- Major Pain Points US Pharmacies Face Today
- What Is “Intelligent” Pharmacy Automation Today?
- Types of Pharmacy Automation Solutions
- 1. Robotic Dispensing Systems
- 2. Automated Packaging and Unit-Dose Systems
- 3. Automated Dispensing Cabinets and Smart Storage
- 4. Inventory Management and Analytics Platforms
- 5. Workflow Automation and Middleware Systems
- 6. Telepharmacy and Remote Verification Tools
- Business Benefits: How Intelligent Pharmacy Automation Drives ROI
- 1. Less Strain on Staff and Lower Labor Spend
- 2. Fewer Errors and Smoother Compliance
- 3. Better Control of Inventory and Waste
- 4. More Throughput Without More Staff
- 5. Closed-Loop Medication Safety
- 6. 340B Program Optimization
- 7. Institutional Resilience
- 8. Support for New Service Lines
- 9. Better Patient and Provider Experience
- Key ROI Levers and How to Calculate ROI
- Direct ROI Levers
- Indirect ROI Levers
- Cost Areas to Plan For
- How to Calculate ROI
- When to Expect Payback
- Challenges of Pharmacy Automation and How Enterprises Can Address Them
- 1. Complex Integrations With PMS, EHR, and ERP Systems
- 2. High Upfront Costs and Budget Questions
- 3. Change Management and Staff Adoption
- 4. Technical Interoperability
- 5. Downtime and Continuity Concerns
- 6. Controlled-Substance Compliance and Security
- 7. Cybersecurity in "Connected" Hardware
- 8. Vendor Dependence and SLA Reliability
- Key Features of an Intelligent Pharmacy Automation System
- 1. Steady and Accurate Dispensing Performance
- 2. Flexible Packaging and Dose Preparation
- 3. Real-Time Inventory Visibility
- 4. Clear Workflow Routing and Exception Handling
- 5. Built-In Safety and Compliance Controls
- 6. Support for Integration Across Core Systems
- 7. Performance, Security, and Scalability Standards
- Pharmacy Automation Implementation Steps: A Practical Enterprise Roadmap
- 1. Start With Discovery and a Clear Baseline
- 2. Define Pilot Scope and Objectives
- 3. Plan and Execute System Integrations
- 4. Prepare the Site and Update Standard Operating Procedures
- 5. Train Staff and Run Parallel Workflows
- 6. Go Live in Phases and Monitor Early Results
- 7. Scale to Additional Sites and Expand Capabilities
- 8. Continuously Optimize and Evolve the System
- Real-World Outcomes from Pharmacy Automation
- Capsa Healthcare – Unit-of-Use Automation ROI
- Capsa Healthcare – Will-Call Automation in Retail and Outpatient
- Noritsu – Central Fill and Upgrade Outcomes
- Omnicell – Trust-Wide Rollout and Safety Impact
- Hospital Studies – Error and Efficiency Improvements
- What is The Future of Pharmacy Automation
- 1. Smarter Inventory Forecasting and Automated Replenishment
- 2. More Accurate Verification and Exception Detection
- 3. Robotics Designed for Flexible, Multi-Step Tasks
- 4. Growth in Remote Dispensing and Telepharmacy Models
- 5. Deeper Interoperability Across the Care Ecosystem
- 6. Larger Central-Fill and Hub-and-Spoke Operations
- Why Appinventiv for Intelligent Pharmacy Automation Systems
- What We Bring to Enterprise Pharmacy Teams
- How This Supports Your Automation Goals
- Conclusion
- FAQs
Key takeaways:
- Intelligent pharmacy automation systems reduce manual work. They also help teams improve accuracy and handle daily tasks in a steady, predictable way.
- The main financial gains come from lower labor costs, better inventory control, fewer error-related expenses, and new service lines that support steady revenue.
- High-volume sites usually see quicker payback. Many reach a clear return within 12–24 months when they begin with a pilot and track the right baseline metrics.
- Strong results depend on more than the machines. Teams need clean integrations, stable workflows, and a data layer that supports daily operations.
- A phased rollout works best. Start small, scale once the system is stable, and refine processes as volume grows. This approach provides leadership with clear proof of impact and a solid case for broader investment.
US pharmacies face rising pressure on three fronts: cost, volume, and safety.
Prescription demand is growing. Staff are stretched thin. Margins are under pressure.
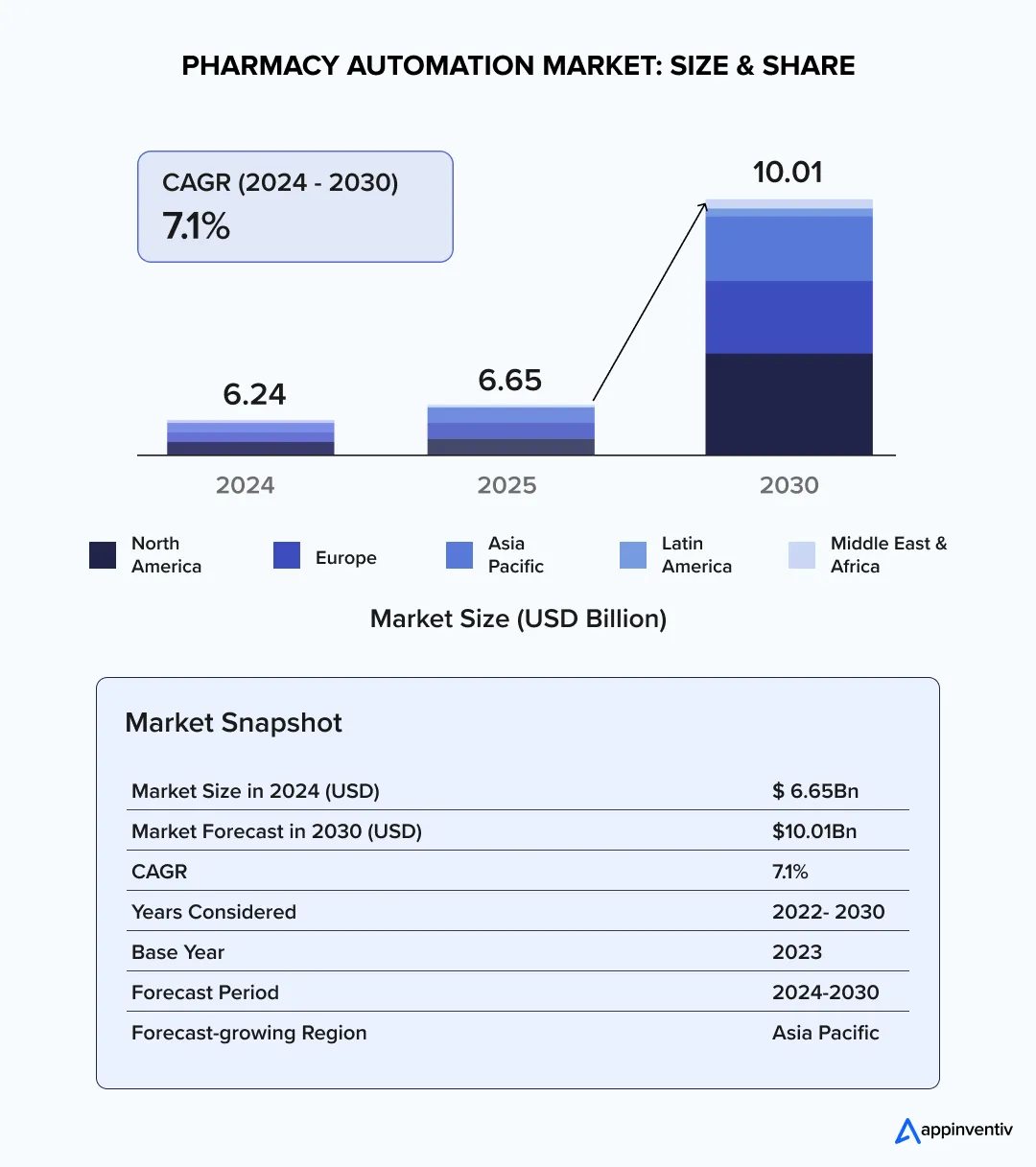
The pharmacy automation market is expanding to meet that pressure. According to industry forecasts, the global market is set to reach roughly $10 billion by 2030, and North America accounted for about 48% of revenue in 2024.
At the same time, pharmacies report high hiring demand and ongoing workforce stress. Job postings for pharmacists and technicians remain elevated. Pharmacy teams spend substantial time managing shortages and operational gaps.
For enterprise leaders, the question is simple. How do we turn automation into a predictable business outcome? CEOs, COOs, and CIOs want clear ROI. They want systems that scale. They want clean integrations with EHR and PMS.
This article focuses on that need. It shows where intelligent pharmacy automation systems deliver value. It outlines the business levers to measure ROI. And it gives a practical, phased approach for pharmacy automation system development that reduces risk and proves impact.
Some vendors pitch plug-and-play solutions. In large health systems, that rarely happens. Integration, process change, and governance matter. Get those right, and automation pays back faster.
Automation is rising fast. Let our team guide your move toward scalable, future-ready systems.
Major Pain Points US Pharmacies Face Today
Pharmacies across the US face growing operational pressure. These issues show up in day-to-day work and in long-term strategy decisions.
- Ongoing staff shortages and rising labor costs
Most pharmacies run with fewer technicians than they need. This raises overtime costs and slows routine tasks. It also limits how far teams can go with manual work.
- Higher risk of medication errors
Manual dispensing increases the chance of mistakes. Each error brings compliance concerns, repeat work, and potential harm. Leaders want systems that reduce this risk in a measurable way.
- Inefficient inventory control
Many sites carry excess stock or face sudden shortages. Poor visibility leads to expiries, wasted spend, and higher carrying costs.
- Throughput bottlenecks during peak hours
During high-volume periods, queues grow fast. This affects service quality and reduces the number of prescriptions a site can process in a day.
- Systems that do not integrate well
Pharmacy management systems, EHR platforms, and dispensing hardware often work in isolation. These gaps make automation in pharmacy operations harder to scale.
- Difficulty building a clear ROI case
Leaders know automation has value. Their challenge is proving the ROI of pharmacy automation in a way that meets finance expectations.
- High administrative burden on pharmacists
Pharmacists spend a large part of their day on routine tasks. This leaves little time for clinical programs that improve patient outcomes and support new revenue streams.
What Is “Intelligent” Pharmacy Automation Today?
Intelligent pharmacy automation refers to systems that combine robotics, workflow software, and real-time data to run daily pharmacy operations with fewer manual steps. These systems are built to improve accuracy, support higher prescription volume, and reduce the operational strain that teams face today.
They bring together three core layers.
- First, automated hardware that performs repetitive tasks such as counting, filling, packaging, and storage.
- Second, a software layer that connects PMS, EHR, dispensing devices, and inventory tools to create a single workflow.
- Third, analytics and safety controls that monitor stock, track errors, and maintain compliance.
For enterprise leaders, the value lies in consistency. Intelligent systems help standardize processes across multiple sites, reduce error-related costs, and give clear visibility into throughput and inventory. They also create a stable foundation for scaling automation in pharmacy operations without disrupting care or service quality.
This foundation supports pharmacy automation system development that aligns with growth, regulatory needs, and long-term ROI goals.
Also Read: How to Develop a Pharmacy Management Software
Types of Pharmacy Automation Solutions
Pharmacy automation comes in several forms, each addressing a different part of daily operations. Most enterprises use a mix of these systems, depending on volume, service lines, and integration needs. Below are the main categories that support modern pharmacy automation strategies.
1. Robotic Dispensing Systems
These systems handle counting, filling, and vial preparation. They reduce manual steps and support consistent throughput in retail and central-fill environments. They also help cut error-related costs and support higher script volumes.
2. Automated Packaging and Unit-Dose Systems
These solutions prepare single-dose and multi-dose packs. They are used in long-term care, chronic care programs, and settings where adherence is critical. They improve accuracy and free up time for pharmacy teams.
3. Automated Dispensing Cabinets and Smart Storage
ADCs support secure storage and controlled-substance tracking. They offer real-time visibility into stock levels and improve compliance. Hospitals and specialty pharmacies use these systems to manage high-risk medications.
4. Inventory Management and Analytics Platforms
These platforms track on-hand stock, expiries, and usage patterns across one or more sites. They help teams reduce waste, prevent shortages, and optimize reorder cycles. They also support reporting needs across finance and operations.
5. Workflow Automation and Middleware Systems
These tools connect PMS, EHR, robotics, and analytics systems. They route tasks, manage exceptions, and keep operations moving without bottlenecks. This layer is essential for any enterprise aiming to scale automation in pharmacy operations.
6. Telepharmacy and Remote Verification Tools
Remote verification tools allow pharmacists to review orders without being on-site. These systems help pharmacies extend service hours, manage staffing gaps, and improve access for rural or high-volume locations.
These categories reflect the core types of pharmacy automation that most US enterprises evaluate today. They also form the building blocks for pharmacy automation system development that can grow with the organization.
Business Benefits: How Intelligent Pharmacy Automation Drives ROI
Pharmacy automation is valuable only when it improves everyday work and strengthens financial performance. The benefits of pharmacy automation below reflect what most enterprise teams see when automation becomes part of their core operations.
1. Less Strain on Staff and Lower Labor Spend
Many pharmacies run short-staffed. When routine work shifts to machines, teams spend less time on counting, filling, and repeated checks. This reduces overtime and frees pharmacists to handle clinical tasks that add more value.
2. Fewer Errors and Smoother Compliance
Most medication errors come from manual steps. Automated dispensing and barcode checks help bring those numbers down. Fewer mistakes mean less rework and fewer interruptions during audits.
3. Better Control of Inventory and Waste
Inventory is often one of the highest cost drivers. Automation helps monitor stock in real time, reduce expiries, and maintain steadier order cycles. Finance teams get clearer forecasts, and sites avoid carrying excess stock.
4. More Throughput Without More Staff
High-volume days strain manual processes. Automated systems keep prescriptions moving at a steady pace, even during peak hours. This helps multi-site enterprises scale without adding significant labor.
Many of these improvements mirror broader AI adoption in clinical settings. Our analysis of AI in healthcare outlines how data-driven tools are reducing errors and improving operational stability across care environments.
5. Closed-Loop Medication Safety
Align with national patient safety goals by ensuring every pill is tracked from the wholesaler to the bedside.
6. 340B Program Optimization
Use automated tracking to ensure compliance and maximize reimbursement capture in eligible health systems.
7. Institutional Resilience
Mitigate the “Great Resignation” of pharmacy techs by automating mundane tasks, improving staff retention rates by up to 20–30%.
8. Support for New Service Lines
Services like multi-dose packaging or long-term care support require accuracy and consistency. Automation makes these programs easier to run and expand, which helps pharmacies build new revenue streams.
9. Better Patient and Provider Experience
Shorter wait times and consistent fill accuracy improve overall satisfaction. Clinical teams also gain more time for counseling and care programs.
Automation also improves how patients interact with pharmacy services. In some settings, digital tools such as AI chatbots in healthcare help reduce wait times and support refill or follow-up requests
These benefits explain why many enterprises place automation at the center of their pharmacy strategy. It improves daily operations and builds a stronger case for long-term ROI.
Key ROI Levers and How to Calculate ROI
Pharmacy automation becomes a strong business decision when leaders can see where the financial gains come from and how fast they add up. Most enterprises track a few clear levers that show the real impact of intelligent pharmacy automation systems on cost, output, and long-term performance.
Direct ROI Levers
These benefits show up quickly and are easy to measure.
- Labor Savings
Automation removes many repetitive steps. This reduces technician hours, lowers overtime, and makes staffing more predictable.
- Lower Inventory Carrying Costs
Real-time tracking and automated stock control reduce expired items and excess stock. This helps finance teams meet budget targets.
- Fewer Error-Related Costs
Each avoided error saves time, medication, and staff hours. Automated checks reduce these incidents and the rework that follows them.
- Revenue From New Services
Central fill programs, adherence packaging, and long-term care services depend on accuracy and steady throughput. Automation supports these service lines and helps bring in steady revenue.
Indirect ROI Levers
These gains build over time and strengthen the long-term case.
- Reduced Overtime
Smoother workflows mean fewer late shifts and emergency staffing fixes.
- Higher Daily Throughput
Automated systems maintain a stable pace during peak hours. This helps sites fill more prescriptions without increasing headcount.
- Better Payer and Contract Performance
Consistent service and fewer delays support scorecards tied to reimbursement and partner agreements.
- Total Cost of Ownership (TCO)
Business leaders must account for software maintenance (15–20% of initial cost annually), HL7 interface feeds, and site-specific electrical/HVAC upgrades.
- Net Present Value (NPV)
Because pharmacy automation systems are 7–10 year assets, a 3-year ROI model is often insufficient. Enterprises should calculate NPV to account for the time value of money and rising labor inflation.
Cost Areas to Plan For
A clear ROI model includes both one-time and ongoing costs.
- Hardware and robotics
- Software licensing
- Integration and professional services
- Site preparation and electrical work
- Training and validation
- Annual support and consumables
This cost view helps leaders compare vendors and avoid surprises during pharmacy automation system development.
How to Calculate ROI
Most enterprises use two simple methods: payback period and a three-year ROI model.
Payback period
Payback (years) = Total upfront cost ÷ Annual net benefit
Three-year ROI
ROI (%) = ((Annual benefit × 3) − Upfront cost) ÷ Upfront cost × 100
Example (for illustration only):
- Upfront cost: $500,000
- Annual benefit: $350,000
- Payback: ~1.4 years
- Three-year ROI: ~110%
Actual numbers depend on script volume, wage rates, inventory size, and the type of pharmacy automation solutions deployed.
When to Expect Payback
Most high-volume sites see payback within 12–24 months. Smaller sites may need more time. But a focused pilot usually gives a clear view of the expected return. This helps executives move forward with confidence and plan a scalable automation roadmap.
Challenges of Pharmacy Automation and How Enterprises Can Address Them
Pharmacy automation brings clear operational and financial gains, but large organizations still face practical hurdles during planning and rollout. Addressing them early helps teams protect timelines, manage cost, and ensure the full ROI of pharmacy automation.
1. Complex Integrations With PMS, EHR, and ERP Systems
Most pharmacies run several systems that were not designed to work together. When automation enters the environment, gaps in data flow can slow the project.
How to address it:
- Use a strong middleware layer and plan integrations before hardware arrives.
- Map data fields, verify message standards, and test exception paths early.
- This step prevents avoidable delays during go-live.
2. High Upfront Costs and Budget Questions
Robotics, software, and site preparation require clear financial planning. Finance teams often want firm numbers before approving the project.
How to address it:
Start with a simple ROI model and a small pilot. Pilots help clarify actual throughput, labor shifts, and inventory savings, giving leadership a realistic view of payback.
3. Change Management and Staff Adoption
Automation changes workflows. Some team members may worry about the new job impact and technologies in pharma automation.
How to address it:
- Explain the new workflow early. Train teams in short cycles.
- Show how automation reduces routine tasks rather than replacing roles.
- This helps build trust and steady adoption.
4. Technical Interoperability
The HL7/FHIR hurdle. Most legacy PMS (Pharmacy Management Systems) do not speak the same language as modern robotics.
How to address it:
Implementing a standardized API gateway or middleware to translate data ensures that when a prescription is modified in the EHR, the robot stops the fill in real-time, preventing wasted inventory and potential errors.
5. Downtime and Continuity Concerns
Pharmacies need consistent uptime. A stalled robot or software issue can slow the entire line.
How to address it:
- Create backup procedures and a clear escalation path with the vendor.
- Plan a short parallel run during early rollout.
- This keeps service steady while teams adapt.
6. Controlled-Substance Compliance and Security
Tracking high-risk medications requires strict rules. Automation adds more points in the process that must meet regulatory standards.
How to address it:
- Audit every workflow step.
- Use secure access controls and real-time reporting.
- Involve compliance teams early to avoid later fixes.
7. Cybersecurity in “Connected” Hardware
Connected pharmacy hardware increases the “attack surface” of a healthcare facility, where a single unsecured dispensing robot can serve as an entry point for ransomware to move laterally into the hospital’s primary EHR and patient data networks.
How to address it:
Ensure all automated hardware follows Zero-Trust architecture, utilizing Network Segmentation to keep medical devices separate from the hospital’s primary guest or admin networks.
8. Vendor Dependence and SLA Reliability
Automation systems need regular support, updates, and spare parts. Poor service can slow operations or extend downtime.
How to address it:
- Review vendor SLAs, parts availability, and support history.
- Ask for references from similar high-volume sites.
- Clear expectations reduce long-term risk.
These challenges are manageable with strong planning. Addressing them early helps enterprises build reliable pharmacy automation systems that scale, support staff, and deliver long-term ROI.
Our healthcare software development team builds secure integrations and workflow systems that support reliable, high-volume operations.
Key Features of an Intelligent Pharmacy Automation System
A modern pharmacy automation system is more than a single machine or software tool. It is a coordinated setup that helps teams run predictable, accurate, and high-volume operations without adding strain to staff. The features below shape how well a system performs at scale and how long it remains useful as business needs grow.
1. Steady and Accurate Dispensing Performance
Dispensing machines must handle day-to-day volume without slowing down during peaks. Consistent performance reduces bottlenecks and keeps wait times under control. Accuracy also improves when counting and filling tasks follow a controlled, automated flow.
2. Flexible Packaging and Dose Preparation
Many pharmacies now support chronic care programs, long-term care partners, or central-fill services. Systems that can prepare multi-dose packs, pouches, or unit doses help teams offer these using AI in pharmacy automation without adding to manual work.
3. Real-Time Inventory Visibility
Pharmacy teams need to know what is in stock, what is expiring, and what needs to be reordered. Inventory engines that sync with dispensing and storage systems help reduce waste and control carrying costs. They also support tight coordination with supply chain teams.
4. Clear Workflow Routing and Exception Handling
Strong automation depends on a clear task flow. The system should route work to the right station, flag exceptions, and show technicians what needs manual review. This avoids confusion and helps teams maintain a steady pace.
5. Built-In Safety and Compliance Controls
Barcode checks, audit trails, and secure access controls reduce the risk of errors and support compliance with regulatory standards. These features also help during inspections, as they provide detailed records of each step.
6. Support for Integration Across Core Systems
A reliable system connects easily with PMS, EHR, dispensing cabinets, and inventory tools. The best integrations for pharmacy automation helps avoid duplicate work and keeps data consistent across locations. It also sets the foundation for multi-site automation.
7. Performance, Security, and Scalability Standards
Enterprises need systems that can grow with demand. High uptime, strong security controls, and predictable performance allow teams to expand automation without added disruption.
These features show what separates basic tools from true intelligent pharmacy automation systems. They also guide leaders during vendor evaluations and support long-term plans for pharmacy automation system development.
Pharmacy Automation Implementation Steps: A Practical Enterprise Roadmap
Implementing pharmacy automation is more than a technical project. It is an operational shift that affects staffing, workflows, compliance, and day-to-day decision-making.
A clear roadmap helps organizations move with confidence, avoid disruption, and establish a strong foundation for long-term ROI. The steps below outline how most enterprise teams move from planning to full-scale automation.
1. Start With Discovery and a Clear Baseline
Every project begins with understanding the current state. This step includes mapping workflows, studying prescription volume, and identifying bottlenecks such as long fill queues or slow inventory checks.
Key tasks in this stage:
- Measure current throughput, labor hours, and error rates.
- Review existing systems, including PMS, EHR, and any current automation tools.
- Identify high-impact use cases, such as central fill or long-term care packaging.
- Build a shared expectation of success across pharmacy, IT, and finance teams.
A strong baseline helps leadership see the early impact once automation goes live.
2. Define Pilot Scope and Objectives
A controlled pilot reduces risk. It helps teams understand how the system performs under real conditions before rolling it out across multiple locations.
During this step:
- Select one site or one process line with consistent volume.
- Set measurable goals, such as reduced fill time or fewer inventory issues.
- Determine which systems need integration during the pilot.
- Prepare training and short practice sessions for staff.
This stage produces real numbers that support internal business cases. It also helps outline the expected ROI of pharmacy automation for leadership review.
3. Plan and Execute System Integrations
Integrations create the link between robotics, workflow tools, dispensing cabinets, and clinical systems. They are often the most complex part of pharmacy automation system development.
Key integration activities:
- Map data flows between PMS, EHR, inventory platforms, and automation tools.
- Set clear rules for exceptions, order routing, and task assignments.
- Test barcode logic, user permissions, and compliance checkpoints.
- Validate system alerts and reporting dashboards.
Strong integrations reduce manual data entry and prevent delays once the system goes live.
4. Prepare the Site and Update Standard Operating Procedures
Automation may require changes to the physical setup and daily routines.
Tasks include:
- Ensuring the site has proper electrical and network connections.
- Adjusting workspace layout for safe movement of staff and equipment.
- Updating SOPs to reflect the new workflow steps.
- Establishing backup procedures for outages or unexpected downtime.
This phase keeps daily operations stable during the transition.
5. Train Staff and Run Parallel Workflows
Training helps staff gain confidence and reduces early errors. Parallel runs—where manual and automated processes work side by side for a short time—help catch gaps before full cutover.
Important elements here:
- Short, focused training sessions based on real tasks.
- Shadowing periods so staff can see how automated lines operate.
- Clear communication about how roles may shift once automation is live.
- Feedback loops so managers can fix issues quickly.
This step strengthens adoption and reduces resistance among teams.
6. Go Live in Phases and Monitor Early Results
Enterprises rarely move all sites to automation at once. A phased rollout gives room to adjust and refine.
Early go-live focus areas:
- Monitor throughput daily.
- Track exceptions and address recurring issues.
- Compare performance against the baseline measured in Step 1.
- Share results with leadership to maintain alignment.
This period often shows the first signs of reduced labor strain and improved consistency.
7. Scale to Additional Sites and Expand Capabilities
Once the pilot proves its value, teams can expand automation across the network.
During scaling:
- Standardize workflows so every site follows the same steps.
- Reuse integration templates to speed up deployment.
- Use early lessons to reduce downtime and training time.
- Expand into more advanced features such as unit-dose or adherence packaging.
Scaling multiplies the impact of automation and strengthens long-term ROI.
8. Continuously Optimize and Evolve the System
Automation is not a one-time project. As prescription volume shifts, new services launch, and compliance rules change, systems must adapt.
This step includes:
- Reviewing monthly throughput and inventory performance.
- Updating SOPs as teams gain experience.
- Scheduling regular system maintenance and software updates.
- Adding new automation modules as business needs grow.
This continuous improvement approach keeps automation aligned with enterprise goals and operational realities.
| Enterprise Readiness Checklist | |
|---|---|
| Category | Readiness Factor |
| Technical | Do we have an HL7/FHIR-compliant integration engine? |
| Security | Is the hardware SOC2 Type II compliant? |
| Operational | Are SOPs updated for “Manual Mode” during system downtime? |
| Financial | Have we audited current “shrink” and “waste” to set a baseline? |
This roadmap helps leaders build pharmacy automation systems that are stable, scalable, and ready to support future growth. It also gives teams a clear view of what to expect at each stage, reducing risk and improving long-term outcomes.
Real-World Outcomes from Pharmacy Automation
For many leaders, the question is simple: do pharmacy automation solutions pay back in real settings, not just in models? Several recent projects show clear, measured outcomes with named vendors and health systems. The examples below can sit under an “Examples of pharmacy automation” or “Real outcomes” section and support the overall ROI story.
Capsa Healthcare – Unit-of-Use Automation ROI
A recent Capsa Healthcare white paper on unit-of-use automation reports that pharmacy automation implementations are delivering 120–600% ROI, with payback periods as short as 9.6 months. These figures are based on documented results, not only projections, across healthcare organizations that moved to automated packaging for unit-of-use medications.
For an enterprise audience, this shows that the ROI of pharmacy automation can be strong when volume is high and workflows are well designed.
Capsa Healthcare – Will-Call Automation in Retail and Outpatient
In another Capsa analysis of an automated will-call system (scripClip), pharmacies reported strong labor and time savings in the “last ten feet” of the dispensing process. Key results include:
- Packaging time improved by up to 45%
- Filing time reduced by more than 90%
- Search time for filled scripts reduced by up to 73%
- Return-to-stock activities sped up by 36–78%
These gains came from better bag tracking and guided retrieval. This is a practical example of pharmacy automation system development focused on a very specific, high-friction part of the workflow.
Noritsu – Central Fill and Upgrade Outcomes
Noritsu shares ROI guidance that includes a case where a $200,000 automation investment was recouped in under two years, once tax benefits were considered.
In a separate example, Noritsu reports that Neil Medical improved medication accuracy by 25% after upgrading to newer automation equipment.
These cases show how central-fill and packaging systems can reduce errors and improve consistency while paying back within a timeframe acceptable to most finance teams.
Omnicell – Trust-Wide Rollout and Safety Impact
Northumberland Tyne and Wear NHS Foundation Trust (UK) uses Omnicell automated dispensing cabinets and a VBM 200F adherence pack system. The Trust reports that automating monitored dosage systems reduced the frequency of errors, cut the time needed to dispense, and reduced the number of staff required for these tasks. Freed staff then moved into more clinical roles.
While this is outside the US, it is a strong reference point for hospital leaders looking at pharmacy automation systems in inpatient and mental health settings.
Hospital Studies – Error and Efficiency Improvements
Recent clinical and operational studies also show clear benefits:
- A 2025 systematic review found that pharmacy automation systems in hospital settings reduced medication errors, dispensing time, and refill errors, while also lowering labor cost.
- A quality-improvement project on inpatient dispensing reported better stock control, lower costs, and faster turnaround times once an automated dispensing solution was in place.
- A study on automated dispensing cabinets (ADCs) in intensive care units showed reduced medication errors across prescribing, dispensing, and administration stages.
These examples give decision-makers concrete evidence that well-planned pharmacy automation implementation steps can reduce risk and improve both clinical and financial outcomes.
Together, these cases provide strong external proof that intelligent pharmacy automation systems are not only a technical upgrade. They are a practical path to measurable ROI, better safety, and more sustainable operations—especially in high-volume enterprise environments.
What is The Future of Pharmacy Automation
Pharmacy automation is moving from task-based tools to connected, data-driven systems that support enterprise-wide care delivery. The next wave of technology will focus on speed, accuracy, and real-time decision support. For pharmacy leaders planning long-term strategies, the trends below signal where the industry is heading.
1. Smarter Inventory Forecasting and Automated Replenishment
Pharmacies are shifting toward systems that predict demand, monitor stock movement, and adjust orders without manual checks. This helps reduce waste, control purchasing, and support a steadier supply across multiple sites.
2. More Accurate Verification and Exception Detection
Automation will play a larger role in spotting irregular orders, unsafe combinations, or unusual patterns. These tools help pharmacists catch issues early and reduce clinical risk, especially in high-volume settings.
3. Robotics Designed for Flexible, Multi-Step Tasks
Future systems will move beyond fixed-path robots. New equipment will support different package types, changes in layout, and more complex handling tasks. This flexibility helps enterprises adapt to shifting business needs.
4. Growth in Remote Dispensing and Telepharmacy Models
Many health systems want extended service hours without adding on-site staff. Remote review and telepharmacy tools make this possible. They also support rural locations and overflow sites where staffing is harder.
As remote dispensing grows, many pharmacies are adding telepharmacy models to support extended hours and rural sites. Our guide on telepharmacy software development explains how these systems support safe remote verification and consistent service.
5. Deeper Interoperability Across the Care Ecosystem
Pharmacy systems will connect more closely with EHRs, dispensing cabinets, supply chain platforms, and patient management tools. This supports closed-loop medication workflows and reduces manual handoffs between teams.
6. Larger Central-Fill and Hub-and-Spoke Operations
Centralized fulfillment continues to grow, especially for high-volume chains and health systems. Automation supports predictable output, faster turnarounds, and better cost control across large networks.
Pharmacies that prepare for these shifts now will be better positioned to scale operations, manage rising script volumes, and support new care services. These trends also reinforce the long-term value of intelligent pharmacy automation systems for enterprise environments.
As systems evolve, pharmacies will also see new models for forecasting and anomaly detection. Our insights on generative AI in healthcare highlight how advanced models are shaping future automation.
Why Appinventiv for Intelligent Pharmacy Automation Systems
Enterprises investing in pharmacy automation want a partner who understands healthcare operations, system behavior, and the realities of multi-site deployments. Appinventiv combines RPA development services with healthcare software expertise to deliver automation solutions that work. We have deep experience deploying robotic process automation across regulated industries—from prescription processing and inventory management to claims handling and compliance reporting—building systems that consistently improve performance at scale.
Our work in healthcare is driven by engineering discipline and measurable outcomes. Our AI development services help organizations plan automation programs, build the workflow and data layers around their systems, and integrate those solutions into existing EHR, PMS, and supply chain environments. This approach reduces risk during rollout and supports long-term ROI.
Appinventiv doesn’t just build solutions; we build regulated interoperability layers. We specialize in navigating 21 CFR Part 11 compliance and DSCSA (Drug Supply Chain Security Act) traceability, ensuring your automation investment is future-proofed against evolving FDA requirements.
What We Bring to Enterprise Pharmacy Teams
- A team of 1,600+ technologists experienced in engineering complex, high-volume healthcare solutions.
- Experience delivering 3,000+ digital and operational systems across industries, including large healthcare networks.
- More than 500 legacy process transformations, helping organizations replace outdated systems without disrupting daily operations.
- Proven capabilities in AI-driven analytics, workflow engines, integration layers, and compliance-focused architectures. It is essential for intelligent pharmacy automation systems.
- Recognition from industry bodies, including Deloitte Technology Fast 50, Clutch Global Award 2025, and the ET Leadership Excellence Award. These awards reflect our consistency in complex delivery environments.
How This Supports Your Automation Goals
- Clear assessment and planning for pharmacy automation system development.
- Integration frameworks that help PMS, EHR, ADCs, and dispensing systems work together reliably.
- Operational workflows designed to reduce errors, maintain uptime, and support multi-site scaling.
- Support models that evolve with your automation roadmap, from pilot to full network rollout.
Our role is to help pharmacy leaders build systems that run smoothly, improve daily throughput, and support long-term growth. We focus on outcomes that matter—steady operations, safer dispensing, and a predictable return on investment.
Our healthcare development architects will review your data flow and provide a gap analysis for your implementation
Conclusion
Pharmacy automation has moved from a helpful upgrade to a core part of how modern pharmacies operate. Rising volume, staffing pressure, and the need for safer, more efficient workflows make intelligent systems a practical choice for enterprises. These solutions reduce manual strain, improve accuracy, and create the consistency needed for steady growth.
The strongest returns come when automation is introduced with clear goals, clean integrations, and a phased rollout. A focused pilot helps teams measure early gains, validate assumptions, and build a roadmap that fits their operations. From there, automation can support higher throughput, stronger inventory control, and new service lines.
For leaders planning the next stage of their pharmacy strategy, this is the right time to evaluate how these systems fit into long-term goals. With the right approach and team, pharmacy automation becomes a predictable investment that strengthens both daily operations and the broader business. Connect with our experts to discuss your project needs.
FAQs
Q. How do you choose a pharmacy automation solution?
A. Start with your current needs and long-term goals. Review daily volume, staffing gaps, and where errors or delays occur. Look for systems that integrate well with your PMS, EHR, and inventory tools, as this reduces manual work. Check whether the solution supports your service lines, such as central fill or unit-dose packaging. Evaluate uptime, support models, and the vendor’s track record with similar enterprise sites. A small pilot can help confirm fit before you scale.
Q. What is the cost of pharmacy automation?
A. The cost of implementing pharmacy automation varies by the type of system and the scale of your operations. Most projects include spending on hardware, software, integrations, site preparation, training, and yearly support. Smaller setups may start in the low six-figure range. Larger automation lines or central-fill setups can run higher due to more equipment and complex integrations. A clear ROI model, based on labor savings and inventory improvements, helps estimate the payback period.
Q. What are pharmacy automation systems?
A. Pharmacy automation systems are tools that help pharmacies perform routine tasks with less manual work. These systems include robotic dispensers, packaging units, automated storage, workflow tools, and inventory platforms. They support accuracy, speed, and safer operations. In enterprise settings, they also help standardize processes across sites and improve the overall ROI of pharmacy automation.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How AI Chatbots for eCommerce are Driving 3x More Sales in 2026
Key takeaways: AI chatbots for eCommerce have a direct impact on revenue. When aligned with buying intent, they lift conversions, increase order value, and drive repeat purchases. The strongest impact comes from personalization and guided selling, helping shoppers decide faster and buy with greater confidence. Abandoned cart recovery is a major revenue driver in 2026.…
AI-Powered Booking Optimization for Beauty Salons in Dubai: Costs, ROI & App Development
Key Highlights AI booking optimization improves utilization, reduces no-shows, and stabilizes predictable salon revenue streams. Enterprise salon platforms enable centralized scheduling, customer insights, and scalable multi-location operational control. AI-enabled booking platforms can be designed to align with UAE data protection regulations and secure payment standards. Predictive scheduling and personalization increase customer retention while significantly reducing…

Data Mesh vs Data Fabric: Which Architecture Actually Scales With Business Growth?
Key takeaways: Data Mesh supports decentralized scaling, while Data Fabric improves integration efficiency across growing business environments. Hybrid architectures often deliver flexibility, governance, and scalability without forcing premature enterprise-level complexity decisions. Early architecture choices directly influence reporting accuracy, experimentation speed, and future AI readiness across teams. Phased adoption reduces risk, controls costs, and allows architecture…