- How to Map the Regulatory Terrain - HIPAA, HITECH, and What’s Emerging
- Building the Foundation of a HealthTech Platform
- Data Transmission and Storage
- How to Build a Culture of Security
- Third-Party Vendors: You’re Only as Compliant as Your Weakest Integration
- Ways to Manage Monitoring, Vulnerability Management, and Incident Response
- Balancing Compliance with Innovation
- How I Approach Compliance as a Trust Layer - Not a Bottleneck
- FAQs
Key takeaways:
- Build HIPAA, HITECH, and other regulatory requirements into your platform’s architecture from the start.
- Stay ahead of emerging regulations like FHIR and SMART on FHIR to ensure seamless integration.
- Implement encryption, access controls, and secure APIs as core components of your platform’s foundation.
- Vet every third-party vendor to ensure they meet compliance requirements and have signed BAAs.
- Foster a company-wide commitment to compliance through ongoing training, cross-functional ownership, and real-time monitoring.
I still remember my first week as CTO at a healthcare startup. We had just finished our MVP – a sleek, cloud-native platform meant to simplify chronic care management. Everything worked. The UI was sharp, the backend scalable, and early users were impressed.
Then came the question from our legal consultant:
“So, how are you handling HIPAA compliance?”
There was a moment of silence in the room. Not because we didn’t care – but because, like many early-stage tech teams, we had underestimated just how complex the US HealthTech regulations landscape really was. It wasn’t just about modernizing legacy systems through HealthTech or storing health records securely or encrypting data. It was about understanding what constitutes Protected Health Information, how to structure our vendor agreements, whether our cloud services were HIPAA-eligible, and if our product roadmap would trigger HITECH audit clauses down the line.
It’s at that moment that I realized: HealthTech regulations for CTOs is not something we bolt on after shipping. It’s something we architect for – from line one of code to the last vendor we onboard. As CTOs in the healthcare space, we’re not just building software but trust systems. Our technical decisions have real-world consequences: misconfigured S3 buckets can leak patient records, poor audit trails can get flagged by regulators, and overlooking HIPAA and HITECH regulations in healthcare can tank a partnership before it starts.
The regulatory landscape isn’t static either. From EHR mandates to the rising influence of FHIR APIs, and from cloud-native deployments to emerging GenAI models, the ground is constantly shifting. That’s why healthtech compliance for CTOs is no longer a siloed function – it’s a strategic pillar of modern product development.
In this piece, I’ll share how we’ve navigated the evolving world of US HealthTech regulations – what we got wrong, what we learned the hard way, and how we built a system that balances compliance, scalability, and innovation. Whether you’re starting from scratch or scaling a platform with tens of thousands of users, I hope this helps you see compliance not as a blocker – but as a framework for long-term success.
Before you scale, let’s stress-test your foundation against the realities of US HealthTech regulations.
How to Map the Regulatory Terrain – HIPAA, HITECH, and What’s Emerging
When I first sat down to design our compliance roadmap, the question I kept hearing from stakeholders was:
“Isn’t HIPAA enough?”
It’s a fair question – but for any CTO navigating healthtech compliance, the reality is far more layered.
Let’s start with the basics. For those outside the legal loop constantly, here’s a quick refresher on what HIPAA and HITECH are and what they cover.
HIPAA, established in 1996, is still the bedrock of US healthcare regulations for enterprise tech. It governs how Protected Health Information must be stored, accessed, and shared. For CTOs, HIPAA development translates into specific technical safeguards: data encryption (at rest and in transit), strict access controls, automatic logouts, audit logs, and disaster recovery plans.
But then comes HITECH – the Health Information Technology for Economic and Clinical Health Act. What many forget is that HITECH didn’t just reinforce HIPAA, it amplified the penalties for violations and demanded greater transparency around data breaches. It shifted enforcement from “best effort” to “prove it.” If you’re looking for HIPAA compliance, it’s incomplete without understanding how HITECH adds teeth to the whole framework.
Also Read: Appinventiv Launches Fortified Development Framework to Surpass HIPAA and HITECH Standards
That’s just the foundation, though. The regulatory terrain is moving fast – and CTOs building digital health products can’t afford to stand still.
Today, FHIR (Fast Healthcare Interoperability Resources) is no longer optional. It’s the standard for enabling API-based access to patient records across systems. If your product touches EHRs, supports patient-facing apps, or wants to connect to provider networks, FHIR compliance isn’t a nice-to-have – it’s mandatory.
Then you’ve got SMART on FHIR, which adds OAuth2-based security and app-level access control on top of FHIR. It’s what makes EHR integrations more secure and modular. Our team spent weeks getting SMART flows right – and the payoff was not just compliance, but seamless interoperability.
HL7 v2 and v3, DICOM (for imaging), and now the Trusted Exchange Framework and Common Agreement (TEFCA) are reshaping how national data exchanges will operate. If you’re dealing with clinical messaging, labs, or imaging, these standards aren’t fringe tech – they’re table stakes.
And let’s not forget the new variables in play.
With the rise of cloud-native applications, AI models trained on medical data, and blockchain experiments in patient consent, the risk surface is expanding. That’s why choosing the right HIPAA HITECH compliance solution has gone beyond hosting and encryption. Now, it includes things like runtime container security, zero-trust access control, AI explainability, and real-time auditability.
As a CTO, I have learned that healthtech compliance for CTOs isn’t just a checklist. It’s an evolving architecture. It’s about asking:
- How does our tech stack align with regulatory expectations?
- Are our APIs and cloud services HIPAA eligible – or just “secure sounding”?
- Can we pass a HITECH audit if the OCR shows up next quarter?
- Are we ready for TEFCA when the data sharing landscape goes national?
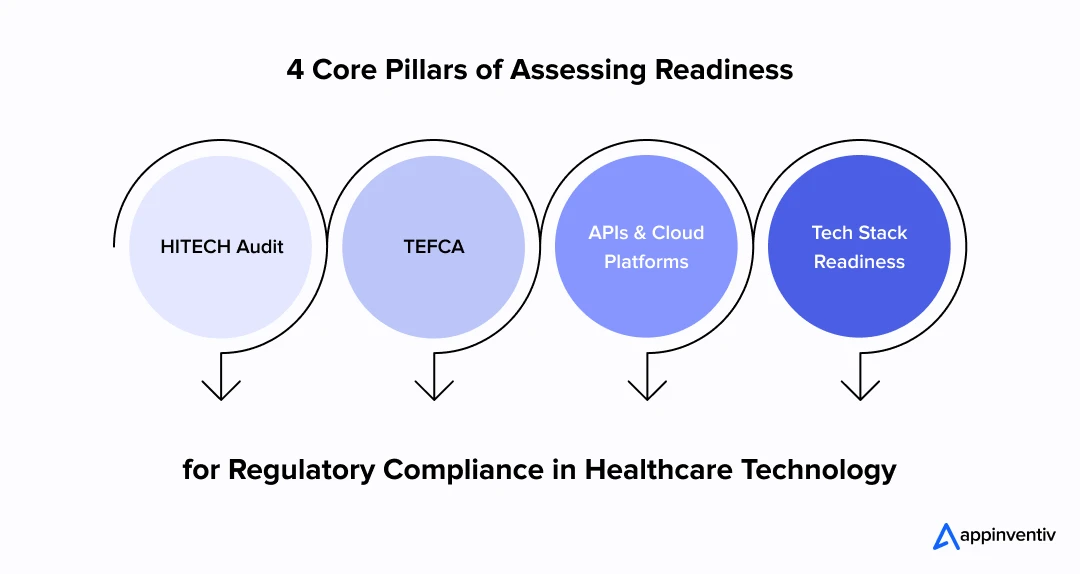
My advice? Don’t treat these frameworks as static documents. They are living blueprints – and your architecture needs to move with them.
Building the Foundation of a HealthTech Platform
When we started building our digital health platform, I knew right away: compliance can’t be layered on later. If you’re serious about meeting digital health app legal requirements in the USA, you have to start with privacy and security as foundational principles – not add-ons.
Privacy by design isn’t just a buzzword. For me, it’s decision architecture. It meant working closely with engineering, legal, and product teams from day one to map how data would move – and where risks could hide. It also meant saying no to speed shortcuts if they created blind spots in compliance.
What most people overlook is that compliance isn’t a feature – it’s a system-wide discipline.
The same mindset applies to building a HIPAA-aligned chiropractor clinic app, where intake, care plans, payments, and access controls need to be designed as one secure workflow.
We implemented encryption at both rest and transit across the board – not just for PHI, but for anything that could be traced back to a patient, clinician, or administrator. It doesn’t matter if it’s a lab result or a prescription reminder; in this ecosystem, it’s all sensitive.
Next came identity and access management. I’ll be honest – getting this right took longer than expected. But implementing granular role-based access, multi factor authentication, and session timeouts was non-negotiable. Because if your internal admin dashboard isn’t locked down tighter than your user-facing app, you’re building a breach vector.
We built secure APIs with rate limiting, authentication scopes, and internal service-to-service tokens – because compliance isn’t just about what users do; it’s also about how services talk to each other behind the curtain.
All of this sits under the umbrella of HIPAA and HITECH regulations in Healthcare – and those aren’t forgiving. For CTOs navigating this space, the HealthTech regulations demand a mindset shift: from “Can we protect this data?” to “What happens when we’re audited?”
I’ve seen teams try to retrofit compliance after MVP. It always costs more. Not just in money, but in lost trust, reengineering cycles, and sometimes reputational damage you can’t bounce back from.
So yes, the upfront investment in building security-first was higher. But it gave us the confidence to scale – to open our APIs to hospital partners, to pass third-party audits, and to grow without fear that a future regulation will break us.
If you’re a CTO in the healthcare space, think of compliance not as a checkbox – but as an engineering framework. You wouldn’t build a platform without CI/CD or observability, so don’t build it without embedded compliance either.
Let’s evaluate your foundation for compliance and scalability.
Data Transmission and Storage
One of the earliest lessons I learned as a CTO was this: data doesn’t just move – it travels through risk zones. And treating storage and transmission like backend plumbing is where many teams slip up. Under US healthcare regulations for enterprise, that kind of thinking just doesn’t cut it.
We built our architecture with HIPAA and HITECH regulations in healthcare compliance in mind from the start. That meant implementing both encryption in transit (TLS 1.3) and at rest (AES-256) – not as an afterthought, but as part of our core system design.
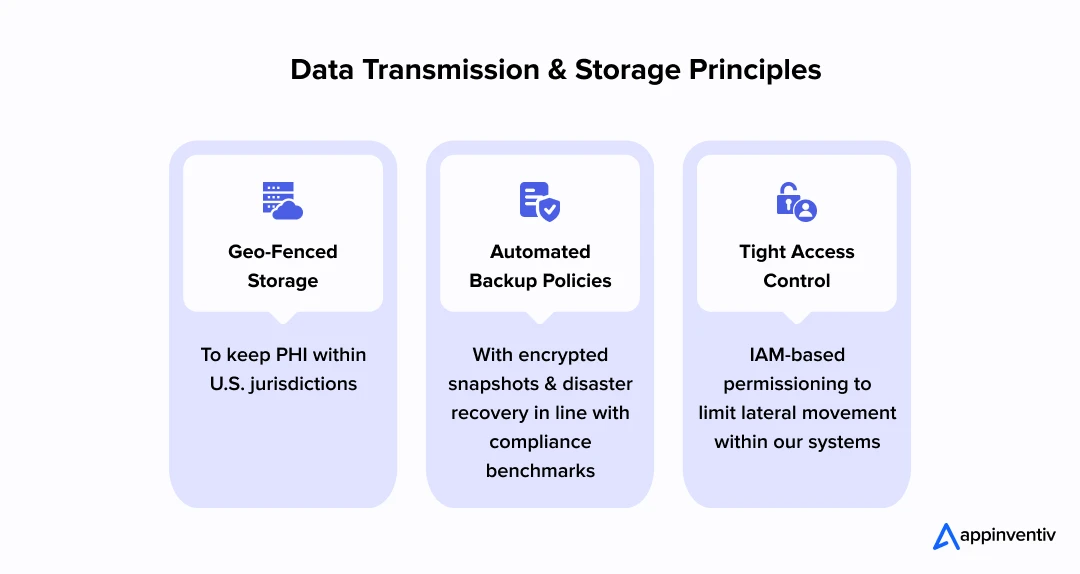
Instead of assuming our cloud provider had us covered, we vetted every service ourselves. AWS offers HIPAA-eligible services, yes – but eligibility isn’t automatic compliance. So, we set up:
- Geo-fenced storage to keep PHI within U.S. jurisdictions
- Automated backup policies with encrypted snapshots and disaster recovery in line with compliance benchmarks
- Tight access control and IAM-based permissioning to limit lateral movement within our systems
Data Transmission and Storage Principles
- Geo-fenced storage to keep PHI within U.S. jurisdictions
- Automated backup policies with encrypted snapshots and disaster recovery in line with compliance benchmarks
- Tight access control and IAM-based permissioning to limit lateral movement within our systems
That’s where HITECH vs HIPAA differences come into play. While HIPAA sets the security and privacy expectations, HITECH enforces them – often financially. And it’s often not the breach, but the audit trail (or lack thereof) that gets teams into trouble.
If you’re asking, “What are common implementation pitfalls CTOs should avoid?”, here’s my shortlist:
- Relying too heavily on vendor claims without your own compliance validation
- Forgetting to rotate encryption keys or enforce data access logging
- Treating backup policies like a devops checkbox instead of a regulatory requirement
Your HIPAA HITECH compliance solution can’t just be technically sound – it needs to be verifiable, reviewable, and designed to stand up to scrutiny. Because in the health data business, transparency is as critical as encryption.
How to Build a Culture of Security
Here’s something that doesn’t get said enough: your HIPAA HITECH compliance solution is only as strong as your most distracted employee. The cleanest codebase, the tightest encryption – none of it matters if someone clicks the wrong link or misrouted sensitive data via email.
As a CTO, I had to start thinking like a CISO – not just in crisis mode, but as we scaled the team and product. Compliance wasn’t just a checklist; it was a mindset we needed to embed from day one.
We made regular drills, phishing simulations, and awareness training non-negotiable. Yes, it slowed things down at times. But in healthcare, safety has to outrank speed.
I learned that HIPAA and HITECH compliance best practices for CTOs aren’t just technical. They’re cultural. We implemented:
- Role-based security briefings for every new hire, from engineering to customer success
- Quarterly refreshers that covered phishing, BYOD risks, password hygiene
- Cross-functional security ownership, so that it wasn’t just the dev team’s responsibility – product, ops, and support all had skin in the game
And we baked these into our digital health app legal requirements USA playbook, ensuring that our documentation, audit logs, and training records were always inspection-ready.
In hindsight, one of our biggest wins wasn’t a breakthrough in encryption or cloud infra – it was that every person on the team knew that handling patient data meant handling trust. And we treated that as our most critical architecture layer.
Third-Party Vendors: You’re Only as Compliant as Your Weakest Integration
In HealthTech, your stack is only as secure – and as compliant – as the no-name API you forgot to vet.
We learned this early. Our product relied on a mix of analytics tools, cloud infra, and communication layers. On paper, they were “HIPAA-aligned.” In practice? Some couldn’t produce a signed Business Associate Agreement for weeks – and a few couldn’t provide one at all.
In the world of HIPAA and HITECH regulations in healthcare, no BAA = no deal and if you’re navigating HealthTech regulations for CTOs, vendor due diligence becomes just as important as building secure code.
Here’s what our vendor vetting checklist evolved to include:
- SOC 2 Type II, ISO 27001, or HITRUST certifications
- Clear documentation on how PHI is handled – at rest, in transit, and at the edge
- BAAs signed before any code hits production, no matter how trivial the tool
- Transparent policies for breach notification and data retention
This wasn’t just about checking boxes for US HealthTech regulations – it was about making sure our trust chain wasn’t broken by a tool we used for convenience.
My advice to fellow CTOs of healthcare enterprises? Make compliance a procurement filter, not a retrofit. No shiny dashboard or LLM-enhanced chatbot is worth risking your platform’s integrity.
Before you plug in any LLM driven feature, it is worth understanding how enterprise generative AI in healthcare is being deployed safely across clinical and operational workflows
If you wouldn’t put unverified code into your EHR layer, don’t put unverified vendors into your PHI pipeline either.
Ways to Manage Monitoring, Vulnerability Management, and Incident Response
When you’re a CTO in healthtech, compliance doesn’t end at deployment-it starts getting tested the moment users log in. Systems evolve, codebases change, vendors update APIs, and attackers never stop scanning for soft spots. Healthtech compliance for CTOs is a moving target, and that’s exactly why proactive monitoring and structured incident response are not just good hygiene-they’re survival.
I still remember a moment early in our growth phase when a library vulnerability popped up on a weekend-ironically, just after we’d submitted a HIPAA audit packet. The exploit had no direct impact on our data layer, but because we were integrated with a third-party analytics plugin, the risk exposure had to be triaged immediately. We patched within 12 hours, but the real win was how quickly our HIPAA compliance guide for CTOs (yes, we maintain one internally) helped us walk through HIPAA compliance testing documentation, notify our legal team, and simulate the breach reporting flow-even though it wasn’t a reportable incident.
Here’s what we’ve learned to do differently ever since:
- Set up real-time alerting on access controls, unusual traffic, and API errors. Compliance isn’t just storage-it’s behavior monitoring.
- Maintain a single-pane compliance dashboard. Ours tracks patch status, vendor SOC 2 expirations, backup snapshots, and access logs-mapped directly to US HealthTech regulations.
- Run quarterly tabletop exercises. These aren’t just checkbox drills. We bring in product, engineering, legal, and support to simulate breaches, phishing attempts, or vendor compromise scenarios.
As CTOs, it’s easy to prioritize performance or shipping velocity. But in regulated spaces, compliance is performance-especially when things go sideways. Your incident response won’t just be judged by users. It’ll be judged by auditors.
Balancing Compliance with Innovation
As a CTO, I’m always walking a tightrope – on one side, the excitement of emerging tech like generative AI or blockchain for consent flows; on the other, the weight of compliance that never lets up. It’s not a one-off choice. It’s a constant, daily tradeoff between pushing boundaries and staying grounded in what the law allows.
Take AI/ML in diagnostics. The temptation to deploy models trained on large, diverse datasets is high-especially when early outputs look promising. But under HIPAA, that training data often includes Protected Health Information. Suddenly, what felt like an R&D initiative becomes a legal landmine. That’s why healthtech compliance for CTOs isn’t just about knowing the rules-it’s about anticipating how regulations evolve alongside technology.
A big part of this equation is understanding CTO responsibilities for health data security. When you’re deploying AI chatbots in patient portals or syncing wearables with real-time vitals, you’re dealing with PHI that’s moving across multiple environments. Security here can’t be reactive-it has to be architected into the product from day one.
We’ve found that one of the most common implementation pitfalls CTOs should avoid is treating compliance as a checklist that follows development. HIPAA lays out the basics for handling patient data: how it’s kept, who gets access, and how it’s shared. HITECH takes that further, adding sharper enforcement, especially around data breaches and third-party vendors. If you’re a CTO, this isn’t just a legal box to tick. It’s something that needs to influence how you architect your systems, choose cloud setups, and sign off on external tools.
Interoperability adds another layer. As we connect to HL7, FHIR, and TEFCA-compliant networks, we’re not just exchanging data-we’re sharing liability. A poorly scoped integration with a hospital’s legacy system can expose you to vulnerabilities no one flagged in the spec. That’s why we now audit every integration not just for technical fit, but for compliance impact as well.
Emerging technologies-like blockchain health ID, edge AI for diagnostics, and quantum-resistant encryption-promise the future. But that future will only be sustainable if built on a foundation that understands both security and law.
For CTOs, innovation isn’t just about what you build-it’s about what you protect while building it.
The right tech stack means nothing without the right safeguards.
Explore how we help healthcare enterprises scale innovation without regulatory risk.
How I Approach Compliance as a Trust Layer – Not a Bottleneck
If there’s one thing I’d tell any tech leader entering the US healthtech space, it’s this: compliance isn’t your enemy – it’s your foundation for long-term success.
Yes, at the surface level, HealthTech regulations for CTOs may seem like a maze of acronyms, legal clauses, and endless paperwork. But when you dig deeper, you’ll realize these guardrails force better architecture, cleaner code, tighter infrastructure, and most importantly – trust.
When we first started building in this space, HIPAA and HITECH regulations in Healthcare felt like constraints that slowed our sprint velocity. But over time, that mindset shifted. We started designing our stack and workflows around compliance from day one. And what emerged wasn’t just legally sound – it was structurally superior.
Every feature we roll out now – whether it’s data syncing, remote diagnostics, or ML-based triage – carries with it an embedded layer of assurance. Patients, providers, and partners don’t just use the systems; they trust them. And that’s a competitive edge that can’t be faked.
As a healthcare software development services company, this philosophy is the North Star for every project we undertake at Appinventiv. It’s the promise we make to every healthcare partner we work with. We don’t treat compliance as a feature to be bolted on at the end; we build it into the very fabric of your product—from the initial API architecture and data pipelines to vendor selection and the core product strategy.
Because regulations won’t stand still—they will shift, tighten, and expand. Our commitment is to engineer your systems with the flexibility to adapt. When your technology partner sees compliance as integral to product thinking, not just paperwork, your platform doesn’t just keep up with change; it leads the market. The companies that wait for an audit to find their flaws will always be playing catch-up.
Let’s schedule a call to understand your healthtech development and compliance requirements.
FAQs
Q. What should a CTO know about HIPAA and HITECH?
A. HIPAA protects patient data how it’s stored, accessed, and shared, HITECH builds on that by making enforcement stricter, especially around data breaches and vendor accountability. For a CTO, this means compliance isn’t a legal side note but something that needs to be considered in every system design, cloud setup, and third-party integration. If your stack touches health data, these two laws need to shape your architecture from day one
Q. What is the difference between HIPAA and the HITECH Act?
A. HIPAA lays out the rules for keeping patient health data private and secure. HITECH took those rules and made them stricter, adding heavier fines for non-compliance, requiring breach notifications, and making vendors just as responsible as healthcare providers. For HealthTech CTOs, it’s the difference between knowing the rules and being held fully accountable for following them.
Q. How does HITECH increase Business Associate responsibilities?
A. HITECH makes Business Associates like cloud storage providers or billing platforms directly responsible for protecting PHI. If they mess up, your company can still face the consequences unless there’s a proper agreement in place. That’s why CTOs need to be hands-on: review every partner, lock down Business Associate Agreements early, and check that they’re meeting compliance on an ongoing basis.
Q. What are the new proposed HIPAA Security Rule updates from HHS NPRM?
A. The HHS has proposed updates that reflect how healthcare tech works today, not how it worked a decade ago. They’re looking to clarify what a proper risk assessment actually looks like, tighten what counts as “minimum necessary” data use, and broaden breach notification requirements. If these changes pass, CTOs will need to take a hard look at their audit processes, documentation habits, and security controls especially with cloud platforms and AI now playing a bigger role in care delivery.
Q. How do you conduct a HIPAA risk assessment / compliance audit?
A. Start with a clear map: where does PHI live, who interacts with it, and where does it go? Once that is clearly laid out, look closely at every point – are the right safeguards in place? Are access levels tight enough? Any overlooked third-party tools? It’s less about following a template and more about stress-testing your real-world data flows for weak spots. Use tools like NIST’s risk framework or third-party compliance platforms. A proper audit should include technical safeguards, administrative policies, and a remediation plan – and it should be reviewed at least annually.
Q. Who is considered a Covered Entity vs. Business Associate under HIPAA/HITECH?
A. A Covered Entity is typically a healthcare provider, insurer, or clearinghouse that directly handles PHI. A Business Associate is any third-party service like a cloud vendor, billing system, or analytics platform that accesses or processes PHI on the entity’s behalf. For CTOs, the key is to correctly classify partners and ensure Business Associate Agreements are signed before any data is shared.


- In just 2 mins you will get a response
- Your idea is 100% protected by our Non Disclosure Agreement.
A Practical Guide to Building Your Mental Health Chatbot - Use Cases, Cost, & ROI
Key takeaways: Mental health chatbots work when they know their limits. They’re most useful as a gentle first step, not as a stand-in for real care. Good chatbot design is more about judgment than AI. Clear boundaries, calm responses, and safety matter more than smart language models. Enterprises invest in chatbots to make support easier…

How To Hire the Right Healthcare Developers As Per Your Business Needs?
Key Takeaways The guide to the step-by-step approach to recruiting the right healthcare software developers to meet your business requirements. In-depth dissection of the major technical skills, certifications and healthcare-specific expertise required in developers. Guidelines for carrying out the evaluation of candidates using portfolios, technical interviews, and trial projects. Industry-specific ERM approaches help address regulatory,…

Healthcare 4.0: Redefining the Future of Connected Care and Clinical Intelligence
Key Takeaways Healthcare 4.0's ecosystem is autonomous and patient-centric, integrating AI, IoT, and cloud computing. AI-driven clinical intelligence enhances personalized care for healthcare professionals and improves patient outcomes through predictive analytics. IoT and AI are being implemented in smart hospitals to improve operational efficiency, resource management, and patient care. Connected care enables better patient empowerment…