such as sleep patterns, heart rate variability, activity levels, and even voice tone, which can be indicative of mental health states.
For instance, Appinventiv developed DiabeticU, a diabetic management app that demonstrates how wearable and remote monitoring data can be integrated into a health platform. The app collects real-time metrics from users to support proactive care and personalized interventions.
Hybrid Care Models (In-person + Virtual)
A careful combination of virtual and in-person care is probably the most successful future model of telemedicine. This intermediary solution is based on the understanding that telemedicine offers clear advantages: it is convenient, accessible, and allows for continuous care.
However, certain aspects of mental health treatment such as initial assessments, crisis interventions, or specific therapeutic modalities, still benefit from in-person communication. This flexible approach enables personalized care based on the needs and preferences of the respective patients to maximize care by engaging them.
As an illustration, a patient may arrange regular virtual meetings with a therapist but visit in person occasionally to have a certain assessment or group therapy. Such flexibility maximizes the use of available resources and enhances patient satisfaction and delivers the appropriate level of care, at the most appropriate time, wherever you are.
Also Read: Healthcare Software Product Development – A Complete Guide
While competitors react to patient needs, create platforms that anticipate them with real-time AI monitoring.
Leverage Appinventiv’s Expertise for Mental Health Telemedicine Development
Healthcare is evolving at lightning speed. To keep pace with the changing healthcare trend, organizations need a trusted telemedicine app development company that can deliver scalable, secure, and patient-centered digital solutions that are fully compliant with industry regulations like HIPAA and GDPR.
This is where we come in. Our team of 1600+ tech experts helps healthcare providers, payers, and digital health platforms leverage telemedicine for mental health to improve outcomes, streamline operations, and enhance patient experiences. In our 10+ years of experience in the HealthTech industry, we have supported 450+ healthcare clients with more than 500 digital health platforms delivered.
Health-e-People, Soniphi and YouComm are some of our notable projects in healthcare, where we helped design and deploy solutions that transform patient engagement and operational efficiency.
What Business Impact We Deliver
- 300+ connected medical devices integrated
- 99.90% uptime for Critical Systems
- 45% operational efficiency gains
- 90%+ clinical data accuracy achieved
- 95% patient satisfaction in deployed apps
Recognized for Excellence
Our expertise in telemedicine software development for mental health professionals and 35+ other industries has earned us several recognitions, such as
- Leader in AI Product Engineering & Digital Transformation by Economic Times
These recognitions underscore our commitment to delivering excellence and innovation in healthcare technology.
Connect with our HealthTech experts to discuss how we can transform your healthcare delivery and patient engagement.
FAQs
Q. How does Appinventiv help in building telemedicine apps for mental health?
A. Appinventiv helps build telemedicine apps for mental health by creating customized, user-friendly solutions that ensure secure, accessible care. Our deep understanding of both telemedicine and mental health allows the company to focus on patient accessibility, offering features like remote therapy, real-time monitoring, and AI-powered assessments.
Our custom applications are designed with top-tier security, ensuring compliance with healthcare regulations like HIPAA. Appinventiv provides end-to-end support, ensuring telemedicine platforms evolve to meet the changing needs of mental health care.
Q. How does HIPAA impact telemedicine for mental health?
A. HIPAA (Health Insurance Portability and Accountability Act) plays a crucial role in telemedicine for mental health by ensuring the privacy and security of sensitive patient information. It mandates that mental health professionals and telemedicine platforms take stringent measures to protect patient data.
Also, compliance with HIPAA ensures that patient communications, video sessions, and records remain confidential. This facilitates trust and enables safe, secure access to mental health care services.
Failure to comply can result in significant legal and financial penalties. Therefore, telemedicine platforms must comply with HIPAA standards.
Q. Why should mental health enterprises invest in custom telemedicine app development?
A. Mental health enterprises should invest in telemedicine software development to enhance accessibility, improve patient engagement, and get secure solutions tailored to their specific needs.
Custom telemedicine apps offer personalized features, such as remote consultations, real-time monitoring, and AI-powered assessments, which ensures better patient care. Additionally, custom solutions allow for continuous evolution, adapting to emerging technologies and expanding patient requirements, thus improving long-term operational efficiency and patient satisfaction.
Q. How much does it cost to develop a telemedicine app for mental health?
A. Depending on a number of factors, such as the complexity of the features, the choice of platforms (iOS / Android), the location of the team doing the development, and the customization level, the cost of developing the telemedicine app for mental health can vary.
On average, a simple telemedicine application development can cost between $30,000 and $200,000.
But when it comes to such advanced functionality as AI-based assessments, real-time monitoring, and third-party integrations, the price may range from 200,000 to 400,000 or even higher. It is also costly in terms of regular maintenance, security updates, and HIPAA compliance.
Q. How is telemedicine effective for mental health?
A. Mental health can greatly benefit the usage of telemedicine since it facilitates the advantages of accessibility, convenience, and privacy for patients. It helps overcome geographical barriers, and residents of remote or underserved regions can receive therapy and counseling. The flexibility of time is another advantage of telemedicine patients can easily integrate mental health care in life.
Also, it facilitates anonymity, which can positively affect the stigma and make people seek care. Telemedicine improves the entire experience of mental health care, making it more secure, confidential, and keeping up with principles such as HIPAA with real-time consultations, follow-ups, etc.
Q. What are the types of telemedicine for mental health?
A. Telemedicine for mental health includes:
- Video Conferencing
- Phone Consultations
- Text-based Therapy
- Online Support Groups
- Remote Monitoring
- Self-help Apps
Q. How can AI and machine learning enhance mental health treatment through telemedicine?
A. AI and machine learning enhance mental health treatment through telemedicine by offering personalized care, predictive analytics, and real-time monitoring.
AI helps create customized treatment plans, predicts mental health risks, and analyzes patient behaviors for deeper insights. Machine learning can improve diagnostics and assist therapists in tracking progress. Additionally, AI-powered chatbots provide 24/7 support, offering immediate help and coping strategies, making mental health care more accessible and efficient.
Q. What are the key features of telemedicine for mental health?
A. Telemedicine for mental health features video consultations for real-time therapy, secure messaging for confidential communication, and easy appointment scheduling with reminders. It includes remote monitoring of symptoms and medication adherence, alongside AI tools for personalized care plans and predictive analytics.
Online support groups provide peer connections, while data security ensures HIPAA compliance, safeguarding patient information. These features ensure accessible, flexible, and secure mental health care.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How to Build a Custom Pediatric EMR and EHR System?
Key takeaways: Clinical Precision: Custom systems accommodate pediatric-specific data points like percentile curves and weight-based longitudinal dosing. Interoperability: Seamless data exchange via HL7 FHIR ensures your practice stays connected to pharmacies, labs, and state registries. Regulatory Resilience: Built-in compliance with HIPAA, HITECH, and MACRA/MIPS reduces legal friction. Enhanced Engagement: Parent portals reduce administrative overhead by…

Change Management in Healthcare: Principles, Processes, and Models
Key Takeaways Change in healthcare fails quietly when ownership, workflow alignment, and follow-through are missing. Successful change management in healthcare focuses on adoption, not just system implementation. Clinical workflows and workforce capacity determine whether transformation sticks or stalls. Governance, clear accountability, and post-go-live support matter more than the model used. Sustainable healthcare transformation depends on…
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…