- Healthcare Prescriptive Analytics Market & Investment Outlook: The Growth Opportunity Businesses Must Know of
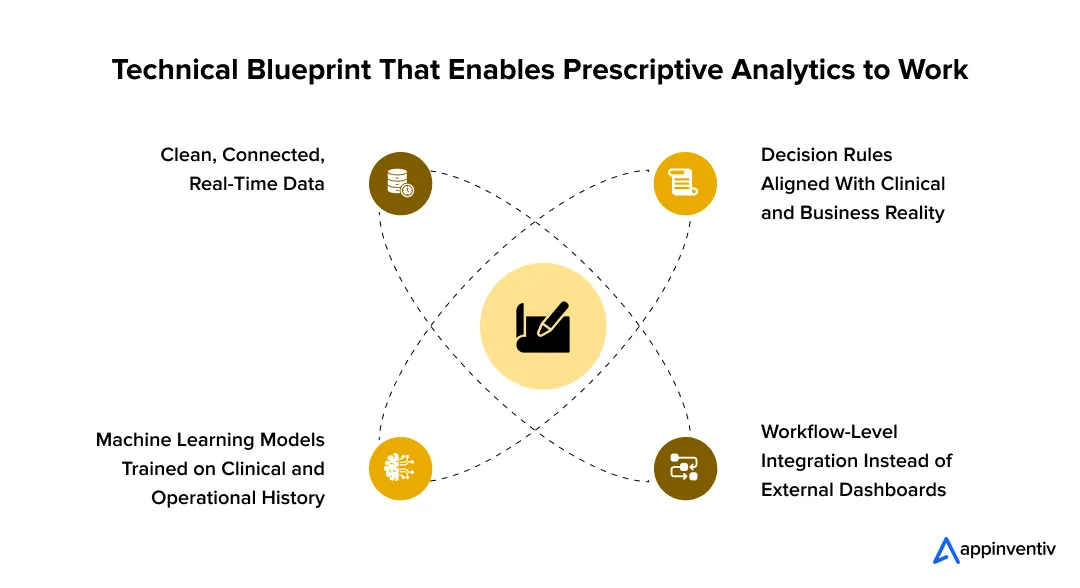
- Technical Foundations: How Prescriptive Analytics Actually Works
- 1. Clean, Connected, Real-Time Data
- 2. Machine Learning Models Trained on Clinical and Operational History
- 3. Decision Rules That Reflect Clinical and Business Reality
- 4. Workflow Integration Instead of Separate Dashboards
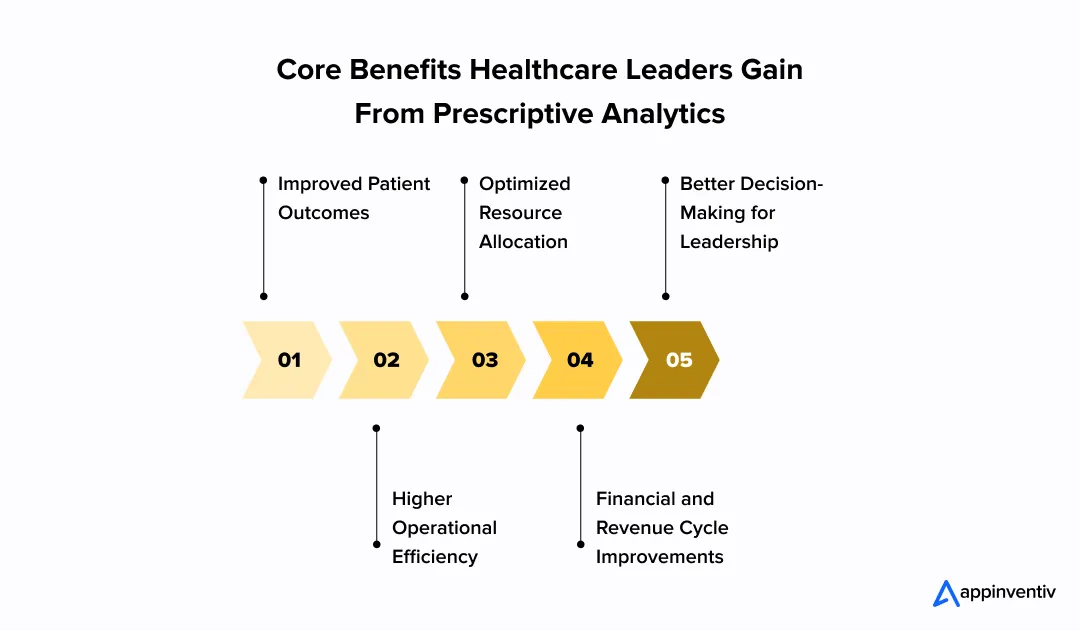
- Benefits of Prescriptive Analytics in Healthcare
- Improved Patient Outcomes
- Higher Operational Efficiency
- Optimized Resource Allocation
- Financial and Revenue Cycle Improvements
- Better Decision-Making for Leadership
- Prescriptive Analytics Use Cases in Healthcare
- Capacity Planning for High-Demand Services
- Chronic Disease Program Targeting
- Demand-Supply Forecasting for Pharmacy and Consumables
- Preventive Maintenance for Medical Equipment
- Care Pathway Optimization for Specific Conditions
- Predictive vs Prescriptive Analytics in Healthcare
- How Can Businesses Leverage Healthcare Prescriptive Analytics
- Step 1: Start With a Single Issue, Not the Whole Hospital
- Step 2: Make Data Practical, Not Perfect
- Step 3: Keep Workflows Familiar
- Step 4: Measure Outcomes Early and Openly
- Step 5: Scale Only After Trust Is Earned
- Common Challenges in Prescriptive Analytics Adoption Across the Healthcare Sector
- A Strategic Roadmap: Best Practices for Leveraging Prescriptive Analytics
- 1. Start With One Clear Goal and One KPI
- 2. Identify the Minimum Data Required - Not “All Data”
- 3. Build a Pilot Model That Works in One Department
- 4. Deploy Inside Existing Workflows - No New Dashboards
- 5. Collect Real Feedback During Live Usage - Not After Go-Live
- 6. Measure Impact Against the First KPI - Not 20 Metrics
- 7. Scale Only When the First Department Asks for It
- The Future Outlook: What Businesses Can Expect
- AI-Based Diagnostics Will Move From Supportive to Central
- Wearables and IoT Will Power Continuous, Real-Time Intervention
- Cross-Industry Collaborations Will Speed Up Innovation
- Compliance and Regulation Will Shape System Design From Day One
- Leadership Will Expect Operational and Financial Visibility in Real Time
- Why Appinventiv Is the Partner Healthcare Leaders Trust
- FAQs
A healthcare business doesn’t fall behind because its teams lack skill. It falls behind when decisions take too long. Bed allocation runs on yesterday’s data. Procurement reacts only when shortages hit. Care managers step in after a patient is already at risk. And leadership gets a picture of what’s happening only after the quarter closes, not when it’s happening.
Every CEO and CTO in healthcare has felt this gap. You’ve already invested in dashboards, predictive tools, EMRs, and automation, yet something is still missing. You know what is happening and often why it’s happening, but not what to do next in the moment that matters.
That’s why so many leadership teams are shifting their attention toward prescriptive analytics in healthcare. Because unlike traditional healthcare analytics that simply describe or predict trends, prescriptive health goes one step further and recommends actions that fit the situation.
- It shows the best staffing model for tomorrow’s patient load.
- It alerts clinicians before a readmission is likely and proposes the exact intervention.
- It gives procurement teams a replenishment plan before supply risk hits.
Simply put, it’s not just insight but guided action.
For many businesses, this is the first time technology is shaping operational decisions proactively rather than documenting them afterward. And that’s the real value of prescriptive analytics for healthcare – smarter resource allocation, reduced clinical risk, and leadership decisions that match the pace of real-world demand.
In this blog, we’ll break down how prescriptive analytics in healthcare works, walk through the use cases, share its examples in healthcare, and outline the common challenges that leadership needs to be ready for. We’ll also look at the future of the technology, and how predictive and prescriptive analytics in healthcare are beginning to work together to support faster, more confident decision-making across the organization.
Prescriptive analytics can unlock that next leap for your healthcare system.
Healthcare Prescriptive Analytics Market & Investment Outlook: The Growth Opportunity Businesses Must Know of
For leadership, prescriptive analytics in healthcare is not just “better reporting”. It is a decision layer that looks at historical data, real-time signals, and clinical or operational guidelines, then recommends the best course of action for a specific patient, unit, or process. As NIH puts it, prescriptive analytics builds on diagnostic and predictive analytics to suggest optimal decisions that support evidence-based interventions and better operational outcomes in healthcare settings.
The prescriptive analytics market was valued at about $9.53 billion in 2023 and is projected to reach roughly $ 61.92 billion by 2030, growing at close to 31.8% from 2024 to 2030, according to Grand View Research. That growth reflects a shift in budgets: instead of funding generic analytics, boards are now backing systems that help decide what to do next and not just forecast what might happen.
IBM’s analysis of the sector explains why this is happening. Healthcare is moving from volume-based to value-based care at the same time as costs, chronic disease burden, staffing shortages, and patient expectations are all rising. IBM highlights that prescriptive technologies allow decision-makers to compare multiple “what-if” scenarios, balance trade-offs, and choose the most effective and efficient path in real time – whether that’s a treatment decision, a staffing plan, or a capacity move.
For CEOs and CTOs, this has a clear investment implication. The future of prescriptive analytics in healthcare industry will reward organizations that start now, in focused areas, and scale from there. Early adopters will accumulate model performance, workflow familiarity, and cultural trust around data-driven decisions. Late adopters will be buying into a mature market where competitors already run key parts of their operations on prescriptive intelligence.
So the investment question isn’t “if” anymore. It’s where you deploy prescriptive analytics first to prove ROI, and how quickly you can move from pilots to decisions that materially change your clinical, operational, and financial metrics.
Technical Foundations: How Prescriptive Analytics Actually Works
Before leaders decide where to leverage the role of prescriptive analytics in healthcare, it helps to understand what sits under the hood. Many hospital executives we speak with already have predictive tools, command-center dashboards, or BI platforms, yet the outcomes don’t change much. The reason is simple: prescriptive analytics only works when certain technical pieces fit together. Without that foundation, the system can show data, but it cannot recommend decisions.
Let’s give you a clear picture of what needs to be true for prescriptive analytics to actually deliver results.
1. Clean, Connected, Real-Time Data
Prescriptive analytics depends on more than historical records. It needs live data from EHRs, labs, wearables, scheduling systems, supply chain tools, and command-center software. When data is fragmented, the recommendations will be fragmented too.
Why it matters: Every operational delay – from bed allocation to discharge planning – happens because decision-makers don’t see the full picture at the moment they need it.
2. Machine Learning Models Trained on Clinical and Operational History
These models study how similar situations played out in the past and learn what outcomes followed different actions. For example, how staffing shifts affected patient flow or how treatment paths affected readmission risk.
Why it matters: The system becomes smarter over time because it learns from the hospital’s own patterns, not generic rules.
3. Decision Rules That Reflect Clinical and Business Reality
This layer converts predictions into recommended actions. It considers guidelines, reimbursement policies, risk thresholds, safety rules, staffing rules, and resource limits before proposing an intervention.
Why it matters: This is the step that turns forecasting into something hospitals can actually execute.
4. Workflow Integration Instead of Separate Dashboards
Recommendations that live in a separate dashboard are ignored. Recommendations that show up in the EHR screen, command-center panel, pharmacy system, or staffing tool are acted on.
Why it matters: Adoption is not driven by analytics – it’s driven by whether clinicians and managers can use the insight without changing their routine.
Benefits of Prescriptive Analytics in Healthcare
Healthcare prescriptive analytics is useful for one simple reason – it tells you what to do next, not just what happened or what might happen. When hospitals are dealing with constant pressure, limited people, and unpredictable demand, having a system that recommends the best next step becomes extremely valuable. If the goal is to improve outcomes while running the organisation more efficiently, this is where prescriptive analytics fits. Let’s look at the benefits of prescriptive analytics in healthcare in detail below:
Improved Patient Outcomes
Prescriptive analytics models flag risk before it becomes a crisis. Clinicians get early warnings about deterioration, suggestions for medication adjustments, and reminders for follow-ups that would otherwise slip through. It doesn’t replace judgmentbut helps the care team act faster and more confidently. The practical impact shows up in fewer complications and better recoveries.
Higher Operational Efficiency
Hospitals lose time when departments wait on each other. Prescriptive analytics in healthcare looks at how patients, staff, and resources move across the system and recommends fixes before delays spread. Instead of reacting to overcrowding in the ER or last-minute OR reschedules, teams get guidance early enough to prevent the slowdown.
Optimized Resource Allocation
Prescriptive analytics for healthcare helps leaders plan staffing and equipment based on real demand rather than old patterns. It takes into account seasonality, acuity, and expected surges and suggests the most sensible staffing distribution. It’s not about cutting people – it’s about putting the right number of people in the right place so no one is burnt out and budgets stay under control.
Financial and Revenue Cycle Improvements
Revenue loss in hospitals rarely comes from one big mistake – it comes from hundreds of small ones that go unnoticed. Prescriptive analytics healthcare models spot patterns that lead to denials, delays, or reimbursement issues and recommend what to fix before the money is lost. It makes billing and coding more accurate without forcing teams to dig through every case manually.
Better Decision-Making for Leadership
Prescriptive health tools help executives test decisions before making them. Instead of guessing which plan will protect KPIs, leaders can see how each scenario affects cost, workload, and patient care. It doesn’t replace experience – it gives leaders clearer visibility so major decisions are less of a gamble.
Prescriptive Analytics Use Cases in Healthcare
Prescriptive analytics in healthcare is most helpful when teams have to make fast decisions with limited time and too many variables. It doesn’t replace people. It just gives clearer direction on what to do next so decisions aren’t based on guesswork.
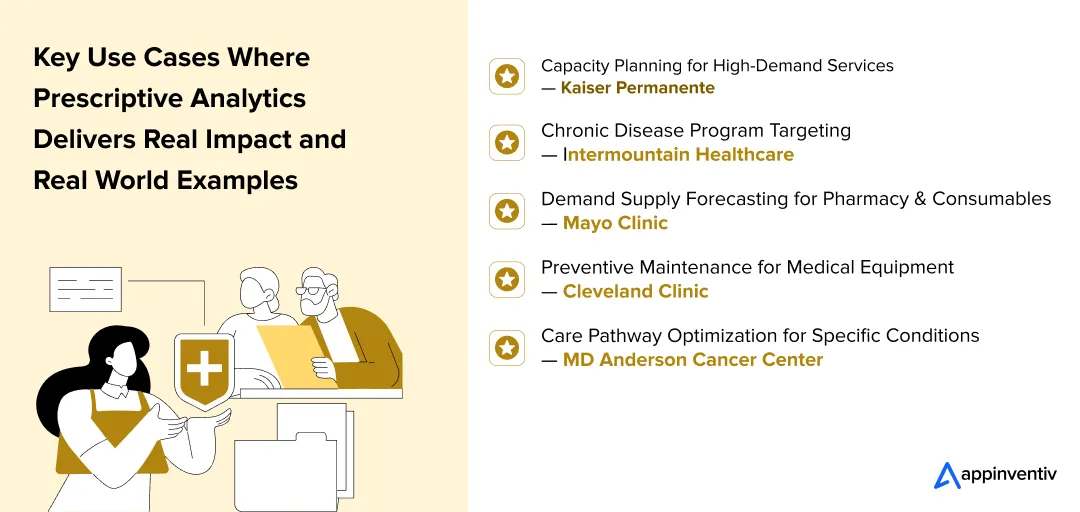
Capacity Planning for High-Demand Services
Some departments are always full no matter what you plan, and that affects the rest of the hospital. Prescriptive models look at referral patterns, seasonal changes, and local disease trends and give a practical plan for adding capacity before things get backed up. It gives leaders enough time to adjust instead of scrambling later.
Real example: Kaiser Permanente uses prescriptive planning for oncology and cardiology surges so they can add capacity early and keep patients from waiting weeks for treatment.
Chronic Disease Program Targeting
Chronic care becomes expensive when everyone gets the same level of attention. Prescriptive health tools point out which patients are most likely to get worse if nobody steps in soon and recommend the order of outreach that creates the most impact. It helps care teams focus their time where it actually matters.
Real example: Intermountain Healthcare uses prescriptive analytics to identify diabetes and hypertension patients who need early intervention instead of waiting for emergency visits.
Demand-Supply Forecasting for Pharmacy and Consumables
Running out of medications at the wrong time forces emergency orders and delays treatment. Healthcare prescriptive analytics predicts when certain drugs or consumables will run short and suggests when and how much to reorder so the pharmacy isn’t constantly firefighting.
[Also Read: 10 Use Cases and Examples of How Pharmacy Data Analytics is Transforming Operations and CX]
Real example: Mayo Clinic is one of the leading prescriptive analytics examples in healthcare. The firm applies prescriptive forecasting to specialty medications to avoid stockouts and reduce last-minute procurement.
Preventive Maintenance for Medical Equipment
Equipment failures always happen when the hospital is already running tight. Prescriptive analytics for healthcare predicts when machines are likely to fail based on how they’re being used and suggests the best time to schedule servicing before anything shuts down.
Real example: Cleveland Clinic uses prescriptive maintenance for large imaging systems so repairs happen before downtime hits operating and radiology schedules.
Care Pathway Optimization for Specific Conditions
Two patients with the same diagnosis can respond very differently to treatment. Prescriptive analytics healthcare models analyze thousands of previous cases and recommend the most effective treatment sequence for a specific patient profile so care plans aren’t based on trial and error.
Real example: MD Anderson Cancer Center uses prescriptive pathway models to match cancer patients with the treatment sequence that statistically delivers the best response.
After seeing where prescriptive analytics actually works in real hospital settings, the next question most leaders ask is where it sits compared to predictive tools they already use. Many organizations think they’re “doing prescriptive” because they have forecasting dashboards, but the two are not the same – and the results they deliver are very different.
Predictive vs Prescriptive Analytics in Healthcare
Most businesses already use healthcare predictive analytics to estimate what might happen next. Prescriptive healthcare analytics goes a step further by recommending what to do about it. Both are valuable, but they serve different purposes and require different decision mindsets. Knowing the difference between predictive and prescriptive analytics in healthcare helps leadership place investments in the right technology and the right workflows.
| Dimension | Predictive Analytics | Prescriptive Analytics |
|---|---|---|
| Core question it answers | “What is likely to happen?” | “What should we do about it?” |
| Main input | Past data and forecasting models | Forecast + clinical/operational rules + real-time conditions |
| Output format | Risk score, probability, trend, forecast | Recommended action with reasoning and alternatives |
| Typical user | Analysts, care managers, planners | Clinicians, operational leaders, executives |
| Human effort required | High – people must decide what action to take | Lower – system recommends best action and timing |
| Speed of impact | Useful for planning and risk awareness | Useful when decisions need to happen now |
| Example in practice | Predicts a potential staff shortage next week | Suggests exact staffing plan to avoid the shortage |
| Strategic role | Awareness and preparation | Execution and measurable outcome improvements |
How Can Businesses Leverage Healthcare Prescriptive Analytics
The biggest mistake hospitals make is treating prescriptive analytics like another IT rollout. It only works when it starts small, proves returns quickly, and grows from there. The goal isn’t to “install technology” – it’s to embed decision support into the areas of the organisation where it will be used every day.
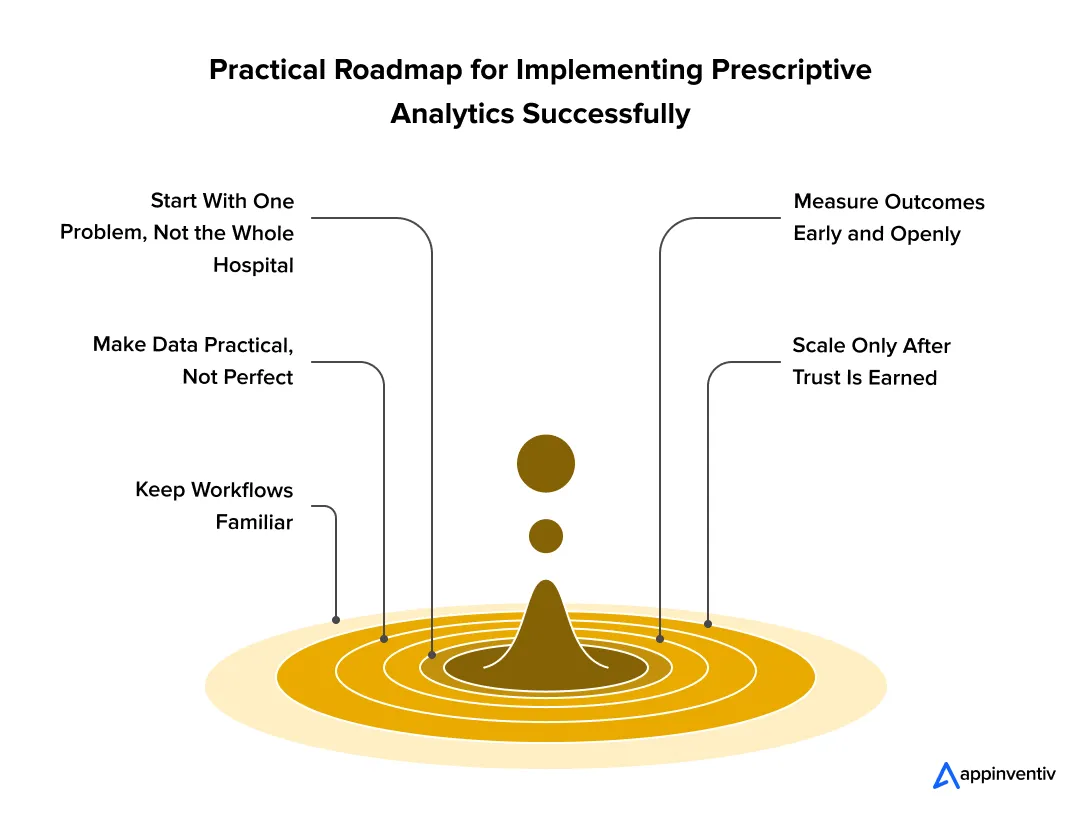
Step 1: Start With a Single Issue, Not the Whole Hospital
Prescriptive analytics in healthcare delivers real value when it solves a single concrete problem first – not when it tries to transform the entire system in one go. Pick a use case where decisions are frequent, measurable, and painful today. That could be OR scheduling, discharge bottlenecks, or pharmacy ordering. If the first win is visible, adoption becomes much easier across departments.
Step 2: Make Data Practical, Not Perfect
Leaders often wait for “clean, complete data” before moving forward. That day never comes. A prescriptive analytics healthcare project can begin with what is already available – EHR data, ADT feeds, vitals, supply consumption trends – and improve over time. The important thing is to feed the model with data that reflects how the hospital actually runs, not data that looks perfect in theory.
Step 3: Keep Workflows Familiar
If clinicians or operations managers have to open a new screen or remember new steps, adoption drops instantly. Prescriptive analytics for healthcare works best when recommendations appear inside the system people already use – the EHR, the capacity board, the staffing app. The technology should move toward the workflow, not the other way around.
Step 4: Measure Outcomes Early and Openly
Prescriptive analytics succeeds when improvements are clear and visible. Track outcomes from day one – even small ones – and share them. Shorter wait times, fewer readmissions, better OR utilisation, or lower emergency stock orders matter more to staff than abstract ROI charts.
Step 5: Scale Only After Trust Is Earned
Once one area shows success, teams start coming forward with their own problems. That’s the best moment to scale prescriptive health workflows – not before. Expansion should follow demand, not force it. If clinicians and managers ask for it, the rollout will be smooth. If it’s forced, resistance will be high.
Common Challenges in Prescriptive Analytics Adoption Across the Healthcare Sector
Prescriptive analytics isn’t difficult because of the technology. It’s difficult because hospitals are busy, workflows are fragile, and every decision has clinical, financial, and human consequences. Most failed projects don’t fail in the model – they fail in adoption, trust, and day-to-day execution. Understanding the barriers upfront makes rollout smoother and protects ROI.
| Challenge | How it Impacts the Organization | How to Resolve It |
|---|---|---|
| Data is scattered across too many systems | Recommendations become unreliable when EHR, pharmacy, lab, scheduling, and finance systems don’t talk to each other. Teams stop trusting the output. | Start with one use case and integrate only the data that matter for that use case. Expand later. Don’t wait for “perfect data”. |
| Clinicians worry models will override judgment | If the tool feels like it’s replacing expertise instead of supporting it, adoption collapses immediately. | Position prescriptive analytics healthcare models as decision support, not automation. Final call stays with clinicians. |
| “New screens” break workflow | If staff have to open a new app or dashboard, they simply won’t use it during high-pressure moments. | Embed recommendations inside the systems clinicians and managers already use – EHR, staffing board, command center, etc. |
| No shared definition of success | IT looks at accuracy, finance looks at ROI, clinicians look at patient safety – and no one agrees whether the project is working. | Set one shared win metric before deployment – fewer readmissions, shorter discharge cycle, safer ICU transition, etc. |
| Over-engineering in phase one | Starting big slows implementation, drains resources, and produces no visible results for months. | Begin with a small prescriptive analytics for healthcare pilot that solves one painful problem and makes the success visible. |
| Lack of transparency in recommendations | If the system gives an answer but not the “why”, people ignore it. Blind recommendations are not trusted. | Use explainable models – show the factors behind the recommendation in simple language. Not equations. |
| Change management is overlooked | Teams assume “because it works on paper” it will work in a real hospital. It won’t – people need to adjust. | Add training, weekly feedback loops, and live shadowing support during the first 60-90 days. Adoption matters more than algorithms. |
| Rollout is rushed to multiple units | Too much, too fast causes frustration and resistance even if the tool is good. | Scale prescriptive health workflows only when the first unit asks for it – demand-led scaling works, forced deployment doesn’t. |
| Regulatory and ethical constraints | Businesses hesitate when they’re unsure whether prescriptive systems could raise healthcare compliance issues, safety questions, or liability risk. Leadership pauses adoption rather than risk exposure. | Build prescriptive analytics into an existing governance framework – HIPAA/GDPR compliance, clinical sign-off rules, audit trails, and ethical review. This protects decisions while maintaining speed. |
A Strategic Roadmap: Best Practices for Leveraging Prescriptive Analytics
Most hospitals don’t struggle with the idea of prescriptive analytics – they struggle with where to start and how to roll it out without disrupting clinical flow. A successful implementation doesn’t begin with algorithms; it begins with clarity, sequencing, and realistic expectations. The roadmap below reflects how hospitals that actually succeeded and approached transformation.
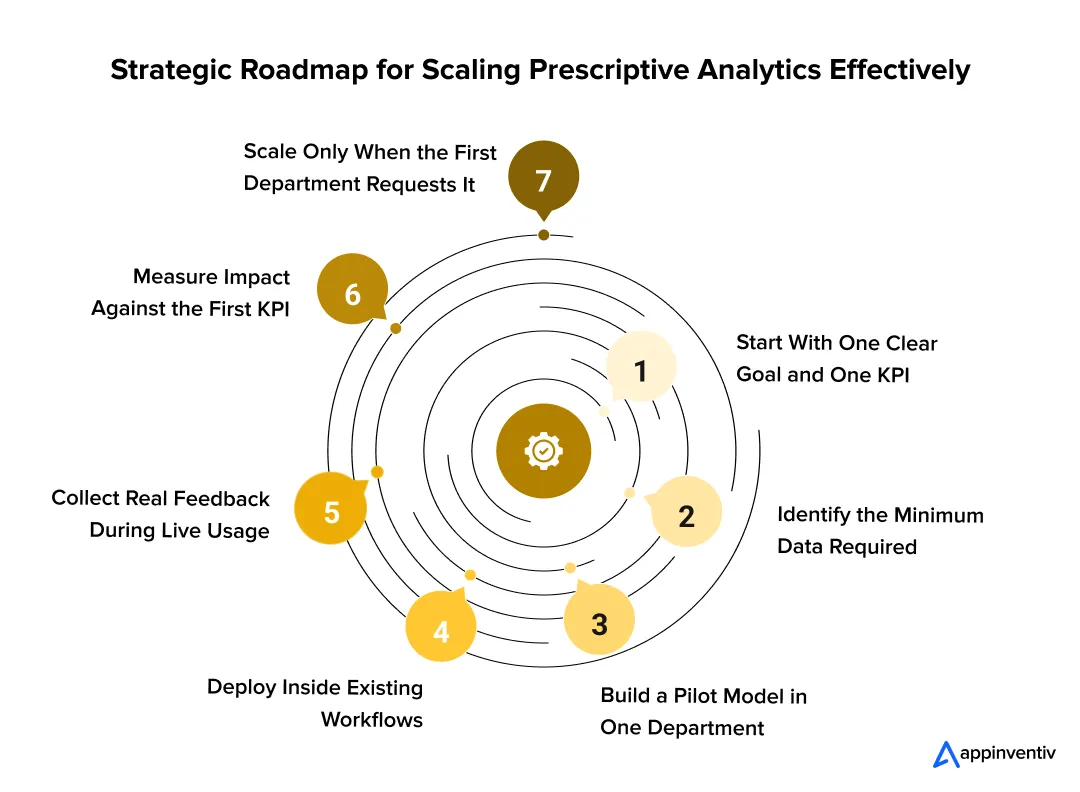
1. Start With One Clear Goal and One KPI
Prescriptive analytics projects go off-track when everyone expects a different win. Pick one measurable outcome first – shorter discharge time, fewer readmissions, OR throughput, ICU step-down safety, or staffing cost control.
Why this works: When one KPI moves, leadership support becomes automatic and scaling becomes pull-based rather than forced.
2. Identify the Minimum Data Required – Not “All Data”
A large data overhaul is where most projects stall. For the first rollout, only integrate the systems required to improve the chosen KPI – EHR + vitals + lab + scheduling, or EHR + pharmacy + billing, etc.
[Also Read: EHR Software Development – Benefits, Features, Process, Costs]
Why this works: Prescriptive analytics for healthcare shows value faster when the scope is narrow and relevant.
3. Build a Pilot Model That Works in One Department
Not a demo. Not a lab. A real unit with real patients. Choosing the right unit matters – ideally a department with strong leadership support, clear pain points, and staff willing to give feedback.
Why this works: One visible win converts sceptics more effectively than 20 presentations.
4. Deploy Inside Existing Workflows – No New Dashboards
If users are asked to switch screens, adoption collapses. Recommendations must surface inside tools already used – EHR, command centre, scheduling board, pharmacy system, etc.
Why this works: Zero behavioural change = fast adoption.
5. Collect Real Feedback During Live Usage – Not After Go-Live
Shadow clinicians during the first 60–90 days. Track where the system feels helpful, where it slows decisions, and where the reasoning needs clarity.
Why this works: Prescriptive analytics in healthcare succeeds only when the end-user feels the system is supporting them, not instructing them.
6. Measure Impact Against the First KPI – Not 20 Metrics
If readmissions were the target, measure only that. If OR capacity was the target, measure only that.
Why this works: Proving success once builds trust. Trying to prove everything at once destroys momentum.
7. Scale Only When the First Department Asks for It
Departments should request adoption because they saw the impact – not because leadership mandated it.
Why this works: Demand-led scaling leads to culture pull, not resistance.
The Future Outlook: What Businesses Can Expect
Prescriptive analytics is still in early stages across the healthcare ecosystem, but the direction is no longer uncertain. Hospitals are already shifting from reporting-based management to operating models where decisions are guided in real time. The next phase won’t revolve around “more data” or “more dashboards” – it will be about turning information into the right action at the exact moment it’s needed, without slowing down clinical staff.
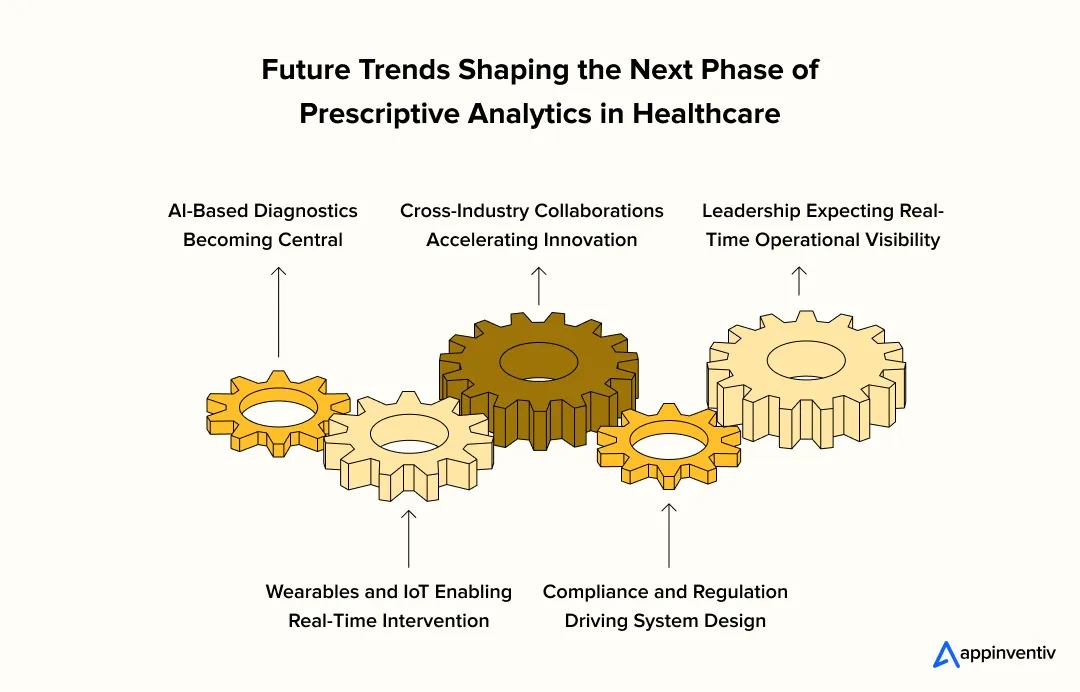
AI-Based Diagnostics Will Move From Supportive to Central
Prescriptive analytics healthcare platforms will increasingly pair with AI-based diagnostic engines. Instead of simply flagging abnormalities, the AI-driven prescriptive analytics systems will recommend next investigative steps or treatment paths. The clinician remains in control, but diagnostic uncertainty shrinks, and time-to-decision becomes shorter for complex cases.
[Also Read: How is AI in Healthcare Transforming the Industry?]
Wearables and IoT Will Power Continuous, Real-Time Intervention
The rise of connected medical devices is changing how care teams track patients. With wearables streaming vitals continuously, prescriptive healthcare analytics can recommend preventive actions hours before a problem becomes visible. Long-term condition management will move from periodic check-ins to continuous course correction.
Cross-Industry Collaborations Will Speed Up Innovation
Some of the biggest breakthroughs will come from partnerships between hospitals, insurers, med-tech firms, pharmaceutical companies, and even consumer tech brands. Instead of innovation happening in isolation, prescriptive health models will be trained on broader data ecosystems – improving treatment recommendations, cost control, and patient engagement across the full care journey.
Compliance and Regulation Will Shape System Design From Day One
New laws and guideline updates will push organisations to build governance into their systems instead of adding it later. Prescriptive analytics for healthcare will include validation trails, safety rules, and audit-ready logic to make sure automated recommendations support – rather than complicate – regulatory compliance.
Leadership Will Expect Operational and Financial Visibility in Real Time
Executives won’t wait for monthly reports to see where margins, staffing, or care quality are heading. Prescriptive analytics platforms will show the operational impact of decisions in advance, allowing leaders to protect capacity, quality, and financial performance before pressure builds.
Why Appinventiv Is the Partner Healthcare Leaders Trust
Hospitals don’t need another vendor. They need a partner who understands clinical reality, regulatory pressure, operational complexity, and the day-to-day challenges of adoption. That’s exactly where Appinventiv has been successful – building healthcare platforms that don’t just work in a demo but work in real facilities with real patients and real constraints.
As a healthcare software development services firm, our approach to prescriptive analytics for the businesses is shaped by three things executives consistently tell us they care about:
We Build for Adoption, Not Just Algorithms
A prescriptive analytics model is useless if clinicians don’t use it. We design recommendations to appear inside the workflows hospitals already rely on – the EHR, nursing dashboards, pharmacy systems, and command-center tools. Zero disruption, zero extra clicks. This is why our solutions are actually used in practice, not just approved on paper.
We Engineer for Compliance From Day One
Healthcare software isn’t like any other software – HIPAA, GDPR, local data laws, clinical audit trails, and medical safety protocols aren’t optional. Our teams are trained to design around compliance requirements from the beginning so hospitals never have to “retrofit” privacy, security, or governance later.
We Deliver Results That Leadership Can Measure
Boards don’t approve technology for novelty – they approve it when outcomes, capacity, quality, and margins improve. We structure prescriptive health projects so the first rollout solves one visible, high-value problem and generates measurable ROI quickly. Once that success is proven, scaling becomes pull-based, not push-based.
Get in touch with our experts to build prescriptive analytics that actually fits your hospital workflows
FAQs
Q. What is prescriptive analytics in healthcare?
A. Hospitals need more than just knowing what already happened. Prescriptive analytics tells them exactly what to do next. Live patient data mixes with treatment guidelines and how the hospital is running to give specific advice: change treatment plans, move nurses where they’re needed most, order the right amount of supplies.
Hospital leaders see benefits right away – doctors make decisions faster and everything gets used more efficiently. Patient care gets better while the money side improves too. The technology pays for itself quickly, fewer patients come back with problems, daily work flows better, and planning resources become way more accurate across the whole hospital.
Q. How do prescriptive analytics improve healthcare management?
A. Prescriptive analytics changes how healthcare businesses operate by giving actionable advice from their data. Results show up right away after setup. Bed assignments get optimized while patient wait times drop at the same time. Additionally, staff schedules work better because they’re based on when people actually need care.
Hospital executives see cost cuts from using resources smartly and running more efficiently. Apart from this, patient care improves when the system suggests better treatment approaches. Hospitals can get ahead of problems instead of always reacting to whatever goes wrong. Simply put, everything runs smoothly while patients have better experiences, and the bottom line gets stronger.
Q. How do prescriptive models integrate with EHR/HL7 FHIR?
A. Prescriptive systems connect to hospital record systems using HL7 FHIR APIs. Data flows straight into what doctors and nurses already do every day. FHIR’s standard setup lets the analytics pull patient info, lab results, and clinical notes while pushing recommendations right back into the same screens doctors use.
This means physicians get helpful suggestions without switching between different programs. Healthcare executives get these systems running faster, spend less on training staff, and see more people actually using the technology. The standard approach works with different EHR companies, so hospitals don’t get locked into one vendor and can add more analytics tools later.
Q. How to measure ROI and clinical impact of prescriptive analytics?
A. Figuring out if prescriptive analytics actually pays off means watching both the money side and patient care results over time. The financial stuff includes spending less on readmissions, getting patients out faster, and making your staff more productive. For patient care, you track satisfaction scores, death rates, and whether doctors follow treatment protocols.
You need baseline numbers before you start so you know what has improved. Then check progress every quarter to see if things are actually getting better. Most businesses save a major chunk the first year by using resources smarter. Track each project separately so you know which ones work best. Compare your results to industry averages to see how you’re doing. Better patient outcomes become the real long-term payoff that goes way beyond just saving money.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…