- What is Synthetic Data in Healthcare?
- Types of Healthcare Synthetic Data
- Why Does Healthcare Need Synthetic Data?
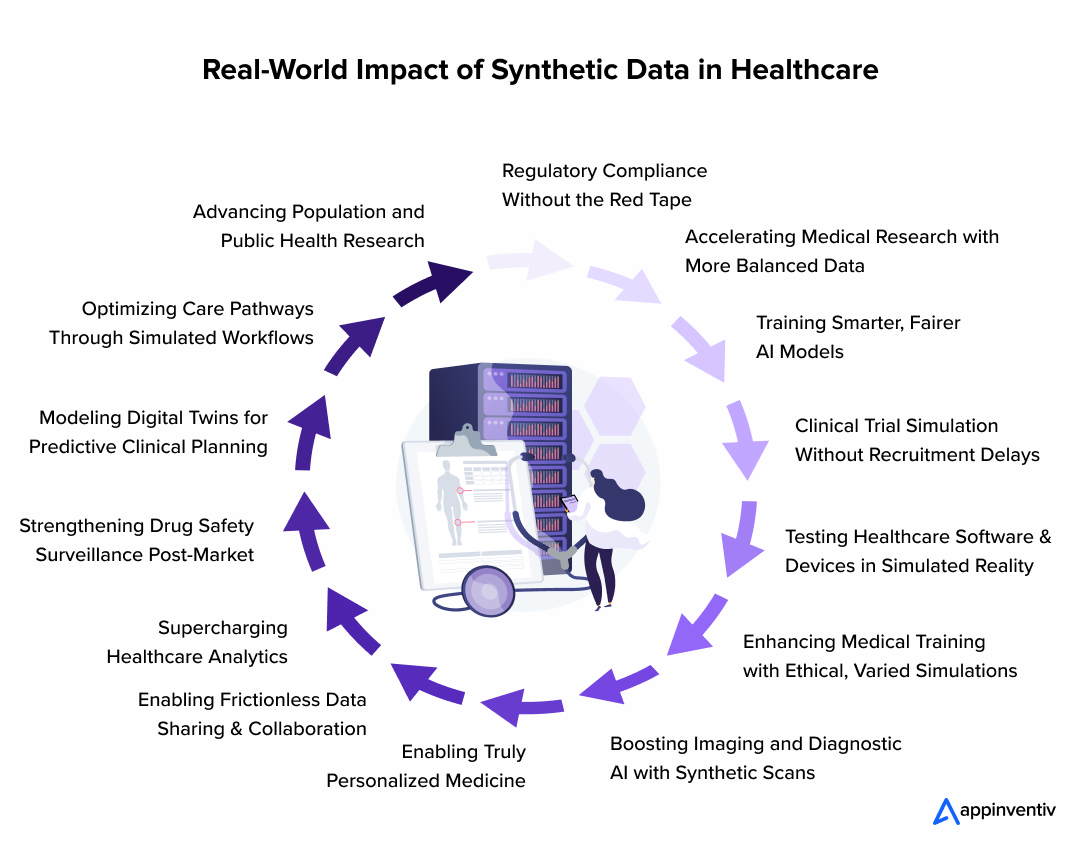
- How Synthetic Data Is Transforming Healthcare from Research to Real-World Impact
- Regulatory Compliance Without the Red Tape
- Accelerating Medical Research with More Balanced Data
- Training Smarter, Fairer AI Models
- Clinical Trial Simulation Without Recruitment Delays
- Testing Healthcare Software and Devices in Simulated Reality
- Enhancing Medical Training with Ethical, Varied Simulations
- Boosting Imaging and Diagnostic AI with Synthetic Scans
- Enabling Truly Personalized Medicine
- Enabling Frictionless Data Sharing & Collaboration
- Supercharging Healthcare Analytics
- Strengthening Drug Safety Surveillance Post-Market
- Modeling Digital Twins for Predictive Clinical Planning
- Optimizing Care Pathways Through Simulated Workflows
- Advancing Population and Public Health Research
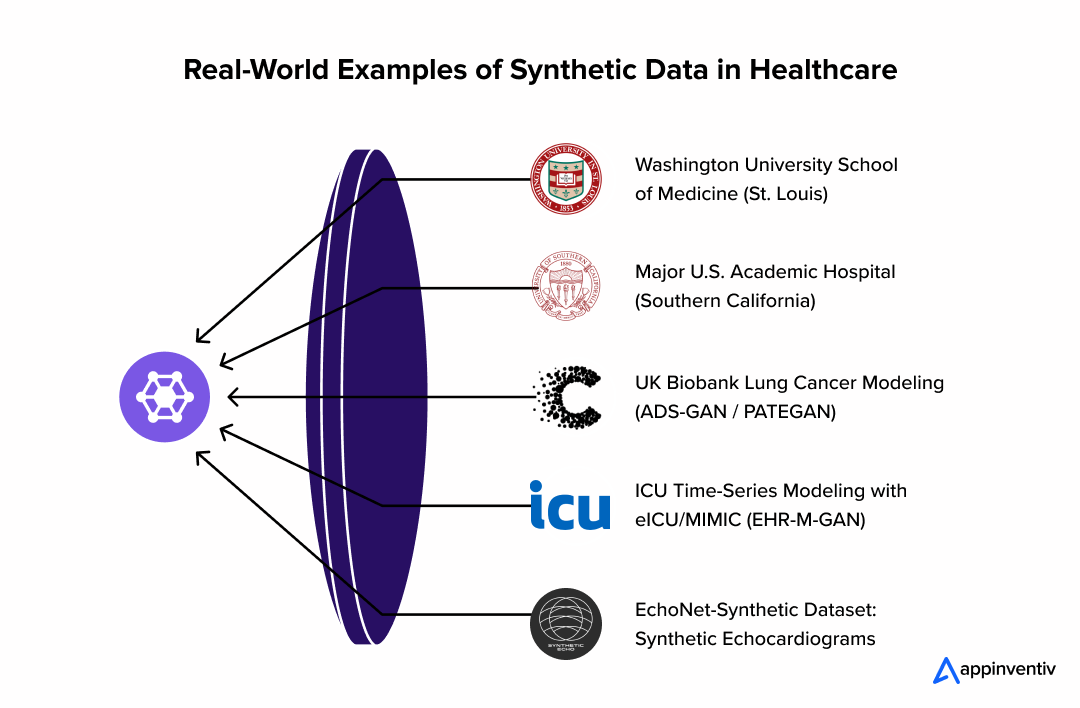
- Real‑World Use Cases of Synthetic Data Healthcare
- 1. Washington University School of Medicine (St. Louis)
- 2. Major U.S. Academic Hospital (Southern California)
- 3. UK Biobank Lung Cancer Modeling (ADS-GAN / PATEGAN)
- 4. ICU Time-Series Modeling with eICU/MIMIC (EHR-M-GAN)
- 5. EchoNet-Synthetic Dataset: Synthetic Echocardiograms
- Notable Examples from Other Institutions
- How to Create Synthetic Data for Healthcare Applications?
- Cost of Synthetic Healthcare Data
- Challenges of Using Synthetic Data in Medicine
- Building Smarter Healthcare Solutions with Synthetic Data and Custom Development
- Synthetic Data is no Longer Optional - It’s Inevitable
- FAQs
Key takeaways:
- Synthetic data mimics real patient data without exposing identities, ensuring privacy compliance.
- It bridges data gaps, speeding up AI training and research, especially for rare conditions.
- Synthetic data is cost-effective and quicker to generate compared to real patient data.
- It helps create diverse datasets, improving fairness in healthcare AI models.
- From AI diagnostics to clinical trials, synthetic data drives key healthcare advancements.
The healthcare industry runs on data – but accessing it is a minefield. Privacy regulations, fragmented systems, and patient consent barriers often stand in the way of innovation. That’s where synthetic data in healthcare is beginning to change the equation.
Generated through algorithms that mirror real-world clinical patterns without revealing any actual patient identities, synthetic healthcare data has moved from an academic concept to a powerful enabler of transformation. Whether it’s testing AI diagnostics, accelerating drug discovery, or training machine learning models without breaching compliance, synthetic data for healthcare is solving the twin problems of data scarcity and data sensitivity at scale.
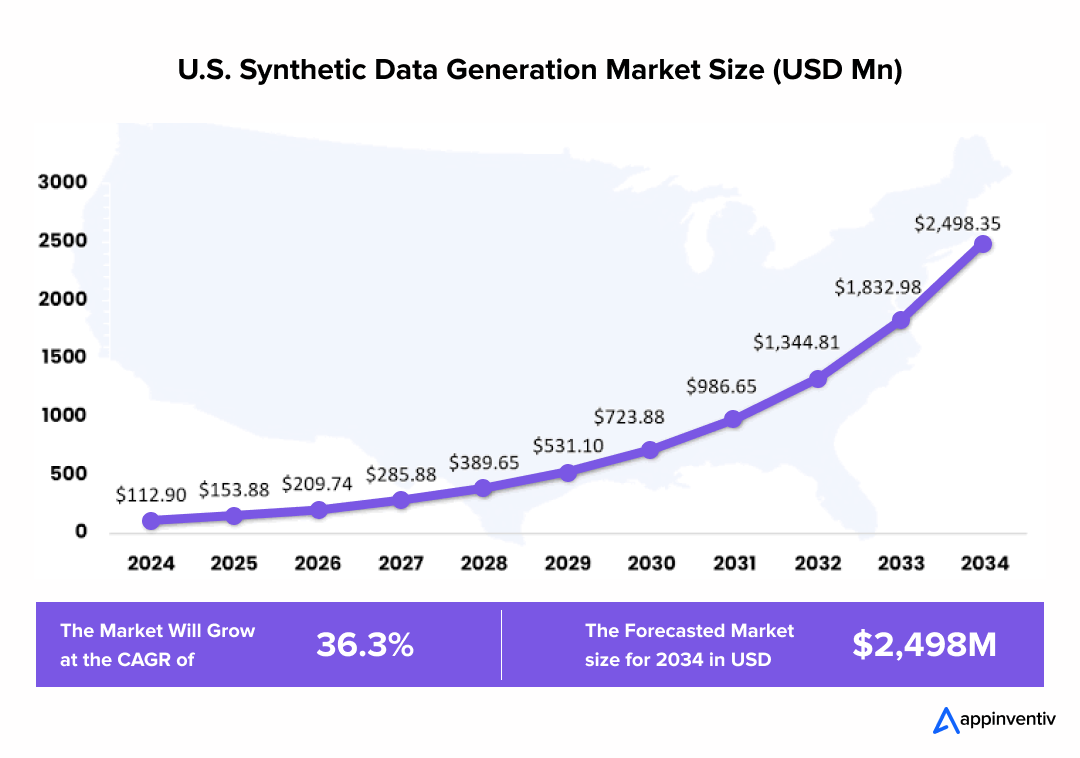
As the cost of synthetic healthcare data drops and tooling improves, hospitals, med-tech startups, and research labs are increasingly integrating synthetic patient data into their core workflows. This isn’t just about anonymization – it’s about creating highly realistic datasets that fuel accurate, ethical, and bias-free healthcare AI systems.
In this article, we explore 10+ real-world applications of synthetic data in healthcare – showing how it’s powering clinical decision support, automating documentation, building digital twins, and much more. We’ll also touch upon the types of healthcare synthetic data, the process of synthetic data for healthcare, its benefits, and the current challenges of using synthetic data in medicine. By the end, you’ll also see why AI synthetic data healthcare is not a substitute – but a strategic foundation – for the future of smart, safe, and scalable digital health systems.
Start your synthetic data journey with us!
What is Synthetic Data in Healthcare?
Synthetic data in healthcare is an approach to use artificially generated data to mimic the statistical properties and structure of real patient data – without ever exposing any actual individual’s identity or their health records. What is important to note is that it is not anonymized; it’s entirely synthetic, created with algorithms, simulations, or generative models like GANs and LLMs.
A Simple Example
Imagine there is a hospital that wants to train an AI model for detecting the early signs of stroke from MRI scans. Now because of the strict patient confidentiality laws, they can not share actual MRI data with third-party developers. Instead, they generate medical synthetic data – hundreds of lifelike but entirely artificial MRI images that reflect the same patterns found in real stroke cases. These synthetic images are built to be statistically accurate, clinically useful, and 100% free of the real patient information.
This enables a hospital to build and test AI tools safely, without having to wait for data-sharing agreements or risk any compliance violations.
Types of Healthcare Synthetic Data
There are a range of different types of healthcare synthetic data, each built to serve a specific use case in clinical research, diagnostics, and AI development. Here are the most common ones:
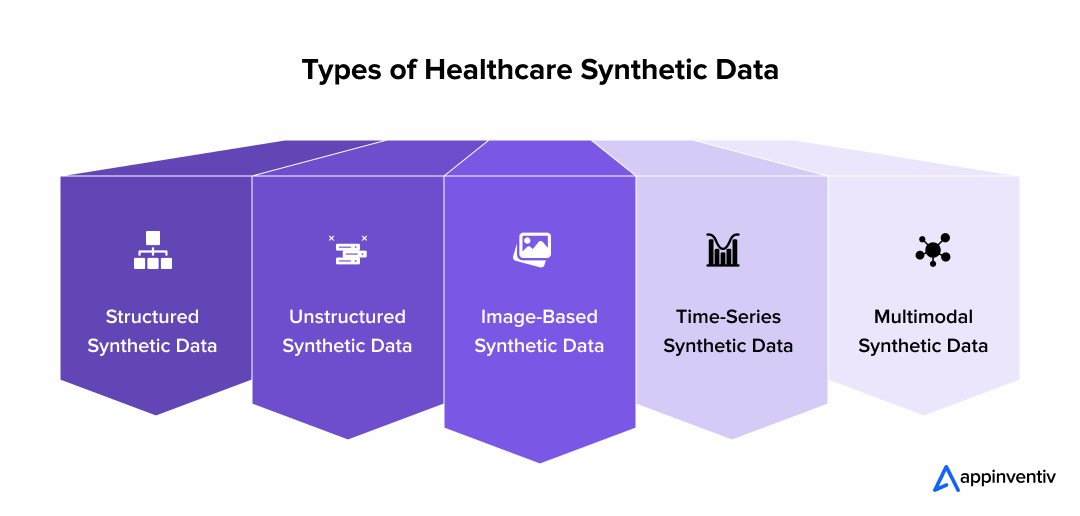
Structured Synthetic Data
Tabular data which mimics electronic health records, lab test results, or hospital billing codes. They are best for predictive modelling and workflow automation.
Unstructured Synthetic Data
Clinical notes, discharge summaries, or radiology reports generated using large language models – often used to train NLP systems in a privacy-safe way.
Image-Based Synthetic Data
Artificial MRI, CT, or X-ray images created to copy rare diseases or simply enrich the training datasets in computer vision models.
Time-Series Synthetic Data
Vital signs, ECG patterns, or wearable data streams that replicate the temporal patient signals to then be used in monitoring, forecasting, or anomaly detection.
Multimodal Synthetic Data
Combines two or more types above – for example, generating patient records with matching clinical notes and diagnostic images – to support AI synthetic data healthcare applications with greater contextual realism.
Why Does Healthcare Need Synthetic Data?
Access to patient data has always been a bottleneck in healthcare innovation. It’s either heavily protected, incomplete, or too skewed to train robust AI systems. Synthetic data in healthcare provides a way around that – without breaching privacy or compromising research quality.
It’s not about replacing real data, the benefits of synthetic data in healthcare solely revolve around filling the gaps.
In clinical environments, building useful datasets often takes months. Cleaning, anonymising, and securing them adds to the delay. With synthetic data, the process is different. Datasets can be created on demand, modelled to reflect specific conditions or demographics, and used immediately – no sensitive information involved.
Some healthcare studies fail to move forward because the data just isn’t there. Fact is cases around rare conditions, underrepresented groups, edge cases – don’t show up frequently in any hospital records, synthetic data replicates them, giving researchers a way to test, build, and learn without waiting for real-world cases to arrive.
Privacy is another major concern. With regulations like HIPAA and GDPR in place, even sharing anonymised data between two hospitals can now raise several legal questions, synthetic data bypasses this entirely. It’s not real, and that makes it safe to share across teams, institutions, and borders.
Cost and time are also factors. Running a pilot with real-world clinical data can be expensive. Synthetic alternatives are faster to generate, cheaper to scale, and easier to adapt as research evolves. That’s why more medtech startups and AI labs are turning to it early in their development cycles.
It’s not a silver bullet. But it removes friction from processes that have traditionally been slow and restrictive – giving healthcare teams room to experiment, validate, and move faster.
How Synthetic Data Is Transforming Healthcare from Research to Real-World Impact
Patient data is not scarce – but accessing it when you need it is, traditional records are famous for being slow to collect, are filled with bias, and tightly regulated, everything that holds back innovation. Synthetic data here help recreate the statistical patterns of real-world health information without referencing the actual individuals. This enables safer experimentation, faster deployment, and a broader collaboration across healthcare systems.
Here’s how synthetic data supports meaningful outcomes across the whole healthcare journey.
Regulatory Compliance Without the Red Tape
Strict rules such as HIPAA and GDPR can slow down the development or even restrict data sharing altogether. Synthetic data solves this by offering fully anonymized datasets:
- No real identities or PHI, removing re-identification risk
- Safe for global collaborations, even where data residency laws limit access
- Enables faster regulatory sign-off thanks to test-ready data
Accelerating Medical Research with More Balanced Data
Clinical datasets often miss rare conditions or underrepresented groups, skewing insights. Synthetic data fills those gaps:
- Recreates rare disease cases or minority group patterns
- Balances datasets across key demographics such as age, gender, and geography
- Lets researchers validate all the hypotheses early, without waiting for recruitment
Training Smarter, Fairer AI Models
AI tools in healthcare must work equitably across all users – but they’re only as good as the data they’re trained on. Synthetic data offers:
- Bias mitigation, since models aren’t learning from skewed historical data
- Scenario-based training – edge cases, rare conditions, and clinical complexity
- Support for low-data or new domains, where real records are sparse
Clinical Trial Simulation Without Recruitment Delays
Running trials often depends on laborious recruitment cycles. Synthetic cohorts change the game:
- Trial designs can be pre-tested on virtual patients
- Institutional review boards (IRBs) see safer simulations, speeding approvals
- Risk of dropouts can be predicted and managed before human enrollment begins
Testing Healthcare Software and Devices in Simulated Reality
Before launching health tech, companies need robust testing – but real-patient access isn’t always possible. Synthetic data enables:
- Stress tests with extreme vitals or edge conditions
- Full QA across demographics, without touching real systems
- Independent testing for early-stage firms without hospital access
Enhancing Medical Training with Ethical, Varied Simulations
Clinical education requires exposure to many patient cases – something ethical and logistical barriers often limit. Synthetic data supports:
- Complex virtual patient histories to simulate long-term disease progression
- Cases of rare conditions to broaden training exposure
- Adaptive AI simulations that respond to student decisions in real time
Boosting Imaging and Diagnostic AI with Synthetic Scans
AI radiology models need huge numbers of labeled images – hard to come by in practice. Synthetic imaging helps by:
- Generating pathologies-rich scans (MRI, X-ray, CT) on demand
- Ensuring representation across body types, conditions, and demographics
- Improving models’ generalization by training on unseen scenarios
Enabling Truly Personalized Medicine
Delivering truly personalized treatment plans demands granular, nuanced data – often locked behind patient privacy. Synthetic approaches allow:
- Generation of detailed virtual patients with varied genetics, behaviors, or comorbidities
- Training personalization tools for drug dosing or care pathways
- Maintaining complete privacy while delivering clinical precision
Enabling Frictionless Data Sharing & Collaboration
Data silos and red tape often block innovation. Synthetic data makes sharing possible:
- Share fully realistic – but entirely artificial – datasets, without PHI
- Tailor datasets by collaborator need or focus area
- Launch joint pilots or research across entities with minimal barriers
Supercharging Healthcare Analytics
Operational and strategic decisions require clean data – but real systems are often messy. Synthetic data offers:
- Cleaner timelines, complete records, and consistent structure
- Capability to run what-if scenarios for staffing, capacity, or outbreaks
- Built-in labels that simplify analytics pipelines and reduce preprocessing time
Also Read: An Entrepreneur’s Guide on Data Analytics in Healthcare
Strengthening Drug Safety Surveillance Post-Market
Monitoring side effects at scale is essential – but real adverse event data takes time. Synthetic cohorts enable:
- Simulation of long-term usage and rare-event reactions
- Early detection of safety signals before real-world aggregation catches up
- Scenario-based planning for label expansions or new demographic rollouts
Modeling Digital Twins for Predictive Clinical Planning
Virtual patient models (digital twins in healthcare) promise preemptive care – but need realistic inputs. Synthetic data provides:
- Virtual patient trajectories with precision and variability
- Simulated interventions to evaluate care decisions before applying them
- Twin models calibrated for demographic continuity and predictive accuracy
Optimizing Care Pathways Through Simulated Workflows
Improving hospital throughput, reducing readmission risk, or refining discharge planning requires rich operational simulations. Synthetic data allows:
- Simulating flows from admission to discharge to identify bottlenecks
- Modelling resource shifts – staffing changes, equipment reallocation
- Testing discharge strategies by predicting readmission triggers
Advancing Population and Public Health Research
Understanding population health trends requires large, diverse datasets. Synthetic populations make large-scale modeling both possible and private:
- Simulate national or regional cohorts with statistical accuracy
- Run “what if” analyses for screening programs or vaccination campaigns
- Forecast care demand, resource need, or outbreak emergence – all safely.
We can help you turn use cases into outcomes.
Real‑World Use Cases of Synthetic Data Healthcare
Synthetic data in healthcare is no longer theoretical-it’s powering real advances in research, product testing, and privacy-forward data operations. Below are five case studies showcasing how synthetic healthcare data looks in action.
1. Washington University School of Medicine (St. Louis)
Researchers validated the statistical similarity and utility of synthetic COVID‑19 patient data generated with MDClone. The study found synthetic datasets preserved the original’s fidelity while removing all patient identifiers.
2. Major U.S. Academic Hospital (Southern California)
A large teaching hospital in California used a synthetic EHR dataset to test and optimize a COVID-19 clinical data tool without exposing their real patient records. Internal validations confirmed strong statistical matches.
3. UK Biobank Lung Cancer Modeling (ADS-GAN / PATEGAN)
Researchers applied ADS‑GAN and PATE‑GAN to the UK Biobank dataset to generate synthetic samples for lung cancer risk prediction. The resulting models maintained predictive accuracy while protecting privacy.
4. ICU Time-Series Modeling with eICU/MIMIC (EHR-M-GAN)
EHR-M-GAN was used to generate synthetic ICU time series data using the MIMIC-III and eICU datasets. The synthetic data maintained key temporal patterns critical to downstream AI model training.
5. EchoNet-Synthetic Dataset: Synthetic Echocardiograms
Stanford’s EchoNet-Synthetic used a video diffusion model to generate synthetic echocardiograms, enabling safer cardiovascular AI development and faster model iteration without needing sensitive patient data.
Notable Examples from Other Institutions
- Patterson Dental slashed test data generation from hours to just 35 minutes using HIPAA-compliant synthetic test data.
- CDC’s NCHS published public-use mortality datasets transformed with synthetic data for healthcare AI, preserving analytics fidelity while removing identifiers.
- Everlywell accelerated feature deployment by 5× using synthetic datasets during development and QA processes.
| Organization / Project | Use Case | Key Benefit |
|---|---|---|
| Washington University (School of Medicine) | Synthetic COVID‑19 data testing | Real-time research with synthetic patient data |
| Southern California Academic Medical Centre | Research & AI pipeline testing | HIPAA-safe access to synthetic healthcare data |
| UK Biobank Lung Cancer Study | Prognostic modeling from synthetic data | Maintained performance with medical synthetic data |
| eICU/MIMIC Modeling | ICU outcome prediction | Enhanced predictive validity using synthetic data for healthcare AI |
| EchoNet‑Synthetic Project | Echocardiogram model training | Privacy-safe synthetic imaging dataset |
How to Create Synthetic Data for Healthcare Applications?
You can’t approach the process of synthetic data for healthcare the same way you would with regular data generation. It takes thoughtful planning to ensure the data feels real, protects patient privacy, and is technically sound. Whether it’s being used to train diagnostic tools, test clinical trial setups, or fine-tune imaging systems, synthetic data for healthcare needs to mirror actual medical situations – without ever risking exposure of real patient details.
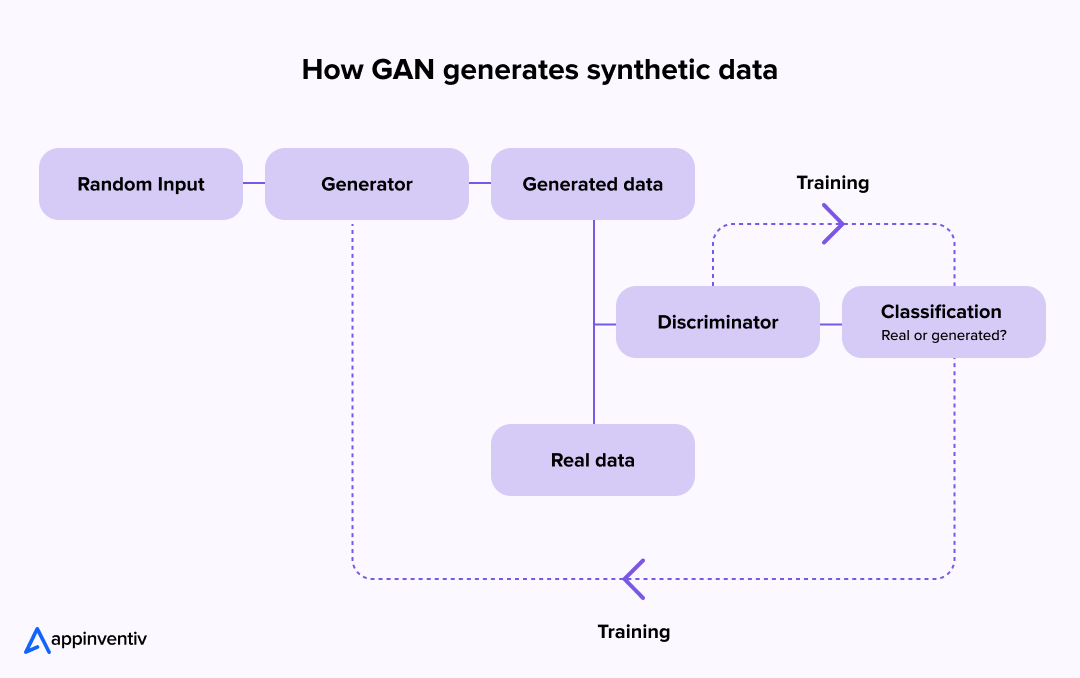
1. Define the Objective
The first step in generating synthetic healthcare data is to clarify the use case. Are you building a model for radiology, pathology, patient analytics, or patient outcome prediction? The chosen applications of synthetic data in healthcare dictate what type of data is required – tabular patient records, time-series vitals, 3D MRI scans, or multimodal data.
2. Select Data Type & Source Model
Depending on the types of healthcare synthetic data needed, you can use:
- Tabular generators for EHR and claims data.
- GANs and VAEs for medical imaging.
- Large Language Models for clinical notes and synthetic patient dialogues.
For realistic data, these models are often trained on de-identified or privacy-preserved datasets, ensuring no trace of real identities is carried over – addressing the challenges of using synthetic data in medicine.
3. Simulate or Model Patient Scenarios
Developers create logic-based rules or train neural networks to replicate disease progression, comorbidities, treatment effects, and demographic variation. The result is highly nuanced synthetic patient data that captures statistical and clinical variability.
4. Validate Against Real Distributions
To ensure high utility, synthetic data in healthcare must be statistically validated against real-world datasets. Tools like TSTR (Train on Synthetic, Test on Real) are used to check fidelity, utility, and fairness.
5. Automate Annotation (for Imaging Use Cases)
In imaging-based models, such as those used in dermatology or radiology, AI synthetic data healthcare workflows simulate varied imaging conditions and auto-label data with high precision – bypassing the need for manual clinical annotation.
Cost of Synthetic Healthcare Data
The cost of synthetic healthcare data creation varies based on data type, use case, and compliance needs:
| Data Type | Approx. Cost Range (USD) | Notes |
|---|---|---|
| Tabular EHR / Clinical Data | $10k – $50k+ | Depending on volume, diversity, and temporal depth. |
| Medical Imaging (CT, MRI, X-ray) | $50k – $250k+ | Includes asset creation, rendering, annotation, and model tuning. |
| Multimodal Patient Simulations | $100k+ | Combines tabular, time-series, and image/audio data. |
| Real-time Synthetic Data Pipelines | $200k+ | For use in online model training or continuous learning setups. |
Costs also account for infrastructure, talent, compliance auditing, and licensing. However, compared to the cost of acquiring real medical data – which includes consent, storage, security, and annotation – synthetic approaches are often more scalable and privacy-preserving.
Challenges of Using Synthetic Data in Medicine
Synthetic data in healthcare promises a future of secure, scalable, and ethically sound data sharing. But that future isn’t here just yet. Beneath the surface of this promising innovation lies a tangle of complexities – from technical inconsistencies to regulatory gaps and trust barriers. If AI synthetic data healthcare tools are to move beyond pilot projects and into everyday medical use, we need to unpack the challenges holding them back.
1. No Clear Standards, Just Competing Methods
Healthcare teams across the globe are building synthetic datasets – but not in the same way. Techniques vary widely, with little agreement on how to judge the quality or usefulness of synthetic patient data. What’s realistic to one system might be unreliable to another. Without shared benchmarks, comparing models – or trusting them across institutions – becomes a guessing game.
2. A Regulatory Blind Spot
Rules around AI synthetic data in healthcare are still a work in progress. While a few countries are drafting frameworks, there’s no global guidance just yet. This patchy oversight makes hospitals and medtech providers wary – especially when it comes to sensitive areas like diagnostics or treatment response. Until regulations catch up, hesitation will remain the default.
3. Privacy: Solved or Just Shifted?
Synthetic data healthcare tools are often praised for solving privacy issues, but the reality isn’t always so clean. In rare cases – especially with unique or limited datasets – there’s still a risk of reverse engineering personal details. So instead of erasing privacy concerns, some models may just be reshaping them in subtler ways.
4. A Shortage of Cross-Domain Talent
Producing healthcare synthetic data that mirrors real-world clinical patterns isn’t easy. It takes more than machine learning – it takes medical insight. But finding people who truly understand both is tough. Without that hybrid expertise, synthetic datasets often miss important nuances or clinical logic, limiting their real-world usefulness.
5. Trust Doesn’t Happen Overnight
Even the best synthetic data for healthcare won’t be adopted instantly. Medicine runs on evidence and experience, and synthetic records – however statistically sound – lack that lived-through texture clinicians rely on. Confidence won’t come from claims alone. It’ll take time, transparency, and real-world results to earn it.
Building Smarter Healthcare Solutions with Synthetic Data and Custom Development
Working with synthetic data isn’t just about generating numbers – it’s about building safe, scalable, and compliant systems that bring those datasets to life. That’s where we come in.
Appinventiv helps healthcare organizations unlock the full potential of synthetic data in healthcare through end-to-end custom healthcare software development. Whether you need a secure sandbox to test predictive models or a platform that leverages AI synthetic data healthcare tools for diagnostics or research, we build from scratch – no templates, no shortcuts.
Our solutions are designed to support the real-world use cases of synthetic patient data: training AI models without risking PHI, simulating rare disease progression, improving clinical trial efficiency, and enabling hospitals to test new workflows. We’ve worked across a range of applications, from mobile platforms to full-scale enterprise systems that handle large volumes of synthetic healthcare data.
Security, compliance, and interoperability are woven into every build and because synthetic datasets evolve fast, we also provide data versioning, auditing, and monitoring frameworks – so your systems don’t just start smart, they stay smart.
Let’s create custom, compliant platforms that bring your healthcare vision to life.
Synthetic Data is no Longer Optional – It’s Inevitable
Healthcare is at a turning point. With tighter data laws, higher patient privacy expectations, and the growing need for robust AI training models, synthetic data in healthcare is emerging not as an alternative, but as a necessity. It enables safe experimentation, unlocks innovation, and accelerates go-to-market timelines for healthtech solutions.
From training diagnostic algorithms to supporting virtual clinical trials, the impact of synthetic healthcare data is real. But reaping those benefits requires more than just access to datasets – it calls for systems that are built for this new reality. This is where custom healthcare software development plays a crucial role, shaping tools that can integrate, generate, and scale synthetic patient data securely and intelligently.
The future of AI synthetic data healthcare isn’t a distant one. It’s already unfolding. Those who invest early in the right strategy, partnerships, and infrastructure will lead the next wave of healthcare innovation – with both speed and compliance on their side.
So what are you waiting for? Connect with our team of healthcare software experts now.
FAQs
Q. What is synthetic data in healthcare?
A. It’s data that is made up, but still useful. Imagine patient records that are totally fake – but built in a way that they mimic real-life cases. That’s what synthetic data is. It lets hospitals and developers test systems or train models without touching anyone’s private health information.
Q. How is the healthcare industry using synthetic data?
A. More than you’d think. It’s being used to try out new healthcare apps, fine-tune AI models, and run internal tests – basically anywhere real patient data would be too sensitive or tricky to get. It’s helping teams move faster without compromising privacy.
Q. How do you use synthetic data to train a healthcare AI model?
A. The process is similar to training with real data. You take a large set of synthetic health records, plug them into the model, and let it find patterns – like what symptoms lead to what diagnoses. It’s a safe way to teach the model without handling real patient details.
Q. Is synthetic data the future of clinical trials?
A. It’s looking that way, at least partly. While it will not replace real-world trials today or tomorrow, synthetic data has started helping researchers simulate trial scenarios early on, to save them time, cut down costs, and even help identify issues before the actual trials begin.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.

How to Build a Custom Pediatric EMR and EHR System?
Key takeaways: Clinical Precision: Custom systems accommodate pediatric-specific data points like percentile curves and weight-based longitudinal dosing. Interoperability: Seamless data exchange via HL7 FHIR ensures your practice stays connected to pharmacies, labs, and state registries. Regulatory Resilience: Built-in compliance with HIPAA, HITECH, and MACRA/MIPS reduces legal friction. Enhanced Engagement: Parent portals reduce administrative overhead by…

Change Management in Healthcare: Principles, Processes, and Models
Key Takeaways Change in healthcare fails quietly when ownership, workflow alignment, and follow-through are missing. Successful change management in healthcare focuses on adoption, not just system implementation. Clinical workflows and workforce capacity determine whether transformation sticks or stalls. Governance, clear accountability, and post-go-live support matter more than the model used. Sustainable healthcare transformation depends on…
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…