- The State of AI in Healthcare: Why 2025 Is the Year to Act
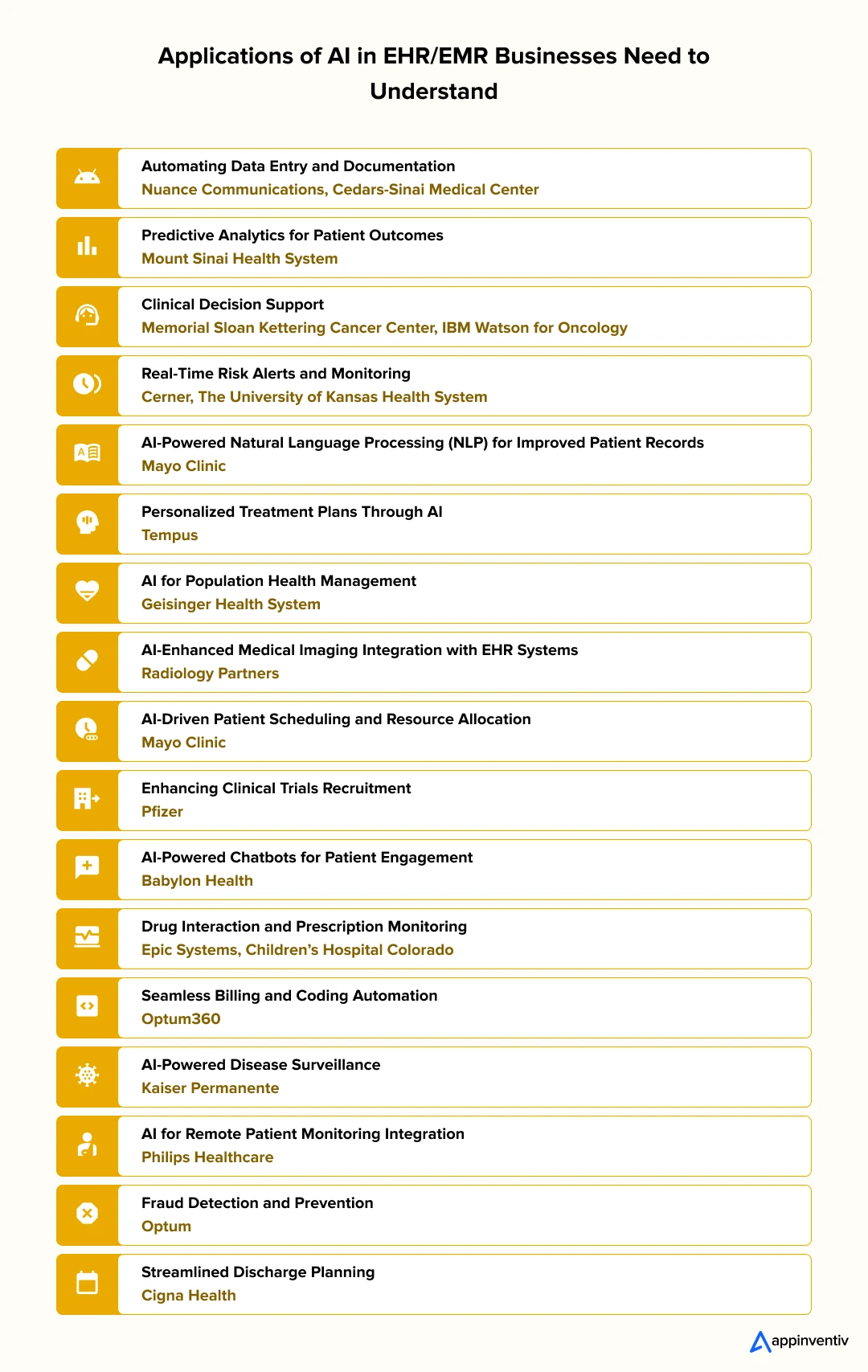
- Use Cases of AI in EHR/EMR: Automating Administrative Tasks to Providing Real-time Clinical Decision Support
- 1. Automating Data Entry and Documentation
- 2. Predictive Analytics for Patient Outcomes
- 3. Clinical Decision Support
- 4. Real-Time Risk Alerts and Monitoring
- 5. AI-Powered Natural Language Processing (NLP) for Improved Patient Records
- 6. Personalized Treatment Plans Through AI
- 7. AI for Population Health Management
- 8. AI-Enhanced Medical Imaging Integration with EHR Systems
- 9. AI-Driven Patient Scheduling and Resource Allocation
- 10. Enhancing Clinical Trials Recruitment
- 11. AI-Powered Chatbots for Patient Engagement
- 12. Drug Interaction and Prescription Monitoring
- 13. Seamless Billing and Coding Automation
- 14. AI-Powered Disease Surveillance
- 15. AI for Remote Patient Monitoring Integration
- 16. Fraud Detection and Prevention
- 17. Streamlined Discharge Planning
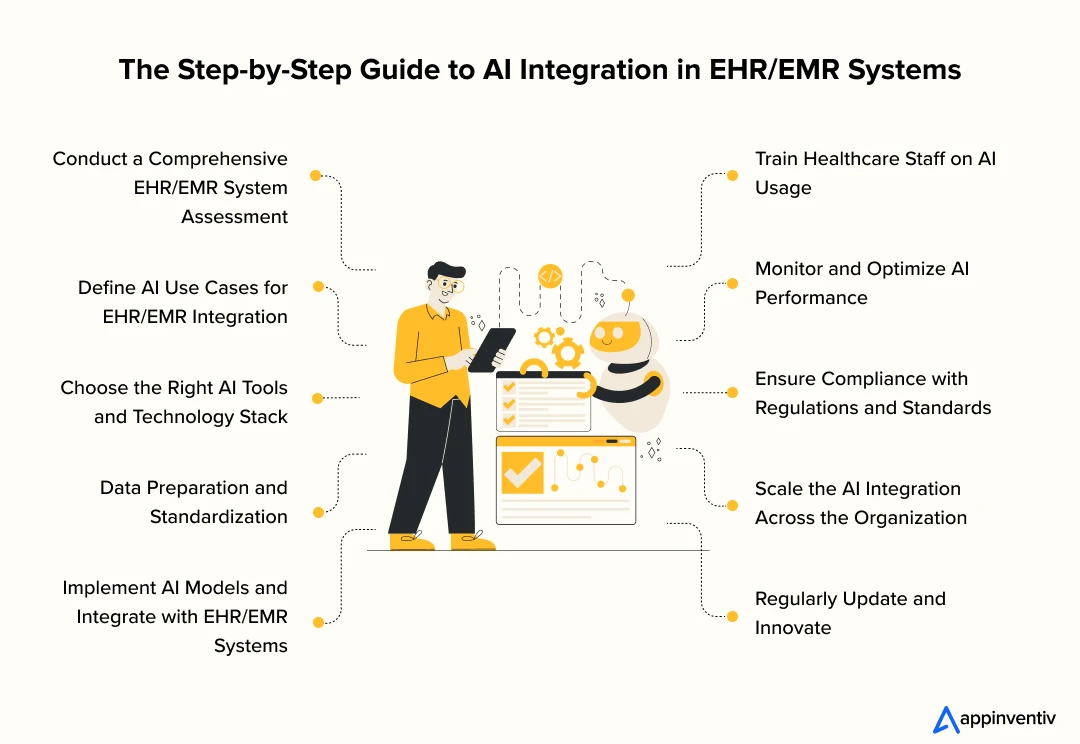
- The Step‑By‑Step AI in EHR/EMR Integration Guide
- 1. Conduct a Comprehensive EHR/EMR System Assessment
- 2. Define AI Use Cases for EHR/EMR Integration
- 3. Choose the Right AI Tools and Technology Stack
- 4. Data Preparation and Standardization
- 5. Implement AI Models and Integrate with EHR/EMR Systems
- 6. Train Healthcare Staff on AI Usage
- 7. Monitor and Optimize AI Performance
- 8. Ensure Compliance with Regulations and Standards
- 9. Scale the AI Integration Across the Organization
- 10. Regularly Update and Innovate
- Ensuring HIPAA Compliance and Data Security in AI Integration
- Technical Safeguards for PHI Protection
- PHI De-identification for AI Training
- Business Associate Agreements (BAAs)
- Interoperability Standards: HL7 & FHIR
- Understanding the Cost of Integrating AI in EHR/EMR Systems
- Challenges and Solutions in AI Integration with EHR/EMR Systems
- Addressing Bias in AI Models and Patient Data: A Must-Have for Responsible EHR Integration
- Where Does Bias in AI Come From?
- Real-World Risk: What Bias Looks Like in Practice
- How to Build Fair and Unbiased AI for EHR Systems
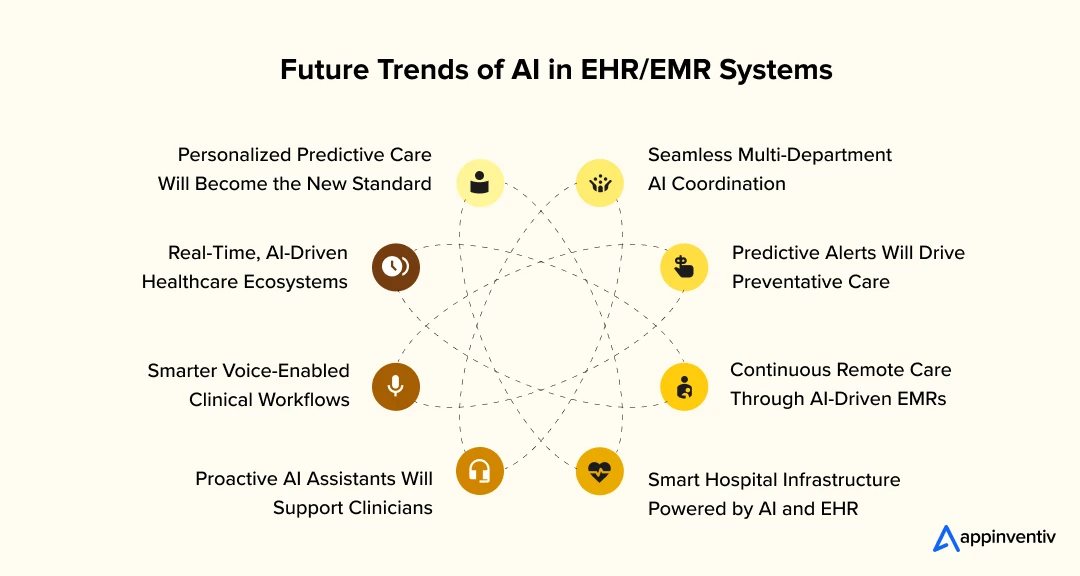
- Future Trends of AI in Electronic Health Records and Electronic Medical Records
- 1. Personalized Predictive Care Will Become the New Standard
- 2. Real-Time, AI-Driven Healthcare Ecosystems
- 3. Smarter Voice-Enabled Clinical Workflows
- 4. Proactive AI Agents Will Support Clinicians
- 5. Seamless Multi-Department AI Coordination
- 6. Predictive Alerts Will Drive Preventative Care
- 7. Continuous Remote Care Through AI-Driven EMRs
- 8. Smart Hospital Infrastructure Powered by AI and EHR
- Why Appinventiv is the Right Partner to Develop AI in EHR/EMR Powered Solutions
- FAQs
Key takeaways:
- Not adopting AI in EHR/EMR today risks falling behind.
- AI streamlines EHR workflows, cutting clinical and admin delays.
- Real-world hospitals are already seeing faster, smarter care with AI.
- Seamless AI integration needs system checks, data prep, and training.
- AI in EHR tackles real challenges like bias, cost, and compliance.
- Custom AI integration costs vary by use case, size, and integration depth.
- Future trends show AI will fully automate, personalize, and connect EHR systems.
Every healthcare leader knows the frustration: piles of paperwork, delayed records, and patient care slipping through the cracks due to manual inefficiencies. Despite all the advances in medical technology, Electronic Health Records (EHR) and Electronic Medical Records (EMR) systems often feel more like obstacles than solutions. These systems, intended to streamline operations, still leave teams bogged down in administrative tasks, creating more work instead of alleviating it.
This is where Artificial Intelligence (AI) steps in—no longer a distant possibility, but a current reality. As we move through 2025, the integration of AI into EHR/EMR systems, will push boundaries and achieve what was once unimaginable. It’s beyond automating tasks; it’s transforming the entire healthcare experience, offering real-time insights, predictive analytics, and dynamic data management that drives better decision-making and patient outcomes.
If you’re not leveraging AI in EHR/EMR systems today, you risk falling behind. We don’t think you want to struggle with outdated systems and drown in administrative overload while others are reaping the rewards of AI-driven efficiency. The stakes are too high, and the gap between those who adapt and those who don’t is widening by the day. The choice is clear: either embrace AI to revolutionize your EHR/EMR systems or risk falling behind in a rapidly advancing healthcare landscape.
In this blog, we’ll guide you through how AI is revolutionizing EHR/EMR integration, offering concrete steps, benefits, and potential hurdles. Get ready to discover why AI is not just an option, but a must-have for the future of healthcare operations.
The State of AI in Healthcare: Why 2025 Is the Year to Act
Electronic Health Records (EHR) and Electronic Medical Records (EMR) have long been the cornerstone of healthcare systems. These systems house vital patient data, facilitating clinical decision-making and improving overall care coordination. However, despite their critical role, many EHR and EMR systems still operate in silos, requiring manual data entry and offering limited real-time insights. This often leads to administrative burdens, delayed diagnoses, and potential gaps in patient care.
Now, AI is already becoming the norm, driving transformation across the board. Healthcare businesses who have already integrated AI have experienced significant improvements in the patient outcomes, the overall operational efficiency, and the cost savings. AI is shifting from being a supplementary technology to being a driving force in healthcare modernization.
Recent industry trends strongly highlight the rising importance of AI in healthcare, especially in transforming EHR and EMR systems, streamlining workflows, improving decision-making, and enhancing patient outcomes. McKinsey highlights that AI integration with healthcare systems could result in net savings of up to $360 billion annually by streamlining administrative processes and improving diagnostic accuracy. Deloitte also reports that 75% of top healthcare organizations are already exploring or preparing to scale Generative AI across their operations, all thanks to the vast potential of Generative AI to reduce inefficiencies and improve patient outcomes.
Additionally, PwC reveals that 77% of healthcare executives consider AI among their top three investment priorities followed by the Internet of Things (IoT), augmented reality (AR), and virtual reality (VR). Other important technologies like advanced robotics, blockchain, quantum computing, and neural interfaces were also part of their future plans.
The shift toward using AI to improve Electronic Health Records is not just about keeping up with technological advances; it’s about improving patient outcomes, enhancing operational efficiency, and staying ahead of the competition. As the healthcare sector embraces AI with EHR/EMR systems, the benefits of AI EHR will continue to grow, providing faster access to data, better clinical decisions, and reduced administrative costs.
Use Cases of AI in EHR/EMR: Automating Administrative Tasks to Providing Real-time Clinical Decision Support
The integration of AI into EHR/EMR systems has opened up a wide array of possibilities, transforming how healthcare providers manage and use patient data. As we explore the detailed use cases below, it’s clear that AI is no longer a futuristic concept but a key enabler of better patient care, streamlined operations, and cost reductions. From automating administrative tasks to providing real-time clinical decision support, AI EHR systems are revolutionizing healthcare operations.
1. Automating Data Entry and Documentation
One of the most time-consuming aspects of EHR systems is manual data entry. Healthcare professionals often spend a significant amount of time inputting patient data, making the process prone to errors and delays. AI in EHR systems can automate data entry by extracting information from patient records, clinical notes, and even voice inputs using natural language processing (NLP) in healthcare systems. This reduces human error, enhances efficiency, and allows healthcare providers to focus on patient care rather than administrative tasks.
Real-World Example: Nuance Communications has integrated AI-driven voice recognition and NLP technology with their EHR systems at several hospitals, including Cedars-Sinai Medical Center. The system automatically transcribes and organizes doctor-patient interactions, reducing the time spent on documentation by more than 50%. This has significantly improved workflow and efficiency, enabling clinicians to spend more time with patients.
2. Predictive Analytics for Patient Outcomes
AI can analyze vast amounts of patient data from EHR/EMR systems to predict future health risks, such as the likelihood of disease progression, readmission, or complications. By identifying at-risk patients early, healthcare providers can intervene before conditions worsen, improving patient outcomes and reducing healthcare costs. AI-powered predictive analytics can help hospitals optimize resource allocation and prioritize high-risk patients for timely intervention.
Real-World Example: Mount Sinai Health System in New York has implemented AI to predict patient readmissions within 30 days using data from their EHR systems. By leveraging AI algorithms, they can flag patients at high risk of readmission, allowing them to proactively address potential issues. This initiative has led to a 20% reduction in readmission rates, improving both patient outcomes and operational efficiency.
3. Clinical Decision Support
AI-powered clinical decision support tools embedded in EHR/EMR systems can assist healthcare providers in making evidence-based decisions. These tools analyze patient data, medical histories, and the latest research to offer recommendations on diagnosis, treatment options, and medication management. By providing clinicians with actionable insights, AI enhances the accuracy of clinical decisions, reduces diagnostic errors, and helps optimize patient care.
Real-World Example: Memorial Sloan Kettering Cancer Center used IBM Watson for Oncology to analyze cancer patients’ medical records and provide oncologists with personalized treatment recommendations based on vast amounts of medical literature. This integration helped doctors make more informed decisions, improving patient outcomes.
4. Real-Time Risk Alerts and Monitoring
AI in EMR systems can provide real-time alerts and monitoring for high-risk patients. By continuously analyzing data such as vital signs, lab results, and medication, AI can flag any abnormalities or changes in a patient’s condition that may require immediate attention. This proactive monitoring allows healthcare providers to intervene early and prevent adverse events, enhancing patient safety and reducing healthcare costs.
Real-World Example: Cerner has integrated AI-driven real-time monitoring into its EHR systems at The University of Kansas Health System. The system continuously analyzes patient data and alerts healthcare providers to any critical changes, such as sudden drops in blood pressure or oxygen levels. This has led to quicker interventions and a reduction in the incidence of preventable complications, such as sepsis.
5. AI-Powered Natural Language Processing (NLP) for Improved Patient Records
One of the challenges with EHR systems is that a large amount of clinical data is often unstructured, existing in the form of free text or voice notes. AI and NLP can extract valuable insights from these unstructured data sources, making it easier to categorize, analyze, and retrieve relevant information from patient records. This improves the quality of data in EHR/EMR systems, enabling better decision-making and more accurate documentation.
Real-World Example: Mayo Clinic has implemented AI and NLP technology to improve the accuracy of patient records in their EHR systems. Using NLP, the clinic can extract key information from clinical notes, enabling faster and more accurate diagnoses. This use of AI has not only improved the quality of their patient records but also enhanced their ability to deliver personalized care.
6. Personalized Treatment Plans Through AI
Artificial intelligence for EHR systems can help develop personalized treatment plans by analyzing a patient’s medical history, genetic information, lifestyle data, and the latest clinical research. By tailoring treatment plans to individual patients, AI can help optimize care and improve outcomes. This personalized approach also allows for better management of chronic conditions and the reduction of adverse reactions to medications.
Real-World Example: Tempus has integrated AI and machine learning with EHR systems to provide personalized cancer treatment recommendations. By analyzing a patient’s genetic profile and treatment history, the platform offers oncologists customized treatment options, leading to more effective and targeted therapies. Tempus’s AI-driven insights have helped clinicians deliver more precise and successful treatments.
7. AI for Population Health Management
AI can aggregate data from multiple EHR/EMR systems to identify trends and patterns in patient populations, such as the prevalence of certain conditions, risk factors, and social determinants of health. This enables healthcare organizations to develop strategies for improving public health, reducing health disparities, and managing population health more effectively. AI in population health management also allows for better resource allocation and more targeted healthcare interventions.
[Also Read: 10 Use Cases on How AI is Transforming Genomics]
Real-World Example: Geisinger Health System uses AI in its EHR system to monitor population health and identify at-risk groups. By analyzing data on patients’ medical history, socioeconomic status, and lifestyle factors, Geisinger is able to provide tailored care to at-risk populations, improving health outcomes and reducing unnecessary hospitalizations.
8. AI-Enhanced Medical Imaging Integration with EHR Systems
AI’s ability to analyze medical images, such as X-rays, MRIs, and CT scans, has greatly improved diagnostic accuracy. By integrating AI-powered image recognition with EHR/EMR systems, healthcare providers can quickly access and analyze medical images alongside patient data. This integration allows for faster, more accurate diagnoses and ensures that patients receive the right treatment without unnecessary delays.
Real-World Example: Radiology Partners, the largest physician-led radiology practice in the U.S., uses AI to assist in reading and interpreting medical images. The AI system is integrated with their EHR, enabling radiologists to quickly identify issues like tumors or fractures in medical images, leading to faster diagnosis and treatment. This integration has significantly reduced turnaround times for diagnostic results and improved patient care.
9. AI-Driven Patient Scheduling and Resource Allocation
AI-powered systems in EHR/EMR platforms are being used to optimize patient scheduling and resource allocation. By analyzing historical data and predicting demand, AI can suggest the best times for appointments, manage waitlists, and even adjust resources dynamically based on patient volume. This optimization reduces patient wait times, prevents overbooking, and maximizes the use of healthcare facilities.
Real-World Example: Mayo Clinic is also using AI to improve electronic health records. The organization has adopted AI-driven scheduling tools in their EHR system to optimize patient flow. By analyzing patient history, availability, and clinician schedules, the AI suggests the best appointment times, ensuring that resources are used efficiently. This has decreased appointment cancellations by 15% and improved patient satisfaction by streamlining scheduling processes.
10. Enhancing Clinical Trials Recruitment
AI can be used to streamline the recruitment process for clinical trials by analyzing EHR/EMR data to match patients with relevant trials. By quickly identifying eligible candidates based on their medical histories, conditions, and other criteria, AI can accelerate the recruitment process and ensure that trials are better aligned with patient needs.
Real-World Example: Pfizer uses AI to analyze patient data within EHR/EMR systems for clinical trial recruitment. By cross-referencing patient records with trial criteria, Pfizer has been able to match eligible participants faster, improving the efficiency of its clinical trials and reducing recruitment time by up to 25%.
11. AI-Powered Chatbots for Patient Engagement
AI chatbots integrated with EHR/EMR systems are increasingly being used to improve patient engagement. These bots can answer questions, provide appointment reminders, and even collect patient information prior to visits. They also assist in triaging symptoms and offering health advice, allowing healthcare providers to focus on more complex patient concerns.
Real-World Example: Babylon Health employs AI-powered chatbots integrated with its EHR systems to provide virtual consultations and health information. The chatbot guides patients through symptom checkers, schedules appointments, and directs them to the appropriate healthcare professionals, enhancing both patient engagement and the efficiency of the healthcare process.
12. Drug Interaction and Prescription Monitoring
AI EHR systems can analyze patient records to identify potential drug interactions and flag medication errors in real-time. By cross-referencing prescriptions with the patient’s medical history, AI can alert healthcare providers to harmful interactions, allergies, or contraindications, reducing medication errors and improving patient safety.
Real-World Example: Epic Systems has integrated AI-driven prescription monitoring in their EHR system. At Children’s Hospital Colorado, the system detects potential drug interactions by scanning the entire patient’s prescription history, lab results, and allergies. This has significantly reduced the incidence of adverse drug reactions and improved medication safety for pediatric patients.
13. Seamless Billing and Coding Automation
AI can automate the process of medical billing and coding, which is a time-consuming task that often involves manual verification and error correction. AI-powered systems can automatically assign the correct codes to medical procedures and diagnoses by analyzing patient data in the EHR system. This increases the accuracy of billing, accelerates reimbursement, and reduces administrative costs.
Real-World Example: Optum360 has integrated AI with EHR systems to streamline the coding and billing process for healthcare providers. By using AI to automate the assignment of ICD-10 codes and procedural codes, the company has reduced errors in billing by 20% and improved claims processing time, leading to faster reimbursements.
14. AI-Powered Disease Surveillance
AI can help monitor and track disease outbreaks by analyzing patient data from EHR/EMR systems. By detecting patterns of symptoms, AI can identify emerging diseases or outbreaks in real-time, providing healthcare providers with the information needed to respond quickly and allocate resources accordingly. This proactive approach can significantly enhance public health management.
Real-World Example: Kaiser Permanente, one of the largest integrated health systems in the United States, leverages its vast electronic medical-record database and in-house machine-learning models to spot unusual spikes in flu-like or respiratory symptoms across its member population. When the AI engine flags a clustering pattern at certain clinics, the public-health team receives an alert within hours, enabling them to speed up testing, shift vaccine supplies, and coordinate outreach in the affected neighborhoodsneighbourhoods—often days before standard reporting channels would raise the same alarm.
15. AI for Remote Patient Monitoring Integration
With the growing popularity of telehealth, integrating Artificial intelligence intofor EHR systems allows for real-time monitoring of patients’ vital signs, especially for those with chronic conditions. AI can analyze data from wearables and other remote monitoring devices, alerting healthcare providers to significant changes that may require immediate attention.
Real-World Example: Philips Healthcare uses AI to analyze data from remote patient monitoring devices integrated with EHR/EMR systems. By monitoring chronic disease patients in real-time, Philips has helped healthcare providers detect early signs of exacerbation, enabling them to intervene before patients require hospitalization. This has improved patient outcomes and reduced hospital admissions for chronic conditions.
16. Fraud Detection and Prevention
AI in EHR/EMR systems can help detect fraudulent activity by analyzing patterns in billing and patient records. Machine learning algorithms can identify inconsistencies, such as duplicate claims or suspicious billing practices, and flag them for review. This ensures that healthcare organizations maintain compliance and protect against financial fraud.
[Also Read: 10 Use Cases and Benefits of AI in Medical Billing]
Real-World Example: Optum uses AI-powered fraud detection tools within its EHR system to identify suspicious billing patterns. By analyzing billing codes, patient data, and healthcare provider activities, the system flags potential fraud, allowing the company to take immediate action. This has reduced fraudulent claims and improved financial security for healthcare providers.
17. Streamlined Discharge Planning
AI in EHR/EMR systems can be used to improve discharge planning by analyzing patient data and predicting the level of care needed after hospital discharge. AI can suggest discharge instructions, follow-up appointments, and home care needs based on the patient’s condition, ensuring that patients receive appropriate care after they leave the hospital.
Real-World Example: Cigna Health has implemented AI in their EHR system to optimize discharge planning. By analyzing data from the patient’s hospital stay, the system recommends follow-up care and at-home support, ensuring that patients receive the necessary care after discharge. This approach has helped reduce readmission rates and improved overall patient satisfaction.
The Step‑By‑Step AI in EHR/EMR Integration Guide
Integrating AI into EHR/EMR systems is a transformative journey that can enhance healthcare delivery, streamline operations, and improve patient outcomes. Below is a detailed step-by-step guide to successfully integrate AI with your EHR/EMR system.
1. Conduct a Comprehensive EHR/EMR System Assessment
Before integrating AI, it is essential to assess your current EHR/EMR system to understand its strengths and limitations. This step helps to identify pain points that AI can address, such as automating data entry, enhancing clinical decision support, or enabling predictive analytics.
What It Does:
- Evaluates the current capabilities of your EHR/EMR system
- Identifies areas for improvement and how AI can add value
- Helps ensure compatibility with AI solutions
- Addresses data privacy and compliance requirements
2. Define AI Use Cases for EHR/EMR Integration
Once the assessment is complete, the next step is to define the AI use cases that align with your organization’s goals. Use cases may include automating administrative tasks, predictive analytics for patient outcomes, or providing clinical decision support.
What It Does:
- Clarifies the specific AI-driven goals for the organization
- Ensures alignment of AI tools with the healthcare provider’s needs
- Helps prioritize AI initiatives based on impact
- Determines the resources required for each use case
3. Choose the Right AI Tools and Technology Stack
This step involves selecting the right AI tools and technology stack that are compatible with your EHR/EMR systems. It is important to choose AI solutions with a proven track record in healthcare and that meet your technical and regulatory requirements.
What It Does:
- Ensures compatibility between AI tools and existing EHR/EMR systems
- Identifies trusted vendors with experience in healthcare AI
- Aligns AI solutions with your technological infrastructure
- Guarantees compliance with privacy and regulatory standards
4. Data Preparation and Standardization
AI models require clean, structured, and standardized data to be effective. This step focuses on preparing the data by cleaning it, ensuring consistency, and converting unstructured data into a usable format. Standardizing data ensures interoperability with other systems and AI tools.
What It Does:
- Ensures that data is accurate, complete, and properly formatted
- Standardizes data to meet healthcare data exchange standards (e.g., FHIR, HL7)
- Prepares unstructured data for AI analysis
- Addresses missing data through data augmentation or enrichment
5. Implement AI Models and Integrate with EHR/EMR Systems
With the data prepared, AI models are implemented and integrated into the EHR/EMR system. This process ensures that AI tools, such as predictive analytics or decision support, are embedded within the existing system, allowing them to interact with patient data and provide insights in real-time.
What It Does:
- Integrates AI models directly into clinical workflows
- Embeds predictive and decision support tools into EHR/EMR systems
- Enables AI-driven analysis of patient data for actionable insights
- Ensures seamless interaction between AI tools and EHR/EMR user interfaces
6. Train Healthcare Staff on AI Usage
Training healthcare professionals on how to use AI-powered tools is critical to ensure that the integration is successful. This step focuses on educating staff about how to interpret AI-driven recommendations and incorporate them into their daily workflows.
What It Does:
- Provides healthcare providers with the knowledge to effectively use AI tools
- Helps clinicians understand AI recommendations and insights
- Improves adoption rates by familiarizing staff with new technologies
- Enhances the confidence of clinicians in using AI for clinical decision-making
7. Monitor and Optimize AI Performance
AI systems require continuous monitoring to ensure that they perform effectively and provide accurate recommendations. This step focuses on tracking the performance of AI tools, identifying areas for improvement, and optimizing models for better results.
What It Does:
- Tracks the performance and accuracy of AI-driven outputs
- Identifies and addresses issues such as errors or biases in AI predictions
- Continuously updates AI models to incorporate new data and research
- Optimizes AI tools to align with evolving clinical needs and goals
8. Ensure Compliance with Regulations and Standards
AI systems in healthcare must adhere to various regulations, including HIPAA in the U.S. This step ensures that AI integration complies with all relevant data privacy and security standards.
What It Does:
- Ensures that AI models comply with privacy regulations like HIPAA and GDPR
- Implements encryption protocols to secure patient data processed by AI
- Regularly audits AI systems for compliance with healthcare regulations
- Maintains transparency and accountability in AI usage for patient data
9. Scale the AI Integration Across the Organization
Once AI integration has been successfully implemented in one department or use case, the next step is to scale the technology across the entire organization. This includes expanding AI tools to other specialties, departments, or patient populations.
What It Does:
- Expands AI usage across different clinical specialties or care settings
- Ensures that AI-driven tools are accessible organization-wide
- Provides support for scaling AI tools to additional departments
- Ensures consistency in AI-driven processes across the organization
10. Regularly Update and Innovate
AI technology is constantly evolving, and it’s crucial to keep your AI models and tools up to date. This step involves staying informed about the latest AI advancements, regularly updating AI models, and fostering a culture of innovation.
What It Does:
- Ensures that AI tools are up to date with the latest technology advancements
- Incorporates new data, research, and clinical guidelines into AI models
- Encourages continuous improvement and innovation in AI solutions
- Ensures long-term relevance and effectiveness of AI tools in healthcare operations
Ensuring HIPAA Compliance and Data Security in AI Integration
When integrating AI into EHR/EMR systems, ensuring HIPAA compliance and protecting Protected Health Information (PHI) is non-negotiable. AI solutions process vast amounts of sensitive patient data—any misstep can lead to legal issues, reputational damage, and patient distrust. Here’s how to secure your AI-powered healthcare infrastructure while meeting all U.S. regulatory standards:
Technical Safeguards for PHI Protection
Healthcare organizations must implement robust technical controls that align with HIPAA’s Security Rule.
- Access Controls: Restrict data access based on roles. Implement multifactor authentication (MFA) and session timeouts for all users interacting with EHR-AI systems.
- Data Encryption: Encrypt PHI both at rest and in transit using AES-256 or TLS 1.2+ protocols to prevent unauthorized interception or breaches.
- Audit Logs: Maintain detailed logs of all system activity, including who accessed patient data, when, and for what purpose. These logs are essential for compliance audits and breach forensics.
PHI De-identification for AI Training
AI models often need real patient data for training, which introduces compliance risks. To mitigate this:
- De-identify PHI following HIPAA’s Safe Harbor method—remove all 18 identifiers (e.g., names, dates, medical record numbers).
- Use synthetic data where feasible to train AI models without exposing actual PHI.
- Maintain data lineage to ensure de-identified data cannot be reverse-engineered.
Business Associate Agreements (BAAs)
Every third-party tech partner involved in storing, processing, or transmitting PHI must sign a Business Associate Agreement.
- Ensure your AI and cloud vendors understand and adhere to HIPAA regulations.
- Your BAA should define responsibilities around breach notification, security practices, and termination procedures.
- Appinventiv, as your technology partner, signs BAAs and adheres to strict HIPAA protocols during the entire AI implementation lifecycle.
Interoperability Standards: HL7 & FHIR
AI integration must support seamless data exchange with other health IT systems. That’s only possible through adherence to interoperability standards like:
- HL7 (Health Level Seven): Facilitates structured data exchange between EHRs, labs, and imaging systems.
- FHIR (Fast Healthcare Interoperability Resources): A modern API-driven standard that enables real-time data access and exchange across devices and platforms.
Supporting HL7 and FHIR ensures your AI tools work across your entire digital health ecosystem, from diagnostics to discharge.
Understanding the Cost of Integrating AI in EHR/EMR Systems
The cost of integrating AI in EHR/EMR systems typically ranges from $50,000 to $500,000 or more, depending on various factors. The cost variation depends on the size of the organization, the complexity of the AI use cases in EHR, and the customization required for integration. Here’s a quick look at the key factors affecting cost of AI EHR/EMR software:
1. Size and Scale of the Organization
Larger organizations require more extensive AI integration, leading to higher costs due to more complex systems and wider deployment needs.
2. Complexity of AI Use Cases
Advanced AI-powered solutions in EHR, like predictive analytics or clinical decision support, typically cost more than simple tasks such as automating data entry.
3. Customization and Integration Needs
Customizing AI tools for EMR systems to meet specific organizational requirements and integrating them with existing workflows can drive up costs.
4. Data Preparation and Standardization
Preparing and structuring data for AI models in EHR/EMR systems requires additional resources, especially for unstructured data, increasing the overall cost.
5. AI Tool Selection and Vendor Costs
The choice between pre-built solutions and custom-built AI models for EMR/AI integration will affect pricing, with premium vendors often coming at a higher cost.
6. Training and Change Management
Training staff on using AI-driven EHR systems and managing the transition can add to the cost, ensuring smooth adoption and reducing resistance.
7. Ongoing Maintenance and Updates
AI models require continuous updates and maintenance, particularly as new data flows into the EHR systems, leading to additional costs over time.
8. Compliance and Security
Meeting HIPAA compliance and ensuring data security are essential for AI EMR systems, adding extra expenses for encryption and audits.
Challenges and Solutions in AI Integration with EHR/EMR Systems
Integrating AI into EHR/EMR systems brings tremendous benefits, but it also presents a series of challenges that need to be addressed for a successful implementation. Below is a detailed breakdown of common challenges and limitations of AI EMR and EHR software solutions:
| Challenge | What It Means | How Businesses Can Solve It |
|---|---|---|
| Data Quality and Standardization Issues | The success of AI in EHR systems depends on the quality and structure of the data it processes. Unstructured, fragmented, or incomplete data can hinder the effectiveness of AI models in EMR systems. | Businesses should invest in robust data cleaning, standardization, and normalization strategies. Utilizing Natural Language Processing (NLP) can help convert unstructured data into structured formats, ensuring compatibility with AI EMR tools. Adhering to standards like FHIR and HL7 ensures seamless integration with other healthcare systems and improved AI output. |
| Data Privacy and Compliance Concerns | The use of AI with EHR/EMR systems requires handling sensitive patient data, raising concerns about compliance with privacy regulations such as HIPAA and GDPR. Mishandling can lead to legal issues. | Businesses must implement strict data encryption protocols, access control systems, and privacy measures to comply with HIPAA and GDPR. Integrating AI in EMR systems that adhere to these regulations and conducting regular audits ensures that patient data is handled securely and within legal boundaries. |
| Integration Complexity with Legacy Systems | Many healthcare organizations still rely on outdated EHR/EMR systems that may not be compatible with modern AI-driven technologies. This makes AI integration with EHR systems challenging and complex. | Healthcare businesses should choose AI in EHR solutions with flexible, modular architectures and robust API-based integration options. In some cases, upgrading legacy systems to support AI EMR tools may be necessary, or businesses can consider cloud-based AI solutions to bypass legacy system limitations. |
| Clinical Adoption and Trust in AI | Clinicians may be skeptical about the accuracy and reliability of AI-powered clinical decision support tools within EHR systems, leading to hesitation in adopting AI tools for clinical decisions with AI in EHR systems. | To foster trust, businesses should involve healthcare providers early in the process, providing evidence of AI use cases in EHR through pilot projects. Offering extensive training and demonstrating AI-driven clinical decision support’s ability to enhance clinical decision-making rather than replace human expertise helps increase trust and adoption. |
| Bias in AI Models and Data | AI in EMR systems can inherit biases from the data they are trained on, leading to skewed results and potentially affecting underrepresented patient populations. | Businesses should ensure their AI in EHR models are trained on diverse, representative datasets that reflect the demographics of the patient population. Regular audits should be conducted to identify and address biases (training data can perpetuate racial or socioeconomic biases), and ensure responsibility. AI models in EHR systems should be adjusted to improve fairness in decision-making. |
| Cost and Resource Constraints | The financial and resource requirements to integrate AI in EHR systems can be significant, especially for smaller healthcare organizations with limited budgets. | Businesses can adopt a phased approach, starting with high-impact areas such as AI-powered clinical decision support or predictive analytics for patient outcomes. Leveraging cloud-based AI in EMR systems reduces infrastructure costs, while choosing AI vendors with affordable pricing models and subscription-based services can spread out expenses. |
| AI Model Transparency and Explainability | AI in EHR systems may sometimes function as a “black box,” with recommendations that are not fully understood or explained, leading to concerns over the reliability of AI-driven clinical decisions. | To improve transparency, businesses should focus on developing explainable AI models that offer clear, understandable reasons behind the AI-driven recommendations in clinical decisions with AI in EHR systems. Implementing explainable AI (XAI) systems helps clinicians better understand how AI models arrive at their decisions, thereby improving trust in the system. |
| Interoperability with External Systems | Healthcare organizations often use multiple systems (e.g., lab management, imaging), and seamless data flow between these systems is essential for comprehensive patient care. | Ensure AI EMR systems support healthcare interoperability through standards like HL7. Implementing AI with EHR/EMR systems that are designed to communicate effectively with other platforms ensures a seamless exchange of patient data, improving care coordination and reducing inefficiencies in healthcare delivery. |
| Managing the Change and Resistance | Integrating AI into clinical workflows can lead to resistance from staff due to fears of disrupting established procedures or replacing human jobs. | Overcome resistance by offering clear communication about how AI in EMR tools will enhance, not replace, clinical workflows. Provide evidence of AI’s ability to reduce administrative burden and improve patient outcomes. Involve clinicians in the AI adoption process, offering training and feedback loops to foster a sense of ownership and acceptance. |
| Scalability of AI Solutions | Scaling AI integration across a large healthcare system or multiple departments can be complex, requiring significant coordination and resource allocation. | Start with scalable, modular tools for AI and EHR that can be implemented in high-priority areas like predictive analytics or documentation automation. Once AI models prove effective in one area, they can be expanded to other departments. Cloud-based solutions can also help businesses scale their AI implementation efficiently without the need for heavy infrastructure investments. |
Addressing Bias in AI Models and Patient Data: A Must-Have for Responsible EHR Integration
Bias in AI is more than a technical flaw—it’s a direct threat to equitable patient care and clinical credibility. When it comes to AI-powered EHR/EMR systems, biased models can lead to misdiagnosis, delayed treatments, and exclusion of underserved communities. For healthcare leaders, addressing bias is not just an ethical imperative—it’s a strategic necessity.
Where Does Bias in AI Come From?
Bias in EHR-integrated AI typically originates from three key areas:
- Historical Data Skews: If your training data mostly includes patients from a specific demographic (e.g., urban, white, male), your AI model will generalize care decisions toward that group—neglecting others.
- Labeling and Annotation Errors: Clinician-generated notes and diagnosis labels can include subjective opinions, which the AI may interpret as clinical truth.
- Structural and Societal Biases: Broader healthcare disparities—like unequal access to care—can be encoded in datasets, reinforcing inequalities when AI models learn from them.
Real-World Risk: What Bias Looks Like in Practice
An AI model trained primarily on male cardiovascular data might underdiagnose heart disease in women. Similarly, a risk-scoring algorithm trained on cost-of-care data might rank low-income patients as lower-risk simply because they historically received less care—not because they were actually healthier.
[Also Read: Preventing AI Model Collapse: Addressing the Inherent Risk of Synthetic Datasets]
How to Build Fair and Unbiased AI for EHR Systems
To ensure fairness in AI-powered EHR/EMR systems, organizations must follow a proactive and repeatable framework:
1. Data Diversity and Representation
- Collect and use training datasets that reflect demographic diversity, including ethnicity, age, gender, socioeconomic background, and geography.
- Partner with data providers that offer curated, demographically inclusive datasets tailored for healthcare AI.
2. Bias Auditing and Fairness Testing
- Regularly audit your AI models for disparate impact—measure accuracy and outcomes across subgroups.
- Use fairness metrics like equalized odds, demographic parity, and false negative/positive rates to uncover hidden discrepancies.
3. Bias Mitigation Techniques
- Apply re-sampling or re-weighting during training to balance data representation.
- Use adversarial debiasing algorithms to minimize sensitive attribute influence (e.g., race or gender) on predictions.
- Apply counterfactual testing—checking how a prediction would change if only a protected attribute (like race) were altered.
4. Transparent and Explainable AI (XAI)
- Integrate explainable AI tools like SHAP or LIME to show how predictions were made and ensure clinicians can interpret model outputs with confidence.
- Transparency boosts clinical trust and also helps reveal hidden biases in decision pathways.
5. Continuous Monitoring in Real-World Settings
- Post-deployment, monitor outcomes continuously to detect real-world bias emergence.
- Set up feedback loops where clinicians can flag suspicious outputs, which can inform retraining or model updates.
Future Trends of AI in Electronic Health Records and Electronic Medical Records
The integration of AI in Electronic Health Records (EHR) and Electronic Medical Records (EMR) is just the beginning. As AI technology continues to evolve, its role in healthcare will expand, transforming EHR/EMR systems into even more powerful, proactive tools. Here are some key future trends shaping AI in EHR/EMR systems.
1. Personalized Predictive Care Will Become the New Standard
Future AI EHR systems will go beyond basic predictions to offer hyper-personalized care journeys. By continuously learning from patient data, AI and EHR platforms will provide highly specific risk alerts and treatment plans tailored to individual needs.
2. Real-Time, AI-Driven Healthcare Ecosystems
The future of AI in EHR will focus on creating real-time, fully connected healthcare environments. AI with EHR/EMR systems will enable seamless data exchange across hospitals, pharmacies, labs, and remote care devices, improving both speed and accuracy in clinical workflows.
3. Smarter Voice-Enabled Clinical Workflows
Voice-powered documentation will become a core feature of Artificial Intelligence for EHR, reducing manual data entry. By integrating advanced voice recognition into AI EHR platforms, clinicians can capture patient notes quickly and accurately, minimizing errors and enhancing productivity.
4. Proactive AI Agents Will Support Clinicians
Future EMR AI systems will include intelligent healthcare agents that anticipate clinician needs. These assistants will proactively provide clinical suggestions, flag missing data, and automate repetitive tasks, further demonstrating the benefits of AI EHR in reducing cognitive load.
5. Seamless Multi-Department AI Coordination
Next-generation AI EMR systems will support real-time collaboration across departments like radiology, pathology, and cardiology. AI and EHR platforms will centralize insights, making it easier for specialists to access critical patient data instantly, improving interdisciplinary care.
6. Predictive Alerts Will Drive Preventative Care
The AI EHR of the future will offer instant, predictive alerts that help clinicians prevent complications before they arise. These proactive alerts will solidify the benefits of AI EHR in minimizing medical errors and improving patient safety.
7. Continuous Remote Care Through AI-Driven EMRs
EMR AI systems will strengthen remote patient care by continuously integrating real-time data from wearables and home monitoring devices. This will make AI in EMR a crucial tool in chronic disease management and post-discharge follow-up.
8. Smart Hospital Infrastructure Powered by AI and EHR
The future role of AI in Electronic Health Records will extend into smart hospitals, where AI in EHR systems will sync with IoT devices to manage beds, track equipment, and streamline emergency care, optimizing resource allocation and patient flow.
Why Appinventiv is the Right Partner to Develop AI in EHR/EMR Powered Solutions
At Appinventiv, we understand the complexities and opportunities that come with integrating AI in EHR/EMR systems. With our deep expertise in AI-powered healthcare solutions, we are uniquely positioned to help organizations navigate the complexities of AI adoption in their EHR systems.
Our team brings a wealth of experience working with top-tier healthcare providers, helping them transform patient care and streamline operations using cutting-edge AI technology. From predictive analytics and clinical decision support to seamless AI-powered documentation, we are ready to build AI-driven EMR solutions that meet your organization’s needs and exceed your expectations.
As a dedicated AI development services firm, here’s why we are the best choice for developing AI-powered EHR/EMR software:
- Expertise in AI Integration: With a proven track record in AI development, we specialize in integrating AI in EHR/EMR systems, enhancing clinical decision-making, and automating workflows.
- Healthcare Industry Knowledge: As a custom healthcare app development firm, we have extensive experience working with healthcare providers, understanding the unique challenges and regulatory requirements involved in AI adoption.
- Customized Solutions: We provide tailored AI-powered solutions for EHR systems, ensuring they align with your organization’s specific needs and improve overall operational efficiency.
- End-to-End Support: From strategy and design to implementation and ongoing support, we offer full-service assistance, ensuring a smooth AI integration process.
- Compliance and Security Focus: We prioritize HIPAA and GDPR compliance, ensuring that all AI-driven solutions adhere to the highest standards of data security and patient privacy.
- Scalability: Our solutions are designed to scale, allowing healthcare organizations to expand AI integration across departments and grow without compromising performance.
- Proven Results: Our clients have experienced tangible improvements in efficiency, reduced administrative burdens, and enhanced clinical outcomes after implementing AI in EMR systems with our solutions.
Get in touch with us to unlock the full potential of AI in your EHR/EMR systems and lead the future of healthcare innovation.
FAQs
Q. How to integrate AI into EHR?
A. Integrating AI in EHR systems involves several stages, beginning with a thorough assessment of your current system. The first step is to understand what challenges or inefficiencies exist in the existing EHR/EMR system that AI can address, such as automating administrative tasks or enhancing clinical decision support. Once this is clear, it’s essential to select the right AI-powered tools that can integrate seamlessly into your EHR systems.
Assess your current system: Understand the strengths and weaknesses of your existing EHR system.
Define the AI use cases: Choose specific applications such as predictive analytics or real-time decision support.
Select the right AI tools: Choose AI solutions for EMR systems that align with your current infrastructure and comply with regulations like HIPAA.
Q. How much does a custom AI EHR cost?
A. The cost of custom AI EHR systems can range between $50,000 to $500,000 or more, depending on the specific needs and scale of the organization. The variation in cost arises due to the level of complexity of the AI models, the integration requirements, and the healthcare organization’s size. Larger systems and more advanced tools, such as AI-powered clinical
Q. How does AI integration with EHRs improve patient care and operational efficiency?
A. AI integration with EHR systems significantly enhances both patient care and operational efficiency. AI-driven tools can streamline administrative tasks such as data entry and billing, which allows healthcare providers to focus more on direct patient care. Additionally, AI in EHR systems can provide real-time clinical decision support, improving diagnostic accuracy and enabling more personalized treatment plans.
AI-Powered Predictive Analytics: AI in EHR can analyze patient data to predict future health risks, allowing for proactive interventions.
Clinical Decision Support: AI in EMR tools help clinicians by providing evidence-based recommendations, aiding faster, more accurate decisions.
Automated Administrative Tasks: AI reduces clinician workload by automating tasks like documentation, billing, and scheduling.
Personalized Care: AI-powered solutions in EHR systems offer tailored treatment plans based on patient history and data, improving outcomes.
Q. How do we ensure HIPAA compliance while integrating AI with EHR data?
A. Ensuring HIPAA compliance during AI integration in EHR systems is critical for maintaining patient privacy and security. AI models processing sensitive patient data must adhere to the stringent requirements of HIPAA to avoid potential legal and financial repercussions. The integration should involve proper encryption, access controls, and regular audits to guarantee compliance.
Q. How does AI reduce clinician burnout when integrated with EMRs?
A. AI in EMR systems helps reduce clinician burnout by automating time-consuming tasks and providing decision support. This not only reduces the administrative workload but also helps clinicians make faster, more accurate decisions, enhancing their efficiency.
By reducing repetitive documentation tasks, AI allows healthcare providers to focus on patient care, which ultimately improves both their well-being and job satisfaction.
Q. What are the interoperability challenges when adding AI to an existing EHR infrastructure?
A. When integrating AI and EHR systems, interoperability can pose significant challenges, especially when dealing with legacy systems. AI models may require data formats that are incompatible with older EHR systems, hindering seamless data exchange.
Ensuring that AI tools work across diverse platforms and can process data from various sources is a complex task, especially when healthcare organizations rely on different technologies.
Data format compatibility: Legacy EHR systems may not support modern data standards like FHIR or HL7, creating challenges for integration.
System integration: Older systems might lack the necessary APIs to integrate with AI-driven EHR solutions and require middleware for smooth communication.
Real-time data exchange: Ensuring that AI models in EHR systems can pull real-time data from multiple healthcare systems for accurate decision-making.
Security and compliance: Ensuring that AI solutions comply with HIPAA when exchanging EHR data across different systems.


AI Agent-Driven UIs: Replacing App Menus and Buttons
Key takeaways: Challenge: Static menus and buttons also become outdated because people are frustrated by limited, multi-stage navigation. Solution: The AI Agent interacts with the user through a friendly UI that does not require cludgy menus but conversational and context-sensitive navigation. The Way AI Agents Work: AI agents establish a basis of natural language understanding,…

10 Use Cases and Benefits of How AI Agents Are Revolutionizing the Retail Industry
Key takeaways: AI agents in the retail industry are revolutionizing businesses by enhancing customer experience and streamlining operations. From personalized recommendations to predictive analytics, AI offers tangible benefits like increased conversions and reduced costs. AI adoption can lead to scalable growth and a competitive edge in the retail industry. Retailers must consider data strategies, talent…

12 Ways AI is Revolutionizing the Fashion Industry
Key takeaways: AI in fashion is booming, with a market value of $28.48 billion by 2032 and a 39.43% CAGR. It's transforming design, trends, shopping, manufacturing, and customer service. Top brands like Zara and H&M report 200% higher conversions, 64% fewer returns, and 25% better retention. Success demands strategy, data infrastructure, and phased AI integration…


















